Premenstrual Dysphoric Disorder (PMDD) is a condition that impacts women about 2-3 weeks out of every month. Symptoms can be mental, emotional, as well as physical. In this guide to treating PMDD we'll cover conventional treatments, as well as 12 natural treatments for PMDD to consider.
Many women are familiar with premenstrual syndrome (PMS). By some estimates, 85% of us experience it.
Moodiness, anxiety, bloating, crying for no reason, polishing off a pint of ice cream before you even realize it … yes, sometimes being a woman with hormonal imbalances can be so much fun.
If you’re one of the 3-8% of women who experience PMDD, PMS can take on a whole other dimension. Your symptoms may be more severe. Your cycles are absolute torture — especially 10-14 days before your period when extreme PMS takes hold of your life.
It’s called premenstrual dysphoric disorder (PMDD).
And for many sufferers, it’s a debilitating disorder that affects their career, relationships, and overall health. One study estimated that women suffering from PMDD actually lose three years of their lives due to the misery they experience on a regular basis.
It’s also one of those conditions that’s routinely dismissed and often overlooked by the traditional medical community (as with so many issues related to female health). Sigh.
By some estimates, up to 8% of women experience PMDD, and 20% experience “sub-threshold” PMDD — meaning severe PMS. Many deal with it over the course of decades, struggling to find a diagnosis and are often left wondering what the heck is wrong with them. Traditional lab testing often indicates that their hormone levels are “normal” — furthering the frustration and dismissal of their concerns.
But it is important to note that there’s a difference in optimal ranges and normal ranges. In addition, PMDD is often thought of as an abnormal response to normal hormonal changes. In this guide to treating PMDD we’ll explore more about testing, hormone balancing, and natural treatment strategies for PMDD.
As a women's health naturopathic physician, I have worked with many women who have been able to overcome their PMDD symptoms using the strategies I'm sharing in this guide to treating PMDD.
In this article:
- What is PMDD?
- Who is at risk for PMDD?
- What causes PMDD?
- PMDD and Estrogen
- PMDD vs. PMS — What’s the Difference?
- Is There a Test for PMDD?
- Can the pill trigger PMDD in some women?
- Is PMDD considered a mental illness?
- Do PMDD symptoms get worse with age?
- How is PMDD treated? Guide to PMDD Treatment
- What medications are used to treat PMDD?
- 12 Natural Treatments for PMDD
- Share the Guide to Treating PMDD
- References
What is PMDD?
PMDD is basically feels like PMS on steroids. Or in other words, imagine the worse symptoms of PMS intensified and for much longer out of the month.
PMDD is a severe cluster of symptoms that starts prior to a woman’s period (usually 10-14 days rather than the typical 5-7 days for PMS).
PMDD Symptoms:
PMDD symptoms may include any combination of the following:
- Headaches
- Bouts of rage
- Mood swings
- Depression
- Joint pain
- Muscle pain
- Hot flashes
- Insomnia
- Extreme fatigue
- Appetite changes
- Anxiety
- Irritability
- Difficulty concentrating
- Cramps
- Bloating
- Breast tenderness
- Feelings of hopelessness
- Suicidal thoughts
- Bouts of extreme sadness
- Decreased interest in usual activities
Typically, these symptoms disappear once a woman’s period starts or shortly thereafter.
Who is at risk for PMDD?
Your brain is full of receptors for sex hormones. This means your natural sex hormones, synthetic ones found in birth control, and perhaps even environmental xenoestrogens (compounds that mimic estrogens) have the ability to influence brain function and mood.
While there is some genetics involved in the development of PMDD, I want you to know that genes aren’t the end of the story. Your environment and the practices you choose can influence your genetic expression and the presence or absence of disease.
We have also come to understand that women who have a past history of trauma or sexual abuse are under a great deal of stress are at an increased risk.
In addition, being overweight also raises the risk. This may be because adipose tissue (fat cells) act as an endocrine organ and can produce estrogen. In addition, increased adiposity can be associated with increased inflammation, which would also influence symptoms. However, don’t let your doctor dismiss you with the archaic “just eat right, exercise, lose weight and you’ll be fine” narrative. It’s not that simple. And you’re not to blame for these symptoms.
What causes PMDD?
PMDD is an abnormal reaction to the fluctuations in hormonal changes that take place during a woman’s monthly cycle.
Recent studies have shown that women with PMDD actually have a genetic sensitivity to estrogen and progesterone which triggers extreme reactions. Sometimes it’s nice to have your experience validated by research, isn’t it?
Even the doctor who announced the findings, David Goldman, M.D., acknowledged “This is a big moment for women’s health, because it establishes that women with PMDD have an intrinsic difference in their molecular apparatus for response to sex hormones – not just emotional behaviors they should be able to voluntarily control.”
