Did you know there are several phases of the menstrual cycle and a whole lot more going on than just your period? That's right. There is a symphony of hormones playing throughout your cycle, which can explain why we feel different throughout the month.
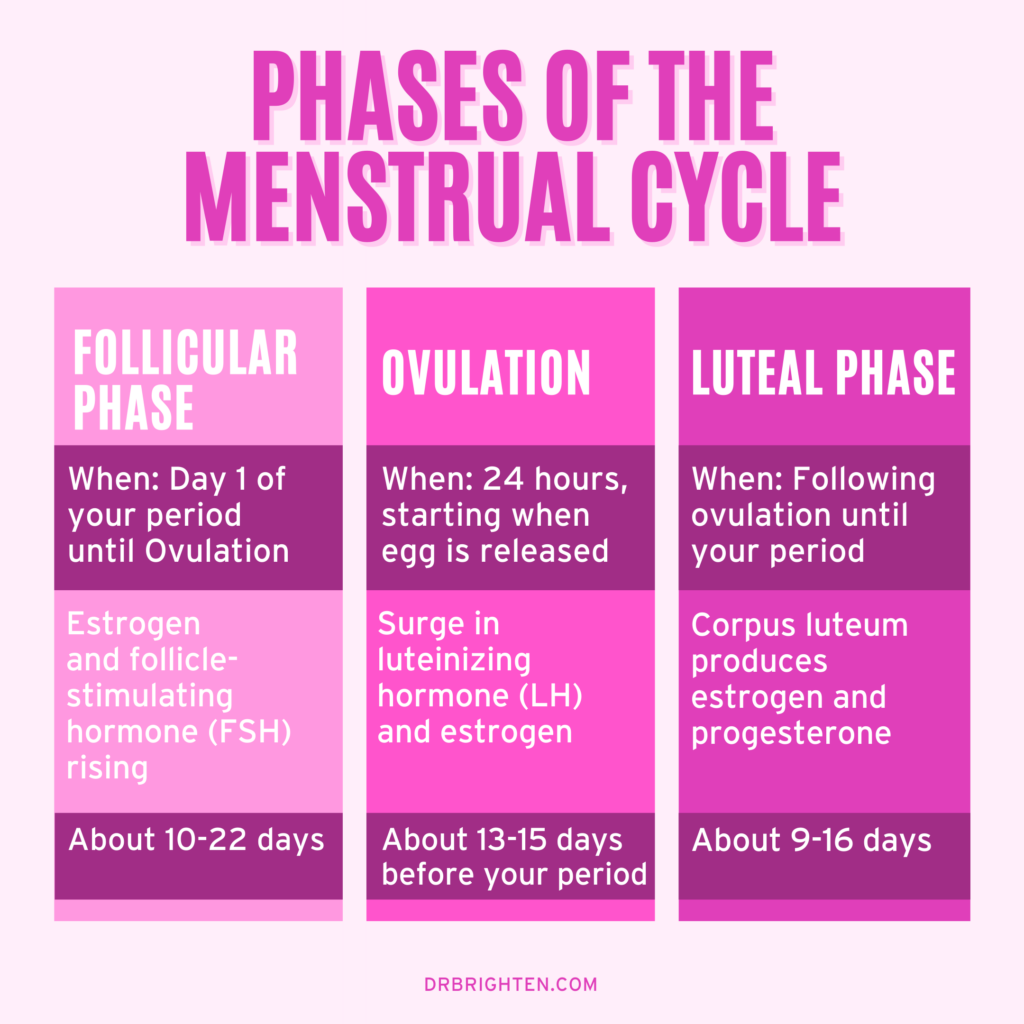
In medicine, there are three phases of the menstrual cycle: the follicular phase, the ovulatory phase, and the luteal phase. You may have heard that menstruation or your period is its own phase, but this isn't totally accurate when we’re talking about hormone physiology and ovarian function.
There is nothing wrong with talking about your cycle as four distinct phases. In this article, I’m going to walk you through a natural menstrual cycle (i.e. a normal cycle that isn’t manipulated by hormonal birth control) and further information on how the menstrual cycle works. I'm also going to toss some medical jargon your way so you can have a more informed discussion when you talk with your doctor.
