Insomnia and sleep problems are pervasive in our culture, but did you know that women are more likely to experience poor sleep than men? The changes in female hormones through the menstrual cycle influence sleep patterns and may explain why sleep becomes more challenging for many women before or during their period.
Moreover, those with premenstrual syndrome (PMS) or premenstrual dysphoric disorder (PMDD) may be even more likely to experience PMS insomnia, fragmented sleep, and reduced sleep quality due to changes in hormone levels.
Today’s article will unpack the connections between the menstrual cycle, hormone health, and sleep. Plus, I’ll offer tips for improving sleep quality before and during your period.
In this article:
Your Menstrual Cycle – Explained
Let’s start with a review of the stages of the menstrual cycle and how a healthy menstrual cycle looks. For a deeper understanding of this topic, please read Phases of the Menstrual Cycle and How the Menstrual Cycle Works.
What are the 4 Stages of The Menstrual Cycle?
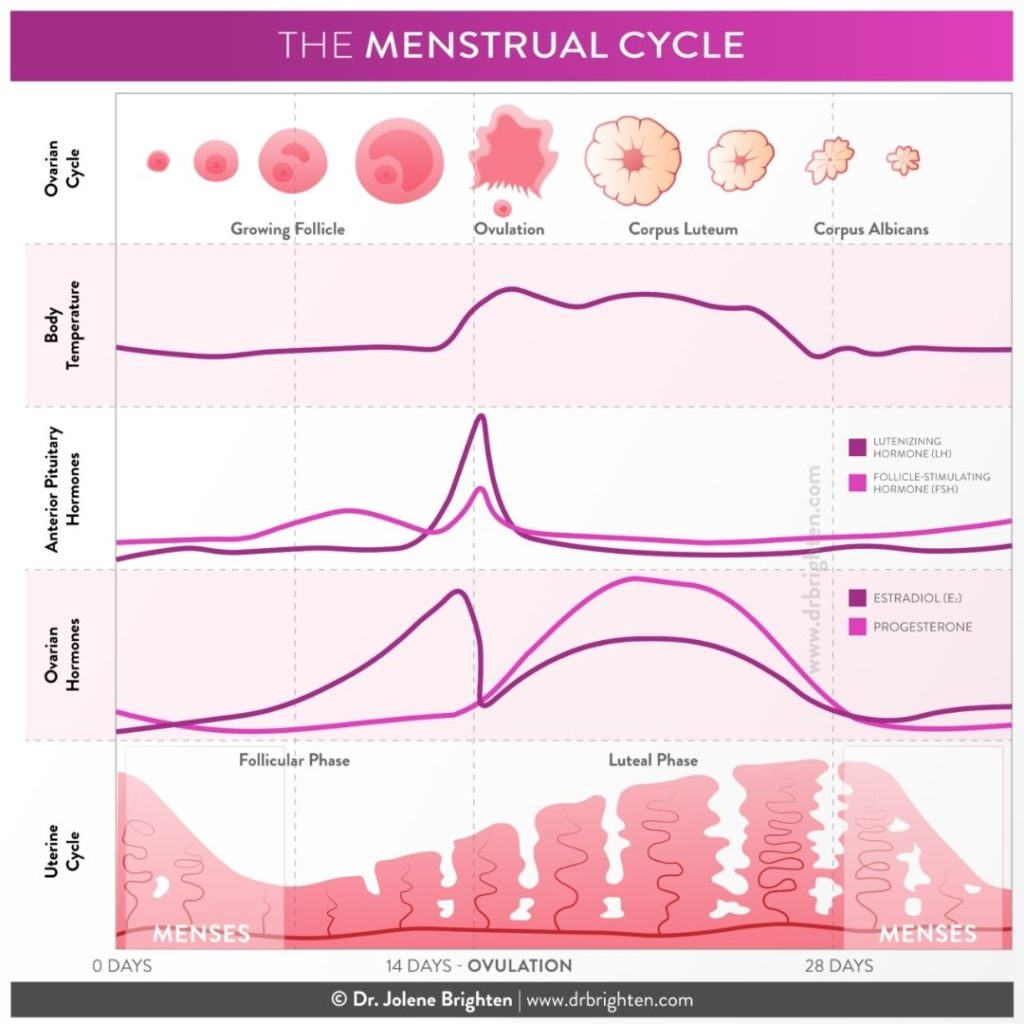
The menstrual cycle encompasses the monthly cyclical hormonal changes women experience between puberty and menopause. The menstrual cycle is how the body prepares for a possible pregnancy and is also an overall marker or vital sign of health.
