Sex and sexuality are highly individualized, as people have different sex drives and desires. How much sex you want to have and your interest in intimacy is deeply personal. But for many people, sex is essential to well-being1, encompassing physical, social, and psychological wellness.
With all that said, it can come as a surprise if your feelings towards sex — and how your body responds — change during perimenopause. If you've noticed changes in your sex drive as you enter and move through perimenopause, you’re not alone. It's estimated that around 45% of women experience sex-related2 issues in midlife.
Sexual dysfunction, the difficulty or inability to respond to sexual cues, can affect how you feel about yourself, your mood, intimate relationships, and your overall quality of life. While medicine and research classify these issues as sexual dysfunction, I prefer to look at them as adaptation, since there is often a root cause to why your body is behaving in this way. It’s not that you’re broken, but often, it is your body’s way of protecting you. Despite these issues being common, many women don't seek support3, either because they're embarrassed to bring it up with a healthcare practitioner (and most doctors don't ask) or because so many people accept this as a normal part of getting older and something they must live with.
I'm here to tell you that while your body and hormones do change during perimenopause in a way that can impact your sex life, you don't have to say goodbye to sexual pleasure. While these changes are expected, you can take steps to make sure you still enjoy a healthy and active sex life.
In this article
- What is Perimenopause?
- Is it Normal to Lack Sex Drive During Perimenopause?
- What are Other Symptoms of Perimenopause?
- How Are Sexual health and Intimacy Maintained During Perimenopause?
- Should I Consider Hormone Replacement Therapy For Perimenopause Symptoms?
- Takeaway: A Healthy Sex Life Is Possible During Perimenopause
What is Perimenopause?
Perimenopause is the transitional phase between the “reproductive years” (when you have a menstrual cycle) and menopause, which is marked by not having a period for 12 consecutive months. It's linked with significant hormonal shifts that can feel like a physical and emotional roller coaster.
The earliest signs of perimenopause4 include subtle changes in the menstrual cycle, energy, mood, and weight. As hormones that control your cycle fluctuate, you may experience shorter cycles, heavier periods, and more frequent spotting.
Ovulation — when the ovary releases an egg — becomes erratic in the later stages of perimenopause. This results in progesterone and estrogen5 levels varying from cycle to cycle. These changing hormones also impact your sex drive and libido, among other symptoms.
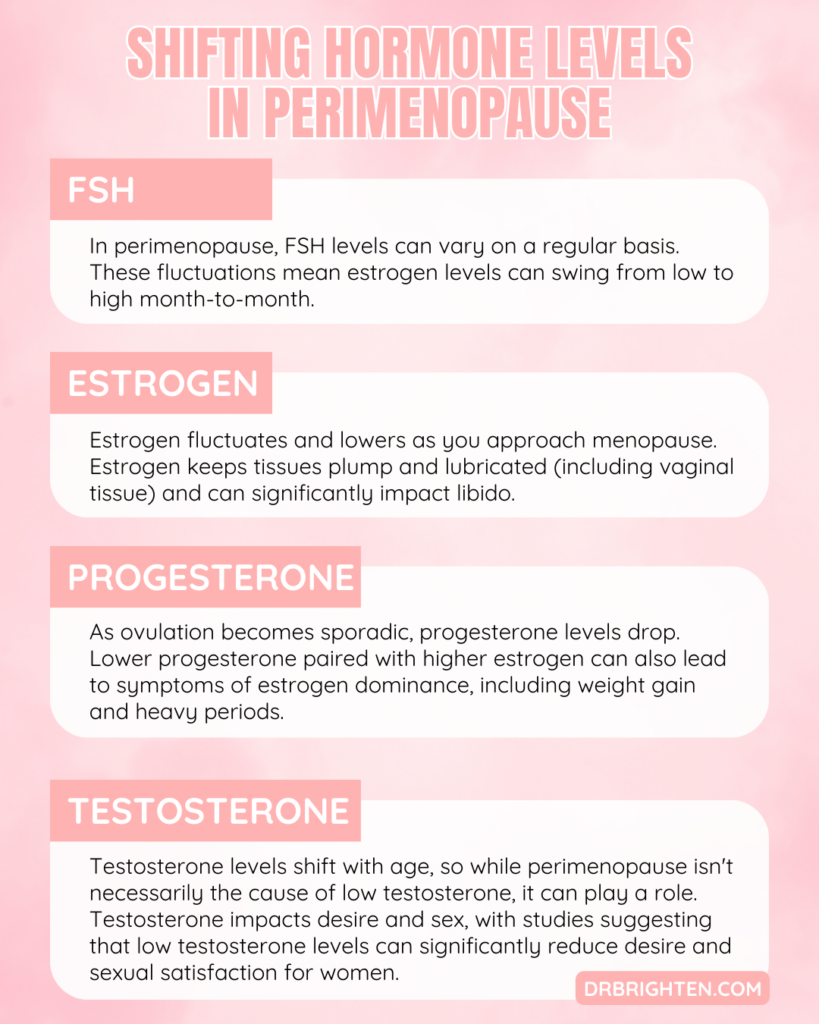
Shifting Hormone Levels in Perimenopause