In chapter 2 of my book Beyond the Pill, I take a deep dive into helping you understand your menstrual cycle, your period, and your period problems (what they mean, and how you can balance your hormones to minimize PMS, heavy bleeding, or other period problems). If you want to go deeper on this topic, I’d recommend leveraging that resource.
In this article:
What Are the Three Phases of the Menstrual Cycle?
The 3 phases of the menstrual cycle include (in this order):
- Follicular Phase
- Ovulatory Phase
- Luteal Phase
Let’s break it down a bit more and give you some definitions.
Detailed Phases of the Menstrual Cycle
- Menstruation. During menstruation, your body sheds the endometrial lining and estrogen and progesterone are at their lowest point. This is your period, the most noticeable phase in your menstrual cycle because you’re bleeding.
- Proliferative Phase. When your period ends and you begin to rebuild the uterine lining.
- Follicular Phase. First day of your period until ovulation. Estrogen and FSH rise in preparation for ovulation.
- Ovulation Phase. The release of an egg. LH and Estrogen spike, which triggers the release of the egg.
- Luteal Phase. The luteal phase starts after ovulation and lasts through your next period. During the luteal phase, you produce higher levels of progesterone.
- Secretory Phase. The secretory phase is when the uterus produces chemicals to prepare for the implantation of a fertilized egg.
Hormones of the Menstrual Cycle
The main hormones of the menstrual cycle include:
- Follicle Stimulating Hormone (FSH)
- Luteinizing Hormone (LH)
- Estrogen
- Testosterone
- Progesterone
Each hormone rises and falls at different times in your cycle. Here’s some detail on what each one does.
Follicle Stimulating Hormone (FSH)
Follicle Stimulating Hormone is a brain hormone that is secreted by the pituitary gland. FSH stimulates the ovaries to prepare for ovulation.
Luteinizing Hormone (LH)
Secreted by the pituitary gland, Luteinizing Hormone triggers the release of an egg during ovulation.
Estrogen
Estrogen is the predominant hormone in the follicular phase that encourages ovulation and the development of the endometrium.
Testosterone
You may think of testosterone as a male hormone, but women need a small amount. And when we don’t have it, we feel it. Testosterone is an androgen that supports immune health, libido, and is necessary for a healthy menstrual cycle.
Progesterone
Progesterone is the predominant hormone of the luteal phase that prepares the endometrial lining for ovulation.
Uterine Phases of the Menstrual Cycle
The uterus has three phases: the period, proliferative and secretory phase. Within the follicular phase (pre-ovulation) there is the period and proliferative phase. Following ovulation there is the secretory phase, which is part of the luteal phase.

Follicular Phase of the Menstrual Cycle
The follicular phase is when you have your period through ovulation. But wait, why isn’t my period it’s own phase?
Your period aka menstruation is a time when your uterus sheds the lining it had built up from your last cycle. But even while your uterus is bleeding, your brain and ovaries have a different agenda.
The focus on the menstrual cycle is ovulation. Or in other words, your body is working on preparing you for pregnancy.
Even while you have your period, FSH is rising, follicles are developing and your ovaries are preparing for ovulation.
The Uterus During the Follicular Phase
Your period is the beginning of the follicular phase.
Day one of your menstrual cycle is the first day that you see blood — the first day of your period. The follicular phase is going to last approximately from day one until ovulation occurs. Contrary to popular belief, we don’t all ovulate on day 141.
Your period is triggered by a drop in your hormones that is the result of the egg not being fertilized. This causes your endometrial lining (the lining of your uterus) to shed.
The Ovaries During the Follicular Phase
The main goal of the follicular phase is getting an egg ready for ovulation. While you have your period, your pituitary (a gland in the brain) secretes follicle-stimulating hormone (FSH). FSH tells your ovaries that it's time to get a follicle ready and that estrogen needs to increase as well to get your body prepared for a baby.
During the follicular phase, estrogen is your main diva. Your lips might look a little plumper, and fewer fine lines2 and wrinkles are visible because of rising estrogen levels. It's also hard at work protecting the heart and modulating the immune system.
Estrogen is also rising and to get the endometrium ready (see the proliferative phase below).
Testosterone begins to rise in the latter half of the follicular phase prior to ovulation.
When your libido spikes, that's usually a good indication that ovulation is coming. As a cyclical creature, you don't have a libido all day, every day. It's normal for women to be in the mood one week and less in the mood the next — your libido is your libido.