The menstrual cycle is divided into four stages:
- Menstrual Phase – The menstrual phase begins on the first day of period flow, which we call Day 1 of the menstrual cycle. During menstruation, the body sheds the endometrial lining (uterine lining). Estrogen and progesterone levels are low.
- Follicular Phase – The follicular phase encompasses the menstrual phase. It begins on Day 1 and goes until ovulation, typically around two weeks. Estrogen and follicle stimulating hormone (FSH) rise. Estrogen builds the endometrial lining and supports healthy cervical fluid.
- Ovulation Phase – Estrogen and luteinizing hormone (LH) spike, and the mature egg is released in ovulation. This phase lasts around 24 hours from the time the egg is released.
- Luteal Phase – The luteal phase occurs after ovulation until your next period begins and the cycle starts again. During this phase, progesterone levels rise. This phase lasts around two weeks.
Hormone Fluctuations During Your Period and Sleep
Hormones fluctuate throughout the menstrual cycle, affecting the circadian rhythm and sleep. Since all hormone systems are connected, the effects go beyond sex hormones. For example, estrogen and progesterone affect other hormones, including thyroid hormones and adrenal hormones, such as cortisol.
When imbalances in female hormones occur, it may affect your menstrual cycle, contributing to period-related symptoms. Conversely, hormone levels are affected when sleep is poor, or you’re putting in too many late nights.
So, establishing regular sleep patterns is good for your hormones and supporting hormone health is good for your sleep.
Let’s look at some of the specific connections.
PMS And Sleep
Can PMS affect sleep? There is a connection between PMS and sleep. Many women report
sleep problems before their periods correlate with premenstrual syndrome symptoms or changes in physical or emotional health leading up to their period.
It’s estimated that 75% of women will experience some PMS symptoms.
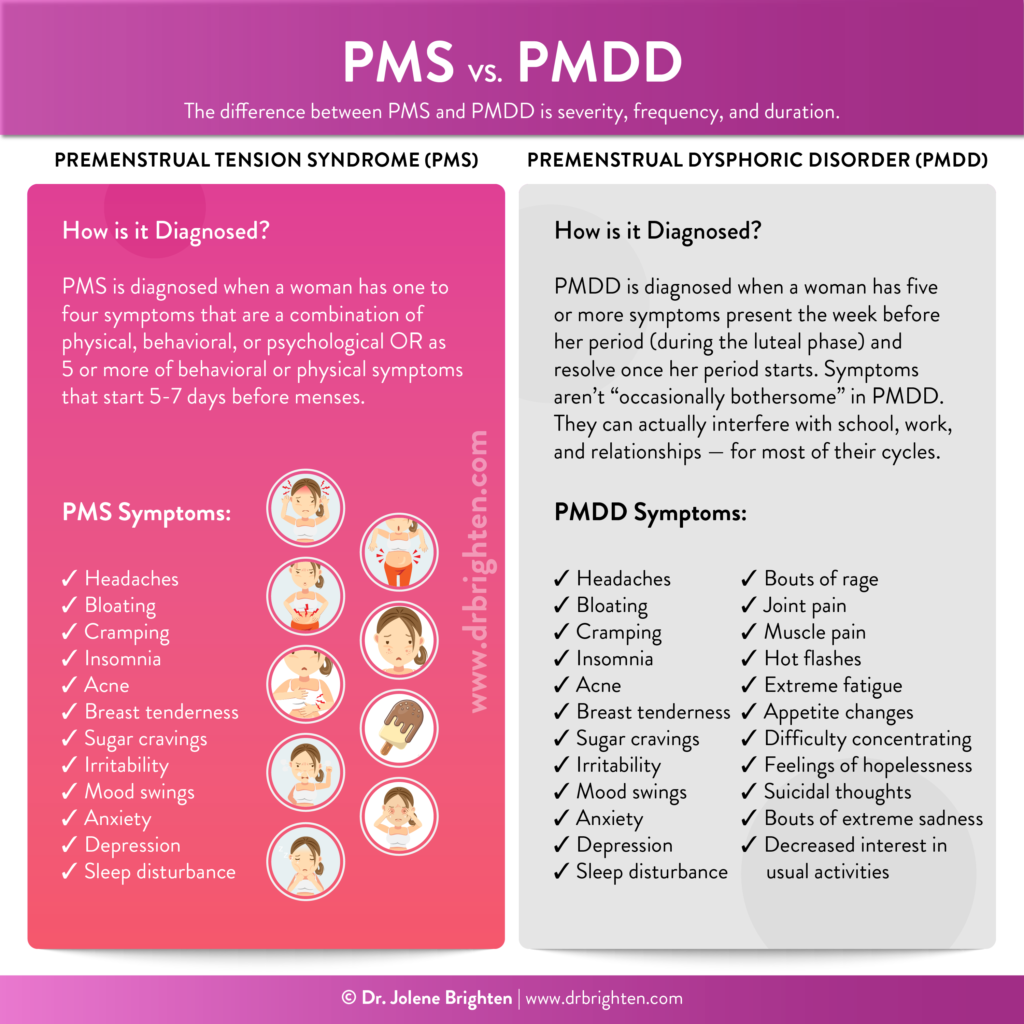
What Is PMS?
