There is a significantly higher prevalence of PMDD (premenstrual dysphoric disorder) among those with ADHD (attention deficit hyperactivity disorder). In fact, it is estimated that 46% of women with (ADHD) also struggle with PMDD. When compared to the general population, with only 28% reporting PMDD, it is clear those with ADHD are at increased risk.
In this article

If you find that you're experiencing the following symptoms the week or two before your period then I encourage you to continue reading:
- Worsening ADHD symptoms: decreased concentration, difficulty with executive function, hyperactivity, etc
- Increased emotions or mood swings
- Anxiety, sleep disturbance, and agitation
- Physical aches, pains, and discomfort
- Reduced effectiveness of stimulant medications

If you have ADHD, PMDD, or potentially both, you know that these two conditions can significantly impact your mental well-being and daily life.
While ADHD and PMDD might seem to affect different aspects of health—ADHD causing difficulty with concentration, for example, and PMDD causing pain and mood-related issues—they often coexist and exacerbate each other's symptoms.
In this article, we'll explore the ADHD-PMDD connection, discuss common symptoms and causes of both, and provide tips for helping to cope with issues such as anxiety before your period, severe fatigue, irritability, and trouble sleeping.
Among the key takeaways you'll learn about the connection between ADHD and PMDD include:
- Both conditions involve neurotransmitter imbalances, hormonal fluctuations, and changes in brain function.
- Dopamine and serotonin are affected in both ADHD and PMDD, impacting moods and mental well-being.
- Estrogen and progesterone influence neurotransmitter activities and issues with emotional regulation experienced by those with ADHD and PMDD.
- PMDD symptoms can worsen ADHD symptoms and vice versa.
- ADHD symptoms tend to heighten and medications may become less effective during the luteal phase, regardless of PMDD being present.
Symptoms of PMDD and Underlying Causes

Premenstrual Dysphoric Disorder, or PMDD, describes severe emotional and physical symptoms that occur in the days or weeks leading up to menstruation. Between 5% and 8%1 of women in their reproductive years struggle with PMDD.
While many women (up to 85%) experience mild or moderate PMS symptoms, PMDD is different because it can cause significant impairment in daily functioning during the 10 to 14 days prior to a woman's period starting.
Common PMDD symptoms that show up in the premenstrual phase include:
- Severe mood swings
- Irritability or anger
- Depression or feelings of hopelessness
- Anxiety or tension