While it’s sad to think in this day and age much of society is still operating under the delusion that PMS and PMDD are things women can just voluntarily control — it is a huge step forward to have science admit that there’s a biological component to the symptoms we can suffer through on a monthly basis.
PMDD and Estrogen
In addition to the genetic component, just like PMS, PMDD can also be characteristic of estrogen dominance.
While we just love estrogen for its role in giving us breasts, hips, and thighs — we don’t always love the consequences of too much of it building up in our systems.
And while we certainly don’t need a team of researchers to tell us that estrogen can mess with our emotions — sometimes it feels good to have the scientific method validate what we already know to be true.
Sometimes, excess estrogen can build up in our systems due to the liver not processing estrogen properly or the gut not eliminating it effectively.
The best ways to ensure estrogen is dealt with efficiently by your body are to support your liver, adrenals, and digestive system.
A hormone friendly diet that includes lots of vegetables, fruits and fiber can go a long way to help improve symptoms of estrogen dominance. I’ve put together a free meal plan to help point you in the right direction for this.
And my Period Problems Kit™ can do wonders for giving the liver, adrenals, and gut a helping hand in processing estrogen and improving PMS and PMDD symptoms.

PMDD vs. PMS — What’s the Difference?
Some of you are probably reading the list of symptoms and thinking, “Wait, I’ve had all of those at one time or another — do I have PMDD?”
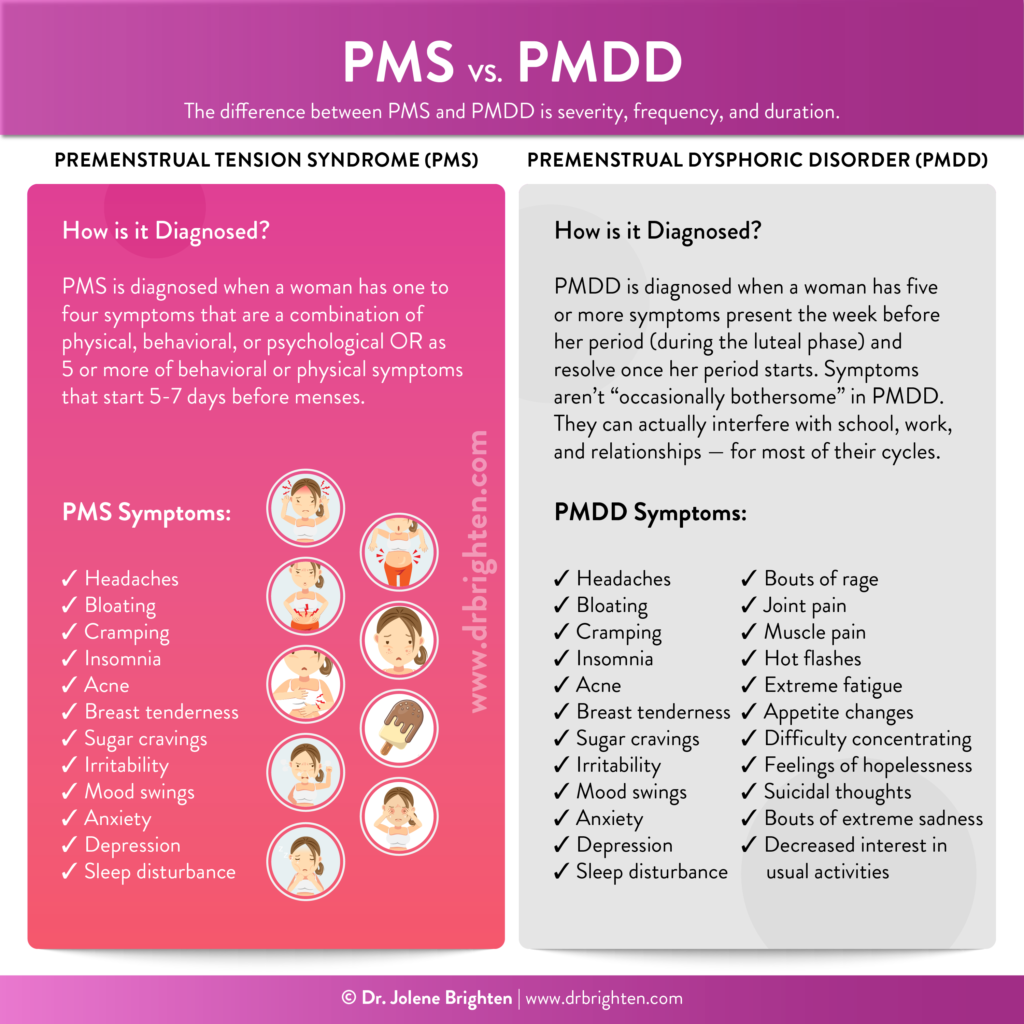
The difference between PMS and PMDD is severity, frequency, and duration.