PMS is related to hormone shifts during the luteal phase of the cycle leading to physical and psychological symptoms that resolve with menstruation. Often women who experience PMS have estrogen dominance with relative excess estrogen levels due to low progesterone.
Symptoms of PMS may include:
- Bloating and fluid retention
- Digestion changes such as constipation or loose stools
- Breast tenderness
- Uterine cramping
- Headaches and migraine
- Brain fog and poor concentration
- Fatigue
- Anxiety, irritability, depression, mood swings
- Increased hunger and cravings
- Decreased libido
- Acne
- Joint pain
- Changes in sleep patterns and insomnia
What Is PMDD?
Premenstrual dysphoric disorder, or PMDD, is more extreme than PMS and much less common, affecting 3-8% of women in the luteal phase of their cycle. PMDD often lasts longer than PMS, 10-14 days, compared to five to seven days for PMS. PMDD can be debilitating, affecting work, relationships, and quality of life.
In addition to the cluster of PMS symptoms listed above, PMDD symptoms may also include:
- Feelings of hopelessness
- Suicidal thoughts
- Sadness
- Depression
- Rage
- Decreased interest in life activities
Can PMS and PMDD Affect Sleep?
Women with PMS and PMDD are more likely to experience sleep problems, especially during the late luteal phase leading up to the period. In the research, sleep disturbance is characterized as subjective and self-reported, and not always substantiated by data collected during sleep studies.
Women report sleep disturbances with PMS and PMDD that include:
- Harder time falling asleep
- Frequent nighttime awakenings (sleep fragmentation)
- Not feeling rested or restored after sleep
Poor sleep leads to daytime symptoms of fatigue, sleepiness, reduced concentration, and decreased performance.
Regardless of premenstrual diagnoses, sleep architecture changes during the menstrual cycle. In the luteal phase, stage N2 non-REM (non-rapid eye movement) sleep, or deep sleep, increases compared to the follicular phase. In addition, REM sleep decreases during the luteal phase.
Women with PMS and PMDD may experience more extreme changes in sleep patterns due to hormonal changes and symptoms experienced.
Sleep, Progesterone, and Melatonin
Progesterone and body temperature influence sleep. As progesterone levels rise in the luteal phase, you may experience an increase in body temperature. Therefore, monitoring basal body temperature confirms ovulation and is used in fertility awareness methods. These body temperature changes are also associated with sleep fragmentation.
In addition, the metabolism of progesterone may play a role. One of the metabolites progesterone breaks down to is called allopregnanolone. When there are decreased levels of this metabolite, sleep disturbance may occur.
This pattern may be exaggerated in women with PMDD, where impaired GABA response to fluctuations in allopregnanolone correlate to mood disturbance, poor stress tolerance, and sleep disturbance. GABA is the nervous system’s primary inhibitory neurotransmitter that helps us to feel calm, relaxed, and supports sleep when levels are optimal for each person.
Melatonin is a hormone involved in the regulation of circadian rhythms that naturally rises at night to promote drowsiness and sleep. Women with PMDD may have a decreased response to melatonin production in the luteal phase compared to the follicular phase, suggesting another mechanism for sleep disruption.