- Decreased interest in usual activities
- Difficulty concentrating, brain fog
- Extreme fatigue
- Changes in appetite or food cravings
- Trouble sleeping, insomnia, or sleeping too much
- Physical symptoms such as breast tenderness, bloating, or joint or muscle pain
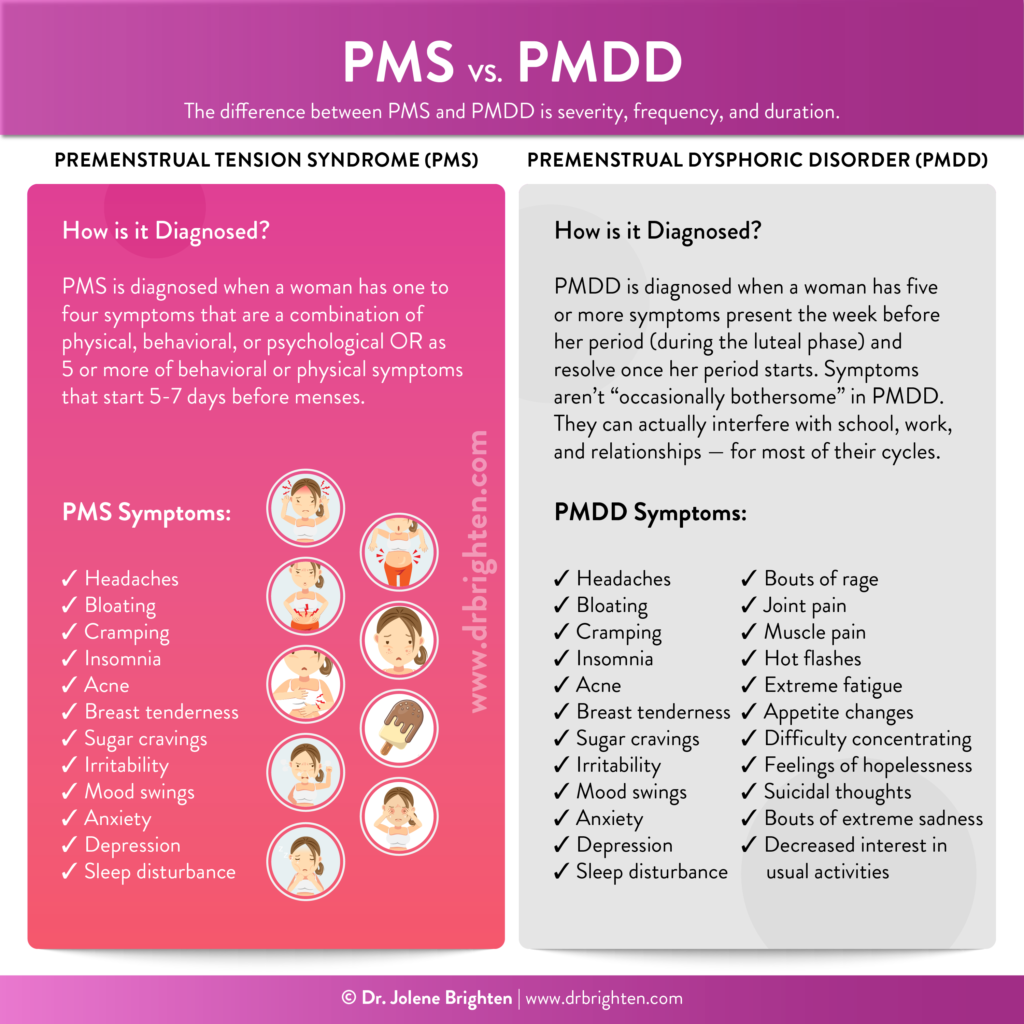
Differences Between PMDD and PMS
PMDD and PMS are related, but they have different symptom severities and impacts on daily life.
PMS involves milder symptoms that can cause discomfort but do not typically interfere with normal day-to-day life or activities. On the other hand, PMDD symptoms are more intense and can significantly disrupt functioning2 and relationships.
For a woman to be diagnosed with PMDD (more on those qualifications can be found here), her symptoms need to interfere with her ability to work, attend school, and tend to her family and other responsibilities. In other words, PMDD is like “PMS on steroids” because it's truly disruptive and life-altering.
PMDD Causes and Risk Factors
PMDD results from abnormal responses to hormonal fluctuations during the menstrual cycle, including fluctuating or high estrogen levels.
The brain is sensitive to sex hormones, including natural hormones, synthetic ones in birth control, and environmental xenoestrogens. Recent studies indicate that women with PMDD may have a genetic sensitivity3 to estrogen and progesterone that triggers extreme reactions to these hormones. The rate of PMDD among those who are neurodivergent suggest variations in the brain may play a role in sensitivity to these hormones.
Excess estrogen is one hormonal imbalance that's thought to be involved in PMDD. Estrogen can build up in the body when the liver does not process estrogen properly or the gut does not eliminate it well enough, resulting in a hyperestrogen state, also known as estrogen dominance, which may play a role in PMDD.
While genetics are believed to play a role in PMDD, environmental factors and lifestyle choices also influence hormone levels, genetic expression, and disease risk. For example, risk factors for PMDD include:
- Experiencing past trauma, including a history of sexual abuse.
- High stress levels.
- Low levels of serotonin4, a calming neurochemical.
- Being overweight or obese, which affects estrogen production in fat cells and can increase inflammation.
- Eating a low nutrient or ultra processed foods diet which can impair liver and gut health.
Connection Between ADHD and PMDD

If you have periods and are ADHD, you have much higher odds of experiencing PMDD. These two conditions have more overlap than most people realize, considering their root causes, including those involving neurotransmitters and hormones, are connected.