While PMS sufferers may experience occasional cravings or a mood swing here or there, women with PMDD have headaches, extreme fatigue, serious breast tenderness, massive bloating, and even fits of full-on rage they can’t control or suicidal thoughts. You can read up more on PMS and the best supplements for it here.
We’re talking symptoms that can actually interfere with school, work, and relationships — for most of their cycles. The symptoms can start as much as two weeks before their period. With PMS, symptoms usually start 5-7 days before menses.
If you suspect your PMS is actually PMDD, start taking note of your symptoms and when they occur on your period tracking app or calendar. This will help you determine more easily which camp you fall into and will give your doc plenty of good data to analyze.
How Is PMS Diagnosed?
After other conditions have been ruled out, PMS is diagnosed when a woman has:
- One to four symptoms that are a combination of physical, behavioral, or psychological OR
- Has 5 or more of behavioral or physical symptoms
Per the American College of Obstetricians and Gynecologist guidelines, symptoms must be present at least 5 days before menses (during the luteal phase), disrupt daily living, and resolve within four days of starting your period. These symptoms need to be present for at least 3 months.
How is PMDD Diagnosed?
The diagnosis of PMDD is made using the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5). Documenting symptoms is a must as they are what determine the diagnosis and they need to be present most of the year.
From the list of symptoms, five or more need to be present the week before your period (during the luteal phase) and resolve once your period starts. Before you dive into this list and self diagnose, understand that this symptoms aren’t “occasionally bothersome” in PMDD. They are downright disruptive, hijack your life, sabotage relationships, and make it really difficult to function.
One or more mood symptoms must be present:
- Anger, irritability
- Mood swings, sudden sadness
- Depressed mood, feeling hopeless, negative/ self-critical thoughts
- Anxiety, tension, feeling on the edge
One or more symptoms from this list to reach a total of five:
- Cravings, overeating, change in appetite
- Brain fog or difficulty concentrating
- Decreased energy or easily fatigued
- Physical symptoms like breast tenderness or swelling, joint pain, muscle pain, bloat, or weight gain
- Insomnia or sleeping in excess
- Lack of interest in usual activities
- General sense of overwhelm or lack of control
These symptoms could indicate other health conditions, so your doctor should fully evaluate them to rule out other causes. Additionally, symptoms must also be present for most cycles per year, and must also be debilitating enough to cause functional difficulties in your life. As in, your symptoms must affect your work, relationships, life, or physical abilities to be considered PMDD.
So, for example – if, at a predictable time almost every month, your symptoms are causing you to miss work, rage at your spouse, affect your ability to think clearly enough to function at your job, or you have trouble getting out of bed, you may want to ask your doctor about PMDD.
Is There a Test for PMDD?
There is no lab test for PMDD. The diagnosis is made based off your symptom history.
Although there is no lab to diagnose PMDD, additional lab testing should be done in order to rule out other conditions.
Sex Hormones
Testing estrogen and progesterone on day 19-22 or about 5-7 days after ovulation can help you understand if you’re making enough progesterone or if you have excess estrogen, which can be a driving factor in your symptoms.
Complete Thyroid Panel
Hypothyroidism and hyperthyroidism should be ruled out as a possible cause of symptoms. You can read about thyroid lab testing here.
Thyroid dysfunction is associated with mood symptoms like depression and anxiety. In addition, women with these conditions can experience insomnia, irregular periods, fatigue, headaches, joint pain, brain fog and more
Adrenal Function Test
HPA dysregulation can be another culprit, as can Cushing’s Syndrome (too much cortisol) and Addison’s Disease (too little cortisol). I wrote about how your adrenal hormones can be driving symptoms here.
Having a morning ACTH and cortisol blood test can provide some useful data with regards to ruling out disease. If you’re looking into dysfunction and optimization, you’ll want a 4 point urinary or salivary test like I talk about in Beyond the Pill.
Blood Sugar Tests
Checking into blood sugar health is a good idea for every woman. A fasting insulin, HgA1C, and fasting glucose can help your doctor determine if your symptoms are related to you blood sugar.
This can account for symptoms of fatigue, cravings, weight gain, inability to concentrate, sleep disturbance, anger, irritability, mood swings, and anxiety.
Can the pill trigger PMDD in some women?
It’s been shown that use of the birth control pill is associated with depression in some women. And anyone who’s gone on the birth control pill to “regulate PMS” only to find their symptoms go completely off the charts will tell you that yes, the pill can trigger PMDD.
There’s a mountain of anecdotal evidence, and believe me, I’ve seen plenty of women in my office that have suffered from extreme PMS after going on the pill. Sometimes, the pill can work to reduce symptoms in the short term and then cause major PMS flare-up later down the road.
Sadly, the experiences of these women are often dismissed by the traditional medical community, and they are forced to search for their own answers.