Hormones are behind the physical and emotional changes of perimenopause. You can find a detailed list of what I use to evaluate my patients’ hormones by taking the quiz in my new book “Is This Normal,” but here are some I consider especially important for perimenopause and sexual health:
- FSH: Follicle-stimulating hormone (FSH) stimulates the follicles in the ovaries to produce mature eggs. In perimenopause, FSH levels6 can vary from month to month, which is why is one reason why it is difficult to test and diagnose perimenopause with labs. High FSH stimulates higher estrogen in the ovaries, while low FSH means less estrogen. These fluctuations mean estrogen levels can swing from low to high month-to-month.
- Estrogen: Fluctuating estrogen7 is also seen in perimenopause, often higher in earlier phases and lower as you get closer to menopause. Estrogen keeps tissues plump and lubricated (including vaginal tissue) and can significantly impact libido.
- Progesterone: As ovulation becomes sporadic, progesterone levels drop, causing irregular cycles and missed periods. Progesterone also influences mood shifts, insomnia, and libido changes. Lower progesterone paired with higher estrogen can also lead to symptoms of estrogen dominance, including weight gain and heavy periods.
- Testosterone: Testosterone levels8 shift with age, so while perimenopause isn't necessarily the cause of low testosterone, it can play a role. Testosterone impacts desire and sex, with studies9 suggesting that low testosterone levels can significantly reduce desire and sexual satisfaction for women. It’s important to note that low testosterone results in more symptoms than just a low libido, so if you find yourself struggling with your mood, muscle mass, or weight, it may be time to look into low testosterone.
When Does Perimenopause Start?
Perimenopause starts around age 45, on average. Some women start earlier10, and timing can depend on factors such as race, ethnicity, medical conditions, genetics, or where you live.
You can also download our free Perimenopause Plan here to get expert guidance tailored to your journey.
Is it Normal to Lack Sex Drive During Perimenopause?
It's common to lack sex drive11 during perimenopause, but the reasons are complex and this shouldn’t be regarded as a “new normal.” Studies on interest in sex and desire are challenging because desire and sex drive are so subjectively experienced. It can be influenced by physical, physiological, psychological, social, and cultural factors that vary from person to person.
While studies12 consistently show that women report low libido during perimenopause, others suggest that women may masturbate more often. So it may not necessarily be that the desire for pleasure is as low as is reported or it may be there’s more complex factors at play.
Contributing causes13 to low desire include hormone imbalances, discomfort during sex, difficulty achieving orgasm, or even body image concerns.
I'm going to start with potential reasons why you might lack sex drive during perimenopause, but this article will end with solutions to help you get your libido back.