While research isn't entirely sure what exactly is behind this increased prevalence, here is what is currently thought to be contributing:
- Disruptions in neurotransmitter function – both serotonin and dopamine plays a significant role in the symptoms of ADHD and PMDD
- Hormonal fluctuations – there is an intimate relationship between cyclical hormones (estrogen and progesterone) and neurotransmitter generation and utilization
- Premenstrual estrogen decline – the natural decline in estrogen prior to menstruation is associated with more inattention and a decline in serotonin, which may contribute to adverse mood symptoms
Rates of ADHD among women have gone up considerably in recent years—due to both medicine finally recognizing the unique ways in which women present and more awareness. Studies suggest that people with ADHD may be more susceptible5 to experiencing PMDD symptoms—which makes sense, considering that both conditions involve neurotransmitter imbalances, hormonal fluctuations, and changes in brain function.
One study6 found that compared to the general public, a greater percentage of female ADHD patients suffer from significant PMDD symptoms, experience postpartum depression during the first childbirth, and experience more severe symptoms.
Findings from another study7 suggest that women with PMDD experience a greater increase in scores of memory problems and difficulties maintaining focused attention compared to women without PMDD throughout the cycle.
Symptoms of PMDD, such as mood swings, irritability, and difficulty concentrating, can also make ADHD symptoms even worse—and vice versa. This creates additional challenges in managing daily tasks and responsibilities.
Here's more about the underlying causes of ADHD and how they overlap with those of PMDD:
Disruptions in Neurotransmitter Function
PMDD and ADHD are both impacted by the neurotransmitters dopamine and serotonin, which play critical roles in mood regulation, attention, and emotional stability.
In ADHD, there is often dysregulation in dopamine8 signaling, which contributes to symptoms such as impulsivity, hyperactivity, and difficulty with focus and attention.
Similarly, PMDD is associated with fluctuations in both dopamine and serotonin levels throughout the menstrual cycle, leading to mood swings, irritability, and emotional instability, especially during the luteal phase9. Serotonin deficiency and low GABA levels, for example, can increase the risk for depression during the days leading up to one's period.
| Phase of Cycle | ADHD Symptoms | PMDD Symptoms |
| Period to Ovulation | Improved executive function, focus, memory | Resolution of PMDD specific symptoms |
| Ovulation to Period | Difficulty focusing, increased restlessness, executive function diminished | Increase mood swings, depression, lack of motivation, fatigue, body aches, breast tenderness, brain fog, etc |
Hormonal Fluctuations
Changes in estrogen and progesterone levels also influence ADHD and PMDD. Estrogen and progesterone impact neurotransmitter activity in the brain, and their fluctuations can exacerbate symptoms10 of both conditions.
For instance, changes in estrogen levels are thought to influence ADHD symptoms11 because estrogen raises neurotransmitter levels, including dopamine, that support focus, motivation, and attention.
Moreover, hormonal imbalances can affect brain function and cognition, contributing to difficulties in concentration, memory, and emotional regulation observed in both ADHD12 and PMDD. In the first half of the menstrual cycle, the follicular phase, estrogen rises, and neurotransmitters stabilize, often improving ADHD symptoms. But in the second half, the luteal phase after ovulation, progesterone increases, potentially worsening ADHD symptoms.
Women may feel more restless, struggle to focus and find tasks more challenging mid-cycle13 and before menstruation. Those with irregular cycles or both ADHD and PMDD may experience heightened symptoms due to unpredictable hormone fluctuations. Certain ADHD medications may even become less effective14 during times of hormonal fluctuation, including the luteal phase of the cycle, postpartum, and perimenopause, when estrogen levels drop and progesterone levels increase.
Some women with ADHD find relief through hormonal birth control15, which stabilizes fluctuations, although it may have side effects, so discussing the option with your provider and tracking your symptoms is important.
How to Manage PMDD

At this time, the FDA has only approved certain medications for the treatment of PMDD. Some of these are only used during the luteal phase or prior to anticipated symptoms or continuously, as is the case with oral contraceptives.