If you’re having trouble adjusting to the pill you’ve been prescribed, I can help support you in your journey to survive on hormonal contraception. In my book, Beyond the Pill, I talk about ways to recognize and treat different hormonal imbalances that often result from the use of the pill. If you haven’t checked it out yet, and especially if you suspect you’re suffering from PMDD, I encourage you to give it a read.
And for other women, the pill and other forms of hormonal birth control can help symptoms. More on that soon!
If you do decide to use birth control, I highly recommend that you check out this extensive article I wrote on reducing the side effects of the pill. It’s chock full of great information to help you navigate the ups and downs of finding hormonal balance while taking oral contraceptives.
Is PMDD considered a mental illness?
Difficulties regulating emotions and mood disturbances like depression and anxiety can be defining characteristics of PMDD. And researchers have found connections between serotonin levels and women with PMDD. PMDD is also commonly found along with other mental illnesses like bipolar disorder.
For these reasons, in 2013, PMDD was added to the Diagnostic and Statistical Manual of Mental Disorders (known as the DSM-5). The DSM-5 is the comprehensive list used by licensed mental health practitioners and physicians to diagnose mental health conditions.
Adding this disorder to the DSM-5 legitimized what many of us already acknowledged as true — that PMDD is a diagnosis that can’t be dismissed.
PMDD is also classified as an endocrinological disorder and can be diagnosed as such. So if you have easy access to either your endocrinologist or psychiatrist, you can get a diagnosis.
Mental Health Support Is Vital with PMDD
I can’t stress enough how important it is for women with PMDD to seek solid mental health support. Ask your doctor to refer you to appropriate counseling or support groups of women going through the same thing.
Guided mental health support will help you develop healthy coping skills, work on safety plans as needed, and develop support networks. Working with a therapist can provide you with an individualized and appropriate safety plan that often includes your key support people.
Suicide Prevention
If you found this article because you are thinking of harming yourself, stop what you’re doing and call the National Suicide Prevention Lifeline number at 1-800-273-8255.
Look, PMDD mood symptoms can get scary quick. I recommend talking to the people close to you about a protocol if you have thoughts of harming yourself or others.
Here’s a sample plan:
- Call 911 or your emergency medical services.
- Remain by the person’s side until responders arrive.
- Listen with compassion. Avoid yelling, arguing, threatening, or trying to “fix” the person in need of aid.
- Remove any items that can be used to cause harm. E.g. Guns, knives, medications, tools that can be used as weapons.
Keep the National Suicide Prevention Lifeline number 1-800-273-8255 in a prominent place, like your refrigerator.
Discuss with your medical provider if you have or ever had thoughts of harming yourself or others.
Do PMDD symptoms get worse with age?
After age 35, progesterone levels start to decline. This may be the reason that PMDD tends to be more prevalent in populations of older women. However, it doesn’t discriminate. Women of all ages, even young women, can experience PMDD.
How is PMDD treated? Guide to PMDD Treatment
There’s a wide range of treatment options for women with PMDD. Once you’re able to understand that your symptoms aren’t typical and you arrive at the conclusion you’re suffering from PMDD — you can evaluate your options.
In my clinical experience, multiple therapies will need to be employed and you may have to try a few things before you find what works for you.
What medications are used to treat PMDD?
There are several medications commonly used to treat PMDD. For some women they can be helpful and for others, they can make symptoms worse or come with additional side effects.
Hormonal Medications
Hormonal birth control
Many women who describe PMDD symptoms to their doctor’s office will walk out of the office with a prescription for the pill. The idea here is if ovulation is suppressed, then hormonal fluctuations that trigger PMDD don’t occur. However, for some women, it only makes the problems worse…and if it works in the short term, it can wreak havoc later down the road. You can read about birth control side effects here.
If you choose to start hormonal birth control, be sure to track your symptoms to ensure it is helping your condition and not making symptoms worse. If you do experience an increase in symptoms, speak with your doctor immediately.
You can also use my comprehensive patient guide to help support your body while on it.Yaz is currently the only FDA approved birth control to treat PMDD. As I discuss in Beyond the Pill, there are certain populations, like women with PCOS, high blood pressure, and increased clotting risk, who should not use oral contraceptives with drospirenone. Be sure to discuss with your doctor about your individual risk factors.
GnRH Agonist
Leuprolide, for example, stops the ovaries from producing hormones. It is essentially a medication induced menopause. For women who are sensitive to hormonal fluctuations, it may offer some relief. However, because the side effects include depression, anxiety, and difficulty concentrating, it may make these symptoms of PMDD worse.