Improving Sleep Quality During Your Period
So far, we’ve focused on how PMS and PMDD correlate with decreased sleep quality in the luteal phase. Sleep can also be disturbed during the menstrual phase. During your period, hormones are at their lowest level. Sleep may be more difficult for some women without progesterone in the follicular phase, especially when estrogen is slow to rise.
Additionally, the feeling of needing to wake and attend to your period by changing a pad or tampon may disrupt sleep or make it harder to get back to sleep. (Periods that are so heavy that you have to very frequently change a pad or tampon could be a sign of menorrhagia.)
When you know your patterns and how your menstrual cycle affects sleep, you can make positive changes to improve sleep. Many lifestyle tools and supplements counteract changes in sleep patterns and provide additional support during the times of your cycle when you need it most.
Let’s take a look at some interventions to consider.
Practice Good Sleep Hygiene
First and foremost, good sleep hygiene is vital. If you have bad sleep habits, sleep will be harder, especially before and during your period. Here are some easy habits to implement:
- Set a regular bedtime, and stick to it.
- Create a relaxing bedtime routine. Drink herbal tea, read, journal, take a bath, or practice other self-care to help you wind down.
- Limit screens before bed. The blue light emitted from screens suppresses melatonin production.
- Limit stress before bed. Set a curfew for social media and checking email. It can wait until tomorrow.
- Make sure your bedroom is cool and dark to promote sleep.
- Wear comfortable, breathable pajamas to help you regulate your body temperature.
- Consider gentle, supplemental support to help with sleep. Find the 10 best sleep supplements here.
Hormone Support Supplements
In addition to practicing healthy lifestyle habits, including good sleep hygiene, supplements that support underlying hormonal patterns may help improve sleep. In the case of PMS or PMDD, supplements and other interventions may support healthy progesterone and estrogen levels and could decrease symptoms over time.
Another factor that influences sleep is stress. Supplements are a supportive tool for adrenal health that, in turn, help to improve sleep.
Let’s look at some of these hormone support supplements.
Support a Healthy Menstrual Cycle
If you notice a correlation between your period and insomnia, you are not alone. As discussed, sleep disruptions can be a symptom of hormone fluctuations, PMS, and PMDD. Often, sleep problems are just one of many changes you notice in how you feel leading up to and during your period.
Supplements can be immensely supportive for supporting hormonal balance that leads to optimal sleep. Please read Supplements for PMS to learn more about B vitamins, magnesium, DIM, turmeric, and other supportive root-cause supplements.
Dr. Brighten Balance Women’s Hormone Support contains many key nutrients and herbal extracts that support a healthy cycle and hormone balance.
Importance of Adrenal Hormone Support and How to Balance Stress Hormones
HPA-axis dysfunction, commonly referred to as adrenal fatigue, may produce an imbalance in cortisol levels that affect sleep.
Cortisol follows a regular daily pattern where it is high in the morning, so you feel alert and energized, and it gets lower in the evening to promote sleep. It has the opposite pattern as melatonin.
If cortisol is high, low, or follows a different pattern, you might feel tired yet wired and anxious at night and have a hard time falling asleep or wake in the night with your mind racing.
The solution is first and foremost to reduce stress; however, while you are working on this piece adaptogenic herbs like those found in Dr. Brighten Adrenal Calm. This formula is a blend of effective adaptogenic herbs and nutrients that supports the body’s natural decline in evening cortisol levels to promote restful sleep.
A side effect of adrenal support is a healthy menstrual cycle and better sleep.
Key Takeaways
- Sleep problems often correlate to phases of the menstrual cycle, primarily the luteal and menstrual phases.
- Hormone fluctuations may trigger changes in sleep patterns, especially in those with PMS or PMDD.
- Changes in progesterone and melatonin help explain why sleep problems are more likely at certain times in the menstrual cycle or with PMS and PMDD.
- Supporting adrenal and sex hormone balance may improve the menstrual cycle and sleep.
- An effective strategy for addressing the hormones that influence sleep is lifestyle change, plus targeted supplements such as Adrenal Calm.
- Be sure to work with your doctor when choosing hormone support supplements, especially if you take medication, have a medical condition, are pregnant, or nursing.
Wishing you more ease with your menstrual cycle and the better sleep it brings!