Changes in Sexual Desire and Arousal
Sexual desire encompasses the feelings of wanting sex, while arousal includes the physical signs of readiness for sex, such as lubrication or increased blood flow, along with neurological changes, like getting more excited. In some instances, desire comes before arousal, but for many women, the physiological response precedes feelings of desire. This is the opposite of what is true for most men, who tend to follow the desire then physical arousal pattern. During perimenopause, these two processes can both become disconnected.
Hormonal shifts can impact physical arousal, resulting in decreased lubrication, tissue engorgement of the nipples, labia, and clitoris, and a phenomenon known as vaginal tenting (where the vagina prepares for penetration), even when you are interested and connected with your partner. The result can be a disconnect between the mental and physical aspects of the sexual experience, making it difficult to enjoy sex.
As we reach the later stages of perimenopause, the declining estrogen and perhaps, even testosterone, can lead to a decrease in vaginal and pelvic floor health. Vaginal dryness, which we’ll discuss shortly, increased risk of UTIs, pelvic floor weakness, urinary incontinence, and prolapsed tissue can accompany these hormone changes and worsen as we enter menopause.
Studies14 on hormones in menopause suggest hormone replacement therapy has significant benefit on sexual health for women, which further exemplifies the importance of hormones. From my clinical perspective, it is better to be proactive about hormonal and sexual health in perimenopause as we know the transition into menopause is both inevitable and can have a major impact on overall health. Keep reading because I’ll provide you tips for wherever you are on this journey.
Vaginal Dryness
Vaginal dryness in perimenopause is related to a decrease in estrogen. Estrogen helps with natural lubrication and blood flow to the vagina, but when the hormone drops, lubrication can become sparse, and sex can be painful. Once this happens, desire also drops as there's an increased fear of sex hurting. Plus, dry tissue and low estrogen put women in perimenopause at risk for urinary tract infections15 (UTIs), which can further reduce sexual desire.
A study in Menopause found a reported 30% increase in sexual dysfunction scores during perimenopause16, and vaginal dryness was a primary reason for the change. This physical change independently impacted desire, arousal, ability to orgasm, and overall sexual satisfaction. This is an estrogen problem, not a “I’m broken” problem.
Some research17 also suggests that the vaginal microbiome shifts in midlife, which could also affect vaginal tissue. Healthy lactic acid-producing bacteria (the lactobacilli strains) in the vagina may help keep the pH lower and, therefore, more acidic, creating an inhospitable environment for harmful bacteria. Estrogen is also a key player in your vaginal ecology, which is why as estrogen begins it’s decline, a daily probiotic may be especially helpful.
As the balance of these beneficial bacteria shifts, pH increases which can influence vaginal health. Women's Probiotic by Dr. Brighten was specifically designed to support a balanced vaginal microbiome and healthy hormones.
As I will discuss below, lubricants are your friend here. But if you already use lubricants and still have any pain or burning with sex, you should always discuss it with your healthcare provider.
Irregular Periods
I mentioned that irregular periods are sometimes the first sign of perimenopause that women clue into, but what does this have to do with sex? Since hormonal shifts can impact how we feel about sex — for example you might feel friskier around ovulation — those same hormonal shifts can also impact when and if you are in the mood during perimenopause.
If you suddenly have short menstrual cycles due to lower progesterone levels, or aren't ovulating some months, then you might not feel as interested in sex comparatively speaking. Similarly, if your periods are heavier due to stimulation by estrogen and lack of sufficient progesterone, or you have symptoms of PMS, like bloating, cramping, or headaches, then that will also impact sex drive, especially if it's happening every three weeks.
Lastly, pregnancy can still happen in perimenopause and the “threat” of an unintended pregnancy is among the primary reasons women will have difficulty with desire and arousal—it can even take you out of the mood once things get going. An unpredictable period means ovulation is a moving target, which can produce anxiety and worry for some people.
Reaching Orgasm
Clitoral stimulation is the primary way women arrive at orgasm. During perimenopause, especially the later phase, clitoral sensitivity can decline. While low estrogen is a universal culprit during this stage of life, decreased insulin sensitivity can also play a role.
Your ability to reach orgasm relies on both physical and psychological aspects of sex, and both are equally important.