Antidepressants
Since mood disorders are characteristic of PMDD, many physicians recommend treatment with selective serotonin reuptake inhibitors (SSRIs) even if the patient has no other existing psychiatric conditions. This is generally the primary medication used in the treatment of PMDD. However, just like with any pharmaceutical, these can come with a host of side effects, including:
- Loss of libido
- Insomnia
- Anxiety
- Dizziness
- Dry mouth
- Restlessness
- Nausea
- Vomiting
- Diarrhea
- Drowsiness
Also, many women report very difficult experiences if and when they decide to discontinue taking these drugs. While they’re not considered addictive, they can create a chemical dependency that can be hard to wean off of.
What about a Hysterectomy?
Some women actually get to the point that they are so desperate for relief they have their entire uterus along with ovaries removed. It’s obviously a worst-case scenario but it’s the last resort some women turn to when other methods don’t work for them. And it is important to note that this invasive procedure isn’t a guarantee that your symptoms will go away.
12 Natural Treatments for PMDD
There effective and natural approaches for the treatment of PMDD that can be used as stand alone therapy or combined with other interventions. In my women’s medicine practice I’ve had great success with addressing gut health, inflammation, and hormones as part of a holistic approach to PMDD. I also have my patients work with a mental health professional as part of their treatment strategy.
1. Balance Estrogen
This is the key to creating hormonal harmony for so many women. Problem is, most of the time women visit their doc and get a hormone blood test — and their levels come back “normal,” their issues get dismissed or they’re handed a prescription for the pill and told this is the only option.
Instead, getting the right lab work done that will actually show you an accurate picture of your hormone levels can help tremendously. In my practice I typically test estrogen on day 3 of a woman’s cycle and again with progesterone about 7 days after ovulation.
If we find that women are experiencing excess estrogen, commonly referred to as estrogen dominance, we then address the root of the issue. This generally includes making dietary changes, supporting liver detoxification, gut health, and bringing progesterone levels up. I often recommend Balance Women’s Hormone Support to provide the nutrients that both the liver and gut need to effectively do their job.
I recommend checking out my article: What is Estrogen Dominance + What to do About It for an in-depth strategy.
2. Increase Progesterone
If estrogen is high, chances are good progesterone needs to be boosted. I go into exactly how to increase progesterone in my article 9 Ways to Improve Low Progesterone.
Definitely check out this article if you’re considering bioidentical progesterone.
For some women, progesterone is a complete game changer and can help their symptoms tremendously. For others, the added progesterone can make them feel more tired, prone to crying, and increase breast tenderness. As you’ll read in the article I shared above, it is always best to work with a licensed healthcare professional.
3. What Is the Best Diet for PMDD?
This question comes up a lot in my community. The best diet for PMDD is the one that works for you. I’m going to share some basic guidelines to help you get started in determining that. And I have a meal plan with recipes for you to grab for free to get started.
While diet can be profoundly beneficial to hormonal health and in the management of PMDD symptoms, it is only part of the equation. If you’ve been changing your diet and feeling like a failure because your symptoms aren’t shifting fast enough, I want you to know that you are most certainly not a failure.
Natural therapies work with your body and take time to see results. Think about how many years you’ve experienced PMDD symptoms. Now convert that to months and that’s about how long we can expect you’ll need to put in the work to reclaim your health. Whether it is diet, lifestyle, medications, surgery or other therapies—it will take time to heal. That’s not to say it’ll take that long to feel better at all. You should see gradual improvements. And it is also normal to experience some setbacks, which can sometimes feel like we must be doing something wrong. You’re not. This is what healing looks like.
What Foods Help PMDD?
From the research, it’s unclear how diet can improve PMDD. However, from my clinical experience, I’ve seen women make great improvements in their labs and symptoms from making dietary changes.
Protein and Fat with Meals
If you’re looking to get your PMDD under control, it’s best to eat high quality protein and fat with each meal. This will help support blood sugar stabilization and liver detoxification of hormones. Plus, they supply you with ample nutrients. If you’re a meat eater, choose organic and grass fed as often as possible.
Increase Vegetables Daily
You need lots of veggies and fiber to help keep that estrogen moving out of the body (shoot for 6-9 cups per day). I’ve created a free guide to help you get started eating the right foods to support hormonal balance.
Aim to eat ½-1 cup cooked or raw cruciferous vegetables daily to support estrogen metabolism. Also incorporate nutrient dense leafy greens like spinach, Swiss chard, mustard greens, and collards.
Fiber Rich Foods
Fiber feeds the microbiome, the critters that live in your gut and influence mood and health. Fiber also support elimination of estrogen your body no longer needs, along with metabolic waste.
Eating fresh fruits and vegetables are definitely a great way to increase fiber. Seed cycling, a practice of incorporating specific seeds throughout your cycle, is another way to add fiber and nutrients to support hormone balance. Incorporating lentils, brown rice, burdock root, whole ginger root, artichokes, oats, and chia seeds is another excellent way to diversify the fibers in your diet.