The Uterus During the Proliferative Phase
The proliferative phase begins when your period stops. During this phase, estrogen (secreted by the ovaries) stimulates the growth of the uterine lining. Yes, the very lining you just finished shedding is being rebuilt.
The uterine lining will continue to grow through the luteal phase (secretory phase). It does this to prepare for the implantation of a fertilized egg. If the egg is not fertilized, your period will begin again.
Ovulatory Phase of the Menstrual Cycle
During the entire follicular phase your ovaries have been working to prepare an egg for ovulation. The dominant follicle is now ready as you enter the ovulatory phase. Estrogen levels will spike, triggering the pituitary to release luteinizing hormone (LH). The surge in LH will result in the release of the mature egg. You're officially in the ovulatory phase for 24 hours.
Ovulation typically occurs 13-15 days prior to your next period.
It’s important to note that if you are in your fertile years — whether or not you want to have a baby — you want to ovulate. This is because when you ovulate, a structure (called the corpus luteum) is left behind in your ovaries, and it is crucial for the luteal phase.
Luteal Phase of the Menstrual Cycle
After ovulation, you enter the luteal phase of your cycle. This phase will last from the ovulation until the beginning of your next menstrual period. The corpus luteum, a temporary endocrine structure left behind from ovulation, begins to secrete progesterone, as well as estrogen during this phase.
Progesterone will peak about 5-7 days after ovulation, which is the most appropriate time to test for it in your cycle. When progesterone levels are optimized you should have no trouble sleeping, feel a sense of calm, and experience minimal PMS symptoms. If you do experience PMS, it may be a sign your progesterone is low. Read more about how to manage PMS here.
A very short cycle could also indicate low progesterone. So if, for example, you don’t ovulate and your periods are coming less than every 21 days, that's a sign that you don't have enough progesterone. This article lists some other signs of low progesterone.
The Uterus in the Secretory Phase
From ovulation to your next period, the uterus will secrete chemicals to support implantation if fertilization occurs or to support the endometrial lining in shedding should you not become pregnant.
Progesterone rising will halt the growth of the endometrial lining, which prevents endometrial hyperplasia. Prostaglandins, hormone-like chemicals, will be released from the uterine lining during this phase. It is the secretions of these chemicals by the uterus that gives this phase its name.
If pregnancy occurs, these prostaglandins will be suppressed to keep the uterine lining intact and prevent cramping. In the event the egg is not fertilized, these prostaglandins (specifically PGE2 and PGF2α) will stimulate the contraction of the uterus and the corpus luteum will stop secreting estrogen and progesterone. The combination of the shifts in these hormones, along with the increase in prostaglandins, causes the endometrial lining to break down—resulting in your period.
How Long Is A Menstrual Cycle?
On average, we think of the menstrual cycle as being a 28-day event. From the first day you see blood until the next period is, on average, 28 days. But not every woman3 is on a 28-day cycle. Women with PCOS tend to have longer cycles. Women in perimenopause may have shorter cycles.
Is there anything wrong with shorter or longer cycles? Regular is the key, but if you experience cycles less than 21 days or longer than 35 days, then there may be an issue.
Tracking Your Cycle
The American College of Obstetricians and Gynecologists (ACOG) termed the menstrual cycle the fifth vital sign. That means that the patterns of your period and your menstrual cycle have incredible data that doctors can use to evaluate your health.
Knowing when your period starts, how many days between periods, and how long your period lasts can help you and your provider understand if there are any issues that need to be addressed.
Some other questions to ask yourself are:
- How do I feel when I'm on my period?
- How do I feel leading up to ovulation?
- How do I feel when I ovulate?
- How do I feel after ovulation?
- How do I feel in the week before my period? (Am I pooping? Is my skin breaking out? Am I having mood swings? Is my sleep disrupted?)
If you understand those symptoms, you can dial in what's going on. There are many ways to track your cycle. You could use a journal or calendar, download apps (like AskTia), and use femtech devices like Natural Cycles. It's simply a question of what works best for you.
References
- https://www.sciencedirect.com/science/article/abs/pii/S0884217515343768 ↩︎
- https://onlinelibrary.wiley.com/doi/abs/10.1111/jocd.12508 ↩︎
- https://www.sciencedirect.com/science/article/abs/pii/S0010782404001313 ↩︎