If physical signs of arousal are low, sex becomes less enjoyable, and reaching orgasm can be more difficult. Or if you're worrying that sex may hurt, it can make things less than pleasurable, and you may be too distracted to relax and enjoy yourself. Plus, low estrogen18 means reduced blood flow to the vagina and clitoris, which can make it harder to become aroused or orgasm.
All the above doesn't even include some of the psychological pieces that influence your ability to reach orgasm. Mood, body image, and your relationship with your partner (all discussed below) can also have an impact.
Changes in Insulin Sensitivity
Your hormones are intimately tied, which means if one shifts, others follow. In the case of insulin, as estrogen declines, your cell’s ability to utilize insulin can change. The result can be decreased insulin sensitivity, which results in blood sugar imbalances and body composition changes (more on body image soon).
In type 2 diabetes19, a significant form of insulin resistance, vascular damage caused by prolonged elevations in blood glucose can cause decreased blood flow to the vagina and clitoris. This impedes arousal. Additionally, this impacts clitoral engorgement (which is the same mechanism by which a penis becomes erect), and the nerve sensitivity of the clitoris is reduced. This all translates to an inability of the tissues to respond to sexual stimuli and for pleasure to be transmitted to the brain.
As we progress through late perimenopause and subsequently into menopause, the low levels of estrogen increase our risk of metabolic issues20, like insulin resistance. The same factors that put us at increased risk of heart disease and diabetes are also impacting our sexual function.
Changes in Mood
So far, we've focused on the physical changes that could impact your sex drive during perimenopause, but understanding the emotional piece is just as important. Symptoms of depression or anxiety21 can increase during perimenopause, especially if you have a history of depression. New onset depression may arise as well.
Depression22 can lead to sexual dysfunction (including some of the medications used to treat it), but sexual dysfunction can also lead to mood changes and feelings of sadness. It's so important to pay attention to your mental health during this time and reach out for help if needed.
Sleep Problems
Sleep impacts every single part of health at any age, and I'm constantly promoting sleep hygiene to my patients. Perimenopause is no different, and unfortunately, daily life, stress, fatigue, and hormone fluctuations can lead to irregular sleep.
Vasomotor symptoms (fluctuating body temperatures) can contribute as women with night sweats experience interrupted sleep and insomnia23. Low progesterone also contributes to insomnia (progesterone is key for GABA, a neurotransmitter that helps with sleep), increasing the risk of sleep disturbances.
When you're exhausted or worried about not getting enough sleep, sex might be the last thing on your mind. In other words, low libido and a decrease in sexual responsiveness due to hormone fluctuations are only exacerbated by fatigue.
If you’re struggling with sleep, try these sleep solutions.
Changes in Body Image
Perimenopause can also lead to changes in how you feel about your body. Once again, hormones influence weight and metabolism. Estrogen24, for example, affects fat burning and how you use and store carbohydrates. Weight gain, or feeling like what used to work in terms of diet and exercise no longer does, can lead to body dissatisfaction — so much so that some studies suggest that perimenopause can increase the risk of developing an eating disorder25.
If you don't feel good in your body, sex becomes less appealing. You may also have conflicting emotions about aging in general. It's completely normal for our bodies to change, but we also live in a world that celebrates youth, and we're targeted with anti-aging ads all the time. These messages can sneak into our heads and live rent-free, affecting our comfort in intimate situations.
Check out this article if you’re looking for support around perimenopause body composition changes.
Changes in Relationship Dynamics
Finally, perimenopause coincides with a time when many women are navigating many other life changes. Maybe you're suddenly an empty nester and finding your way in a new life stage, or you're dealing with aging parents and trying to balance their needs with your own.
You also may be struggling with a partner who wants more intimacy, and you feel you can't meet their needs due to physical discomfort, and it's become a conflict in your relationship. All of this can contribute to a lack of desire and finding space in your life for wanting to have sex.
Couples counseling can help you and your partner communicate openly as your needs change. Finding someone to help guide your conversations may be just what you need to get back on course. Additionally, an AASECT certified sex therapist may also be an ally during this time of life.