Foods to Reduce or Avoid
These foods can possibly drive hormone imbalance and contribute to worsening symptoms.
Refined Carbohydrates and Sugar
Eating a diet high in sugar or processed carbs can cause blood sugar imbalances and therefore hormone dysregulation. This can lead to shifts in stress hormones and sex hormones.
Caffeine
Additionally, some women are greatly affected by caffeine and experience more anxiety, sleepless nights, and breast tenderness. Doing a trial elimination can help you understand if this is true for you.
Alcohol
When stress is high it can be tempting to reach for a glass of wine or 2, but alcohol can disrupt sleep, cause unfavorable mood shits, and is known to raise estrogen levels.
This doesn’t mean you can never have a drink, a piece of cake, or enjoy a latte. This means you need to evaluate how these particular foods impact your health and affect your body.
4. Reduce chemical exposure
We are exposed to hundreds of endocrine disrupting chemicals in pesticides, common household products, beauty products and even building materials every day. These chemicals can trick our bodies into thinking they are actual hormones — or prevent our natural hormones from doing their jobs. Try your best to use natural beauty products, eat organic produce and meat, and ditch the plastics, it will only serve to decrease your PMDD symptoms.
Watch this video to learn more about endocrine disruptors and how to support your body.
5. Cognitive behavioral therapy
Due to the mental health component of the disorder that can spiral into negative self-talk and depression, therapy is a beneficial modality for many women with PMDD. I recommend working with a mental health expert as part of your health care team.
Often, women with PMDD struggle with their personal relationships due to the difficulties of the condition. This is true for all people who are dealing with anxiety, depression, irritability, and bouts of anger. Having a counselor to talk to and guide behavior and thought modification can be a huge help. There’s never any shame in pursuing optimal mental health!
Can Supplements Help PMDD?
There are several amazing herbs and supplements that can help create hormonal balance and reduce PMS & PMDD severity.
Supplements that may calm PMDD
- Vitex agnus castus (also known as chasteberry)
- Black Cohosh
- Magnesium
- Vitamins B6, B12, and folate
- Vitamin E
- DIM
- Calcium
- Green Tea
- Rhodiola
- High-quality probiotic
6. Vitex agnus castus (VAC) for PMDD
In one systematic review it was concluded that “RCTs using VAC for treatment of PMS/PMDD suggested that the VAC extract is a safe and efficacious alternative to be considered for the treatment of PMS/PMDD symptoms.” In another systematic review it was found that the use of Vitex was associated with an over 50% reduction in symptoms for most women experiencing PMS/ PMDD with no serious side effects.
There have been many studies on the benefits of Vitex for women’s health conditions and in my clinic, I have seen it help a lot of women experiencing symptoms of PMS and PMDD. This is why you’ll find Vitex in my Balance Women’s Hormone Support supplement
7. Calcium for PMDD
Calcium has been shown to be helpful in both PMS and PMDD. In fact, it is among one of the top nutrients recommended by the Mayo Clinic for PMDD, along with magnesium, vitamin E, Vitamin B6, and tryptophan. Aim for 1,200 mg of calcium via diet and supplements.
Broccoli, bok choy, mustard greens, Chinese cabbage, and sardines are excellent sources of calcium. While dairy does contain calcium, it can make premenstrual symptoms worse for some women and increased acne breakouts. It’s best to gauge if dairy works for your body.
You’ll also find highly absorbable calcium in my Women’s Twice Daily supplement, as well as Prenatal Plus.
8. Magnesium for PMDD
Magnesium is essential to having a healthy mood, hormones, energy, and feeling calm. Aim for 300-600 mg daily depending on your symptoms. This mineral can help with sore breasts, bloating, and cramps. You can find magnesium in nuts, seeds, and greens.
I recommend choosing a supplement with magnesium bisglycinate such as our Magnesium Plus capsules, as it is a highly absorbable form that doesn’t tend to cause digestive issues.
9. Vitamin E for PMDD
Vitamin E can help with menstrual cramps by reducing prostaglandins, hormone like substances that can lead to cramps. Avocados, nuts, seeds, shrimp, and oils are excellent sources of vitamin E.
You’ll also find vitamin E in my Women’s Twice Daily supplement, as well as Prenatal Plus.
10. Vitamin B6 for PMDD
Vitamin B6 is incredibly beneficial in women’s health, especially when it comes to optimizing your hormones. You can read this article on Vitamin B6 Benefits for Women.
To help with irritability, fatigue, insomnia, and mood, aim for 50-100 mg of B6 daily. You’ll find vitamin B6 in chickpeas, salmon, and avocado.
My Period Problems Kit™ delivers 35 mg of vitamin B6 and is designed to address your hormones, liver, gut and adrenal health. I’ve seen improvements in overall energy, mood, and menstrual cycles for women who support their liver, adrenals and gut health with supplements in combination with a nutrient dense diet.