It is best to speak with your provider about managing PMDD symptoms, whether it be with medication or employing natural therapies. Understandably, not everyone wants to choose a pharmaceutical option, nor is everyone a good candidate. You will find additional information below on natural therapies that can be used to support yourself whether you are opting for medication or trying a different treatment route.
| Evidence Based Options for ADHD and PMDD | How to Implement |
| Nutrient Dense Diet | Calcium, vitamin E, B6, D, omega-3, and magnesium may prove to be particularly beneficial for those with PMDD. Use the free recipe guide here to help you get started. |
| Vitex agnus (Chaste tree berry) | Balance Women’s Hormone Support |
| Exercise | Aim for 150 minutes of moderate physical activity weekly or as advised by your medical provider. |
| Cognitive Behavioral Therapy | Meet with a trained mental health professional who has trained in the unique needs of ADHD |
| Pharmaceutical Therapy | Discuss the following with your licensed medical provider: – Oral contraceptive Pill – SSRIs |
| Stress Reduction | Tai chi, yoga, meditation, acupuncture, journaling |
| Rhodiola rosacea | Adrenal Support Note: avoid in cases of bipolar disorder diagnosis |
| Vitamin D | Sunlight exposure Foods: fatty fish, fortified foods, mushrooms Vitamin D3/K2 supplement |
| Limit Alcohol Intake | No alcohol is best. Otherwise, limit to no more than 1 drink per day16. |
| Omega-3 Fatty Acids | Eat cold water fish, walnuts, and other omega-3 food sources Omega Plus |
Medication Options to Treat PMDD
- Oral Birth Control Pills: The pill is often used to suppress brain-ovarian communication in order to stop the hormone fluctuations that happen over the course of the cycle. It replaces ovarian hormones with a consistent state of synthetic versions. While effective for some cases of PMDD, some women experience worsening symptoms. There are several conditions where the pill is contraindicated, such as with clotting disorders or migraines with aura, and in these instances, SSRIs are often the first line pharmaceutical treatment.
- Selective Serotonin Reuptake Inhibitors (SSRI): Fluoxetine (Sarafem), Paroxetine (Paxil), Sertraline (Zoloft) may be taken continuously, starting the 10-14 days before you expect your period, or from symptom onset until a few days after menses starts. It is important to discuss side effects and withdrawal symptoms with your provider before beginning.
- Serotonin-Norepinephrine Reuptake Inhibitor (SNRI): Venlafaxine is not recommended as first-line therapy since the side effects of discontinuing are worse than SSRIs and in some cases, the symptoms of PMDD.
Natural Support Options for PMDD and ADHD
Several natural remedies have been found to provide relief from PMDD symptoms, including by addressing hormonal and emotional imbalances. These include a healthy diet with plenty of fiber and protein, as well as supplements.
First and foremost, the best way to support estrogen and progesterone balance is to support your liver, ovaries, and digestive system with help from an anti-inflammatory, hormone-friendly diet. This type of diet includes lots of vegetables, fruits, and fiber from legumes, whole grains, nuts, and seeds.
I’ve put together a free recipe guide to help point you in the right direction.
Eating regular meals that support blood sugar balance can support regular energy, stable moods, and better sleep.
The Period Problems Kit™ is designed to give your liver, adrenals, and gut a helping hand in optimizing your hormones so you can feel your best all month long.
Consider trying these ingredients and supplements to help naturally support your hormones and brain health:
- Calcium: Essential for supporting mood stability and reducing anxiety symptoms commonly associated with PMDD. You’ll also find calcium, as well as other vitamins and minerals mentioned below, in my Women’s Twice Daily supplement and my Prenatal Plus formula.
- Vitamin E: Known for its ability to alleviate breast tenderness and mood swings, helping to improve overall emotional well-being during PMDD episodes.
- Vitex (Chasteberry): Supports hormone balance by influencing the pituitary gland, which can alleviate symptoms such as irritability, mood swings, and physical discomfort. You'll find chasteberry in my Balance Women’s Hormone Support formula, which also features polygonum, DIM, and calcium-D-glucarate to promote the proper elimination of excess estrogens.
- Magnesium: Promotes muscle relaxation, reduces bloating and cramping, and supports emotional stability by modulating neurotransmitters involved in mood regulation. I recommend choosing a supplement with magnesium bisglycinate, such as my Magnesium Plus capsules, as it is a highly absorbable form that doesn’t tend to cause digestive issues.
- Vitamin B6: Vitamin B6 plays a crucial role in serotonin production, regulating mood and potentially alleviating symptoms of depression and anxiety during PMDD episodes.
- Saffron: Demonstrates promise in reducing depressive symptoms17 associated with PMDD, possibly due to its mood-enhancing effects and ability to influence neurotransmitter activity in the brain.