What are Other Symptoms of Perimenopause?
I can't discuss perimenopause without touching on two common symptoms: hot flashes and night sweats.
Hot Flashes
Hot flashes feel like a sudden warming of the face and body, with sweating and sometimes skin redness. They can last seconds to minutes and happen to up to 80% of women26 during perimenopause.
Night Sweats
Night sweats are like hot flashes but occur primarily during sleep, so you wake up drenched with sweat.
Both can also contribute to a lower sex drive, as if you may be exhausted and drained or simply feel like you need more space away from your partner to avoid the intensity of your physical symptoms.
I mean, who wants an extra heat generating body against theirs when they’re already overheating?
How Are Sexual health and Intimacy Maintained During Perimenopause?
Yes, all the above can happen, but that doesn't mean your sex life has to suffer. Here are some tips for keeping things going strong:
Perimenopause Hormone Support:
Nutrition and lifestyle are essential for hormone balance and improving sexual desire, arousal, orgasms, and pleasure during perimenopause. I’m going to share some key areas to focus on, but there are also many supplements I use in practice that support hormones, stress response, sleep, and more.
Balance Women’s Hormone Support by Dr. Brighten was formulated with specific botanicals and nutrients that support changing hormones to help you feel better in your body. It contains the trifecta of DIM, calcium D-glucarate, and sulforaphane to help with proper estrogen metabolism—that is the processing of the estrogen your body is no longer using. In addition, it contains magnesium, calcium, and B6 to support healthy moods. The blend of herbs and nutrients also support those ovaries in making progesterone for as long as they can.
Adrenal Support helps these two little glands optimize their DHEA and stress hormone production. As I’ve discussed in other articles, the adrenal glands are key in late perimenopause and menopause in producing DHEA, a precursor to estrogen and testosterone. If we’ve got low estrogen, then herbs and nutrients to give those adrenal glands the support they need is a must.
Women’s Probiotic is a blend of spore-based organisms for gut health and lactobacilli species for vaginal health. It also contains antioxidants to support the urinary tract and a prebiotic to help the good stuff grow in the gut. As I mentioned above, a probiotic is a key supplement to put into the routine as we enter perimenopause.
Myoinositol Plus is formulated to support the body in getting a good night’s sleep and helping blood sugar stay in check.
Proactive Communication With Your Partner:
It's not always easy, but honest, open conversations about fears, stress, and what's happening in your body are essential to maintain intimacy during perimenopause. Talking to your partner will help you feel connected, and together you can create a roadmap to navigate these changes in your sex life.
I’ve also found with my patients that their partners are sometimes internalizing what they feel is “rejection” because they don’t understand the changes of perimenopause. No one gives your partner a manual to understanding your body and your experiences are unique, which is all to say, you’ve gotta check in with them about your needs and what you’re going through.
Physical Activity:
Exercise can help by boosting endorphins to help your mood, improve sleep, increase lean body mass, and reduce stress, which are all factors contributing to a healthy sex drive. Consider a mix of stability, strength, flexibility, and cardio for optimal benefits.
As I’ve discussed in articles about perimenopause metabolism and weight, strength training is a must in perimenopause. This will help your body stay sensitive to insulin, produce testosterone, reduce stress hormones, and can improve your pelvic floor health.
Additionally, exercise has been shown in numerous studies to improve sexual health!
Dietary Considerations:
Nutrition is crucial during perimenopause to ensure you get all the necessary nutrients to support healthy hormones. Antioxidants27, fiber, protein, vitamins, and minerals can all influence symptoms of perimenopause and influence sex drive. You can find a lot more detail about the ideal diet for perimenopause in my article here.
If you need extra support to optimize your diet for hormones, my free Hormone Balancing Starter Kit with a 7-day meal plan and recipe guide can help you get started.
Stress Management:
We know stress28 lowers libido, so targeted approaches to lower your stress are a no-brainer.