11. Acupuncture for PMDD
Acupuncture has been shown to reduce symptoms of PMS and PMDD by as much as 50% without any significant adverse side effects. It is important to work with a licensed acupuncturist who has had sufficient training. My patients have reported better outcomes when working with an LAc, opposed to a provider practicing medical acupuncture after very little training. That’s not to say you wouldn’t benefit from a session with an MD practicing acupuncture, but rather, if you don’t experience benefits it may mean you need to look for a different provider.
12. Exercise for PMDD
Aerobic exercise daily can be beneficial for women struggling with symptoms of PMDD. Aim for 30 minutes daily. You can split it up into 10 minutes three times a day or 30 minutes all at once. Find activities you enjoy like dance, cycling, kickboxing, jogging, or HIIT.
Share the Guide to Treating PMDD
Remember, just because PMS, PMDD, and symptoms of hormone imbalance are common that doesn’t mean it should be accepted as normal.
If you’re reading this article and recognizing the symptoms of PMDD in yourself but your physician isn’t hearing your concerns, get a second opinion. If you’re not seeing improvement with the treatments you’ve been provided, ask your provider about some of the therapies discussed here.
And don’t stop until you find the answers you need.
So often, women suffer in silence, and don’t realize that what we’re experiencing is not normal and that there are therapies that can help.
We can help each other move forward and improve women’s medicine by talking about our experience and sharing what has helped. You never know who will heal by hearing your story. Spread the word however you can.
You can start by sharing this post — you never know who’s hurting and could use a little bit of help finding the right information. And I’d love to hear from you in the comments about your experience and what has helped.
References
Yamada K, Kamagata E. Reduction of quality-adjusted life years (QALYs) in patients with premenstrual dysphoric disorder (PMDD). Qual Life Res. 2017 Nov;26(11):3069-3073. doi: 10.1007/s11136-017-1642-1. Epub 2017 Jul 3. PubMed PMID: 28674766.
https://www.ncbi.nlm.nih.gov/pubmed/28674766.
Pearlstein T, Steiner M. Premenstrual dysphoric disorder: burden of illness and treatment update. J Psychiatry Neurosci. 2008;33(4):291–301.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2440788/.
Schmidt PJ, Nieman LK, Danaceau MA, Adams LF, Rubinow DR. Differential behavioral effects of gonadal steroids in women with and in those without premenstrual syndrome. N Engl J Med. 1998 Jan 22;338(4):209-16. doi: 10.1056/NEJM199801223380401. PubMed PMID: 9435325.
https://www.ncbi.nlm.nih.gov/pubmed/9435325.
Dubey, N., Hoffman, J., Schuebel, K. et al. The ESC/E(Z) complex, an effector of response to ovarian steroids, manifests an intrinsic difference in cells from women with premenstrual dysphoric disorder. Mol Psychiatry 22, 1172–1184 (2017) doi:10.1038/mp.2016.229
https://www.nature.com/articles/mp2016229.
Yen JY, Wang PW, Su CH, Liu TL, Long CY, Ko CH. Estrogen levels, emotion regulation, and emotional symptoms of women with premenstrual dysphoric disorder: The moderating effect of estrogen receptor 1α polymorphism. Prog Neuropsychopharmacol Biol Psychiatry. 2018 Mar 2;82:216-223. doi: 10.1016/j.pnpbp.2017.11.013. Epub 2017 Nov 14. PubMed PMID: 29146473.
https://www.ncbi.nlm.nih.gov/pubmed/29146473.
Dubey N, Hoffman JF, Schuebel K, Yuan Q, Martinez PE, Nieman LK, Rubinow DR, Schmidt PJ, Goldman D. The ESC/E(Z) complex, an intrinsic cellular molecular pathway differentially responsive to ovarian steroids in Premenstrual Dysphoric Disorder, Molecular Psychiatry, January 3, 2016, doi:10.1038/mp.2016.229. https://www.nih.gov/news-events/news-releases/sex-hormone-sensitive-gene-complex-linked-premenstrual-mood-disorder.
Skovlund CW, Mørch LS, Kessing LV, Lidegaard Ø. Association of Hormonal Contraception With Depression. JAMA Psychiatry. 2016;73(11):1154–1162. doi:https://doi.org/10.1001/jamapsychiatry.2016.2387
https://jamanetwork.com/journals/jamapsychiatry/fullarticle/2552796.
Reuveni I, Dan R, Segman R, Evron R, Laufer S, Goelman G, Bonne O, Canetti L. Emotional regulation difficulties and premenstrual symptoms among Israeli students. Arch Womens Ment Health. 2016 Dec;19(6):1063-1070. doi: 10.1007/s00737-016-0656-y. Epub 2016 Aug 18. PubMed PMID: 27538401.
https://www.ncbi.nlm.nih.gov/pubmed/27538401.