In addition to a nutrient dense diet, the following have also been shown to be beneficial:
1. Cognitive Behavioral Therapy or Counseling
Cognitive behavioral therapy has been shown to be effective18 in addressing PMDD, especially in those that don’t experience relief from pharmaceuticals. It can be used as an adjunct therapy to pharmaceutical treatment or part of a more holistic plan.
It is very important that women with PMDD and ADHD seek solid mental health support from a knowledgeable therapist or counselor or even a support group of women going through the same thing. Not every mental health provider is going to be well versed in ADHD, so it can take time and multiple visits before you find someone that is best suited to help you.
Guided mental health support will help you develop healthy coping skills to cope with your symptoms and increase your awareness of lifestyle choices that may be making your symptoms worse. Additionally, educating yourself about ADHD and PMDD, including symptoms, triggers, and treatment options, empowers you to make informed decisions about your health.
2. Mindfulness and Stress Management Techniques
Practicing mindfulness, meditation, acupuncture, or yoga can significantly reduce stress levels, which is crucial for managing both ADHD and PMDD symptoms.
These techniques help regulate emotions, improve focus and memory, and enhance overall well-being by promoting relaxation and reducing the impact of hormonal fluctuations on mood and cognition. For example, acupuncture has been shown to reduce symptoms19 of PMS and PMDD by as much as 50% without any significant adverse side effects.
3. Rhodiola for ADHD Support
Rhodiola (or Rhodiola rosea) is an adaptogenic herb that may offer support for people with cognitive conditions20, including ADHD, by helping to improve focus, attention, and cognitive function. Some people report positive benefits throughout the cycle when taking this herb daily.
Adaptogens like Rhodiola are believed to help the body adapt to stress and maintain homeostasis (or balance). These effects may be especially helpful for those managing ADHD symptoms21 such as restlessness or anxiety, which are often related to stress22 or made worse by it.
As always, check in with your doctor about any herbs you’re considering and remember, natural therapies are not a direct replacement for medications.
Rhodiola's Effects on Dopamine
Rhodiola is thought to work by modulating neurotransmitters such as dopamine and serotonin, which play key roles in ADHD symptomatology.
Dopamine is crucial for motivation, reward processing, and executive function, all of which are commonly impaired in those with ADHD who struggle to prioritize tasks or plan far ahead. By increasing dopamine activity, Rhodiola may help enhance these cognitive processes23, leading to improved focus and attention.
Rhodiola's Impact on Serotonin
Additionally, rhodiola's effects on serotonin levels may contribute to its mood-regulating properties24, such as by promoting calmness. Serotonin plays a role in emotional stability and can influence mood swings and irritability, which are sometimes associated with ADHD as well as PMDD.
Help Balancing Energy and Reducing Fatigue
Finally, Rhodiola has been studied for its potential to reduce fatigue and improve energy levels, helping those who experience mental and physical exhaustion.
Its adaptogenic properties support adrenal function and may help regulate cortisol levels, helping to decrease stress and improving resilience to stressors that can contribute to ADHD symptoms.
Caution should be used in those diagnosed with bipolar disorder. There have been cases of mania in those taking very high doses of Rhodiola.
4. Regular Exercise
Engaging in regular physical activity, such as walking, jogging, or swimming, can alleviate symptoms of both ADHD and PMDD. Exercise releases endorphins, which improve mood and reduce anxiety and depression. It also promotes better sleep quality, boosts energy levels, and enhances overall physical health.
Many people with ADHD report better focus and concentration when engaging in regular exercise.
5. Establishing a Consistent Routine
Creating and maintaining a daily routine can provide structure and predictability, which is beneficial for individuals with ADHD and PMDD.
A consistent schedule for meals, sleep, work/study, and relaxation can help manage symptoms by reducing stress and improving time management skills. This stability can also support hormone balance and emotional stability throughout the menstrual cycle.
Routines are often one of the biggest challenges those with ADHD face. Here are some tips that I personally use to manage my ADHD and that have been effective with my patients:
- Create checklists that you print out and laminate. Place these in areas where you need to see them. For example, a checklist on the bathroom mirror may include brush teeth, floss, shower, brush hair, etc. It can feel silly, but we all need reminders sometimes and some people get a dopamine burst when they use a dry erase marker to check off these items.