If you're stressed, cortisol can make it harder to lose weight, increase your blood sugar, and adversely impact your adrenals. Stress also makes you tired and can wipe out your sex drive. Taking care of yourself, whether that means yoga, meditation, or taking a few minutes to breathe and center yourself, can make a difference (and sex can be a stress reliever, too!).
Basically, stress is going to make your body choose survival over sex, which to your body, is an expensive baby-making event.
Vaginal Moisturizers and Lubricants:
Lubricants are your friend during perimenopause. They can make sex more pleasurable and help to reduce pain or friction during intercourse. I have an entire article devoted to lubricant, where you can learn more.
Should I Consider Hormone Replacement Therapy For Perimenopause Symptoms?
Early in perimenopause hormone replacement therapy or HRT may not be necessary as the ovaries are still able to produce hormones. Supporting your body with the nutrition, lifestyle, and supplement therapies discussed above can go a long way in helping you manage symptoms. This is your foundation for hormone health.
As you progress in perimenopause, you’ll want to keep that foundation going and may want to consider progesterone therapy. Since ovulation is the way we produce sufficient progesterone and ovulation is becoming less of a regular occurance, progesterone therapy may help. However, while oral progesterone (not the progestin found in birth control) can help alleviate moods and support sleep, it may also make it a little more challenging to get in the mood. That being said, if it benefits sleep and moods, this might not be the case and it may actually help.
Estrogen therapy is often reserved for late perimenopause and menopause. However, topical estriol, E3, applied to the vulva can be helpful in eliminating vaginal dryness, atrophy, and supporting sexual health. Keep in mind though, you don’t want to expose your partner to these hormones so apply them after being intimate, rather than before.
Testosterone hormone replacement therapy or alternatively, DHEA, can be used in women, although it has yet to gain FDA approval. It may be helpful to use DHEA when women are on the pill or experiencing symptoms in early perimenopause. While testosterone therapy can improve libido, mood, muscle mass, and even immune function in some people—it is not a cure all for low sexual desire or other sexual concerns.
HRT is very individualized and should be considered in every perimenopause or postmenopausal woman. That doesn’t mean everyone is a candidate, but they should at least be considered. The best course of action is to talk to your medical provider who knows your health intimately so they can guide you on what’s best for your care.
Takeaway: A Healthy Sex Life Is Possible During Perimenopause
The hormone changes in perimenopause can impact your body, but it doesn't mean your sex life is over. Understanding the root causes of these changes — physical and emotional — can help you develop a plan to feel like yourself again.
Changes at this time can be related to hormone shifts, but stress, body image, and life changes can also play a role. I'd love it if all women could see perimenopause as a powerful shift to a chapter of freedom and wisdom, but I also know that age is a complicated topic, and many women have a hard time during the transition, especially when symptoms are running your life. Add on feelings of sexual inadequacy, and it can be overwhelming.
It’s important to seek out medical and psychological support to help you through this transition. There will be bumps along the way, but the right support can help smooth the ride. Diet, supplements, sleep, stress, and communication with your partner can all help as your hormones change during perimenopause. With the right tools, you can look forward to a healthier sex life at any age.
References
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6487288/ ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6226268/ ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6226268/ ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4834516/ ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6082400/ ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7676929/ ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4834516/ ↩︎
- https://journals.lww.com/menopausejournal/Abstract/2018/11000/Predictors_of_decreased_libido_in_women_during_the.12.aspx ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6487288/ ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3285482/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/35675610/ ↩︎
- https://journals.lww.com/menopausejournal/Abstract/2018/11000/Predictors_of_decreased_libido_in_women_during_the.12.aspx ↩︎
- https://pubmed.ncbi.nlm.nih.gov/19212271/ ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6963159/ ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6629580/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/31738734/ ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6226268/ ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6487288/ ↩︎
- https://www.mdpi.com/2673-4540/1/1/2 ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4440199/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/27475888/ ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5900810/ ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3185248/ ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8308420/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/26857889/ ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6082400/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/30086485/ ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4199300/ ↩︎