Yen JY, Tu HP, Chen CS, Yen CF, Long CY, Ko CH. The effect of serotonin 1A receptor polymorphism on the cognitive function of premenstrual dysphoric disorder. Eur Arch Psychiatry Clin Neurosci. 2014 Dec;264(8):729-39. doi: 10.1007/s00406-013-0466-4. Epub 2013 Oct 26. PubMed PMID: 24158751. https://www.ncbi.nlm.nih.gov/pubmed/24158751.
Slyepchenko A, Frey BN, Lafer B, Nierenberg AA, Sachs GS, Dias RS. Increased illness burden in women with comorbid bipolar and premenstrual dysphoric disorder: data from 1 099 women from STEP-BD study. Acta Psychiatr Scand. 2017 Nov;136(5):473-482. doi: 10.1111/acps.12797. Epub 2017 Aug 28. PubMed PMID: 28846801; PubMed Central PMCID: PMC5630503. https://www.ncbi.nlm.nih.gov/pubmed/28846801.
Reid RL. Premenstrual Dysphoric Disorder (Formerly Premenstrual Syndrome) [Updated 2017 Jan 23]. In: Feingold KR, Anawalt B, Boyce A, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Table 1, Diagnostic Criteria for Premenstrual Dysphoric Disorder (PMDD)
https://www.ncbi.nlm.nih.gov/books/NBK279045/table/premenstrual-syndrom.table1diag/.
de Carvalho AB, Cardoso TA, Mondin TC, da Silva RA, Souza LDM, Magalhães PVDS, Jansen K. Prevalence and factors associated with Premenstrual Dysphoric Disorder: A community sample of young adult women. Psychiatry Res. 2018 Oct;268:42-45. doi: 10.1016/j.psychres.2018.06.005. Epub 2018 Jun 26. PubMed PMID: 29986177.
https://www.ncbi.nlm.nih.gov/pubmed/29986177.
Abdominal hysterectomy – Mayo Clinic. 2019. https://www.mayoclinic.org/tests-procedures/abdominal-hysterectomy/about/pac-20384559.
Sepede G, Sarchione F, Matarazzo I, Di Giannantonio M, Salerno RM. Premenstrual Dysphoric Disorder Without Comorbid Psychiatric Conditions: A Systematic Review of Therapeutic Options. Clin Neuropharmacol. 2016 Sep-Oct;39(5):241-61. doi: 10.1097/WNF.0000000000000173. Review. PubMed PMID: 27454391.
https://www.ncbi.nlm.nih.gov/pubmed/27454391.
Lykkegaard LA, Videbech P. [Discontinuation syndrome after SSRI antidepressants]. Ugeskr Laeger. 2014 Feb 3;176(3):231-5. Review. PubMed PMID: 24629750.
https://www.ncbi.nlm.nih.gov/pubmed/24629750.
Gore A, Crews D, Doan L, La Merrill M, Patisaul H, Zota A. Introduction to Endocrine Disrupting Chemicals (EDCs). December 2014. https://www.endocrine.org/-/media/endosociety/files/advocacy-and-outreach/important-documents/introduction-to-endocrine-disrupting-chemicals.pdf?la=en.
Cognitive behavioral therapy – Mayo Clinic. 16 Mar. 2019, https://www.mayoclinic.org/tests-procedures/cognitive-behavioral-therapy/about/pac-20384610.
Lanza di Scalea T, Pearlstein T. Premenstrual Dysphoric Disorder. Psychiatr Clin North Am. 2017 Jun;40(2):201-216. doi: 10.1016/j.psc.2017.01.002. Epub 2017 Mar 1. Review. PubMed PMID: 28477648.
https://www.ncbi.nlm.nih.gov/pubmed/28477648.
Cerqueira RO, Frey BN, Leclerc E, Brietzke E. Vitex agnus castus for premenstrual syndrome and premenstrual dysphoric disorder: a systematic review. Arch Womens Ment Health. 2017 Dec;20(6):713-719. doi: 10.1007/s00737-017-0791-0. Epub 2017 Oct 23. Review. PubMed PMID: 29063202.
https://www.ncbi.nlm.nih.gov/pubmed/29063202.
Fathizadeh N, Ebrahimi E, Valiani M, Tavakoli N, Yar MH. Evaluating the effect of magnesium and magnesium plus vitamin B6 supplement on the severity of premenstrual syndrome. Iran J Nurs Midwifery Res. 2010;15(Suppl 1):401–405.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3208934/.
Shobeiri F, Araste FE, Ebrahimi R, Jenabi E, Nazari M. Effect of calcium on premenstrual syndrome: A double-blind randomized clinical trial. Obstet Gynecol Sci. 2017;60(1):100–105. doi:10.5468/ogs.2017.60.1.100
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5313351/.