- Break down the routine into bite size tasks. This is crucial when your executive functioning struggles during that luteal phase. I keep the mundane breakdown in my notes on my phone with a checklist. When my brain just doesn’t want to do it, I open the app and remind myself that if I can just do the smallest thing then I am making progress.
- Try to go to bed and wake at the same time. Using apps to set alarms, turn off wifi routers, turn on the bedroom lights and off the rest of the house, and even buying pajamas you’re really in love with can all help you on your way to this.
- Identify what motivates you. No joke, I have patients that thrive with sticker charts and I’m all for it. If you can identify your key motivators then you can hack that to get you onto a more consistent routine.
- Perfection is not that goal. You will absolutely fail if you think rigidity is the standard to which you should be measured. Giving yourself grace for those times when routines are especially difficult (um, yes this is PMDD time) is important.
6. Limiting Alcohol Intake and Examine Caffeine
Both caffeine and alcohol can exacerbate symptoms of PMDD. Caffeine can increase anxiety, disrupt sleep, and affect mood stability, while alcohol can interfere with medications and worsen hormonal imbalances. But for some people with ADHD, light to moderate caffeine intake improves their focus and concentration.
When it comes to alcohol, we know it won't support brain or hormone health. Caffeine, on the other hand, may prove to be a useful tool if you have ADHD. My advice to patients with ADHD and PMDD is to limit caffeinated beverages to one to two cups daily and monitor symptoms.

7. Sleep Hygiene Practices
Establishing good sleep hygiene practices, such as maintaining a regular sleep schedule, creating a relaxing bedtime routine, and ensuring a comfortable sleep environment, is essential for getting enough sleep (seven to nine hours per night) and managing ADHD and PMDD symptoms. Quality sleep supports cognitive function, emotional regulation, and hormone balance.
You can read more tips for addressing sleep problems before your period here.
8. Vitamin D and Omega-3 Fatty Acids
Omega-3 fatty acids, found in fish oil sources like salmon and sardines, provide DHA and EPA that support cell membranes and neurotransmitter function, reducing inflammation and benefiting mood and brain function. Research25 suggests they may also help improve behaviors associated with ADHD in some cases. For a reliable supplement, consider Omega Plus.
Vitamin D, crucial for sun-induced synthesis, may also help manage ADHD symptoms26, especially inattention. Supplementing is recommended for those with deficiency or limited sun exposure, ideally with a combination of vitamin D3 and vitamin K2 for added benefits.
ADHD and PMDD Next Steps:
Get the tools to heal your hormones and feel your best by exploring our articles:
- ADHD and Hormones: How to manage symptoms through your cycle
- Guide to Premenstrual Dysphoric Disorder
- How Hormones Affect Your Mood Throughout Your Period
- How Does Serotonin Affect Depression
- 18 Causes of Fatigue and How to Increase Energy
Key Takeaways on ADHD and PMDD
Understanding the complex interplay between ADHD and PMDD is helpful for managing symptoms and improving overall quality of life. If you deal with either ADHD or PMDD (or both), addressing neurotransmitter imbalances, hormonal fluctuations, and lifestyle factors can help you find relief. With the right support and treatment strategies, those with ADHD and PMDD can navigate their conditions more effectively and live more productive, fulfilling lives.
References
- https://pubmed.ncbi.nlm.nih.gov/30335340/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/37055419/ ↩︎
- https://www.nature.com/articles/mp2016229?error=cookies_not_supported&code=3bf183f6-38b1-4ca0-b25b-81bc8c73d9e8 ↩︎
- https://pubmed.ncbi.nlm.nih.gov/24158751/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/38836765/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/33302160/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/38836765/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/25092688/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/37055419/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/38152361/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/38039899/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/38039899/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/38678676/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/38152361/ ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7667464/ ↩︎
- https://www.prevention.va.gov/Healthy_Living/Limit_Alcohol.asp ↩︎
- https://www.researchgate.net/publication/346531707_Saffron_for_the_Management_of_Premenstrual_Dysphoric_Disorder_A_Randomized_Controlled_Trial ↩︎
- https://pubmed.ncbi.nlm.nih.gov/28419170/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/24410911/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/37627598/ ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4968082/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/35745023/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/32592534/ ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4757677/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/30594823/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/31368773/ ↩︎

