When you engage in consensual sex, you expect it to be a positive emotional experience leaving you feeling happy and relaxed. But when you feel sad after sex, you may wonder what is going on and if this is a normal or a common experience for women.
While most research on female sexual dysfunction focuses on what happens before or during sex, we are beginning to learn more about the emotional response that comes after sex.
You probably won’t hear about postcoital dysphoria, the “post-sex blues” from your average doctor and may be told it’s normal or just your hormones. But in truth PCD is something that should be explored. In this article, you’ll learn what post-coital dysphoria is, its prevalence, symptoms, causes, and the self-care strategies to use when you experience feeling sad after sex.
In this article:

What Is Post-Coital Dysphoria?
Postcoital dysphoria, also known as PCD or the “post sex blues,” is when you feel unexplainable negative emotions after a consensual and satisfactory sexual experience.
In PCD, the dysphoria always occurs after sex, not before or during, and may endure for over an hour. It can occur in committed, loving relationships, with a casual partner, or after masturbation. It can also happen whether an orgasm occurs or not.
PCD doesn’t correlate with the type of sex or amount of intimacy in a relationship. It’s not a sign that anything is wrong with the relationship.
Both men and women experience post-coital dysphoria, although it appears more common in women1.
Postcoital dysphoria can feel confusing, disorienting, and paradoxical. While we typically expect a feeling of well-being and positive emotions after sex, post-coital dysphoria may feel the opposite. It’s an underrecognized2, unresearched, and likely underreported condition.
Post-coital dysphoria is not the same thing as sexual abuse. It’s reasonable to be upset after sex if you felt forced or coerced into doing it—even by a spouse or partner. If you think you may have experienced sexual assault or abuse, call the National Sexual Assault Hotline at 1-800-656-4673 (24/7) for confidential support.
Is It Normal To Feel Sad After Sex?
Many people report experiencing negative emotions, including sadness, after sex.
In a 2015 survey3 of college students, 46% reported post-coital symptoms at least once in their lifetime, and 5.1% experienced symptoms in the previous month.
In a small 2020 survey4, including men and women, 94.3% of respondents experienced PCD at least once in their lifetime and 91.9% experienced symptoms in the past month.
It’s important to note that this study used a convenience sample where people elected to complete an online survey, compared to a random sample of the population. Still, the survey revealed that people experienced PCD symptoms after sexual activity (not including intercourse), intercourse, masturbation, and post-orgasm.
Other data5 suggests the overall prevalence of postcoital dysphoria symptoms between 14 and 34% in men and 33 to 43% for women, with symptoms experienced at some point during their lives and not necessarily consistently.
While it does seem quite common for women to experience PCD at some point in their lives, it doesn’t mean that you have to accept it as the way it’s going to be for you. Remember that common doesn’t mean normal and the cause should be investigated). If symptoms happen frequently and interfere with your quality of life or relationships, please discuss your experience with your doctor for support.
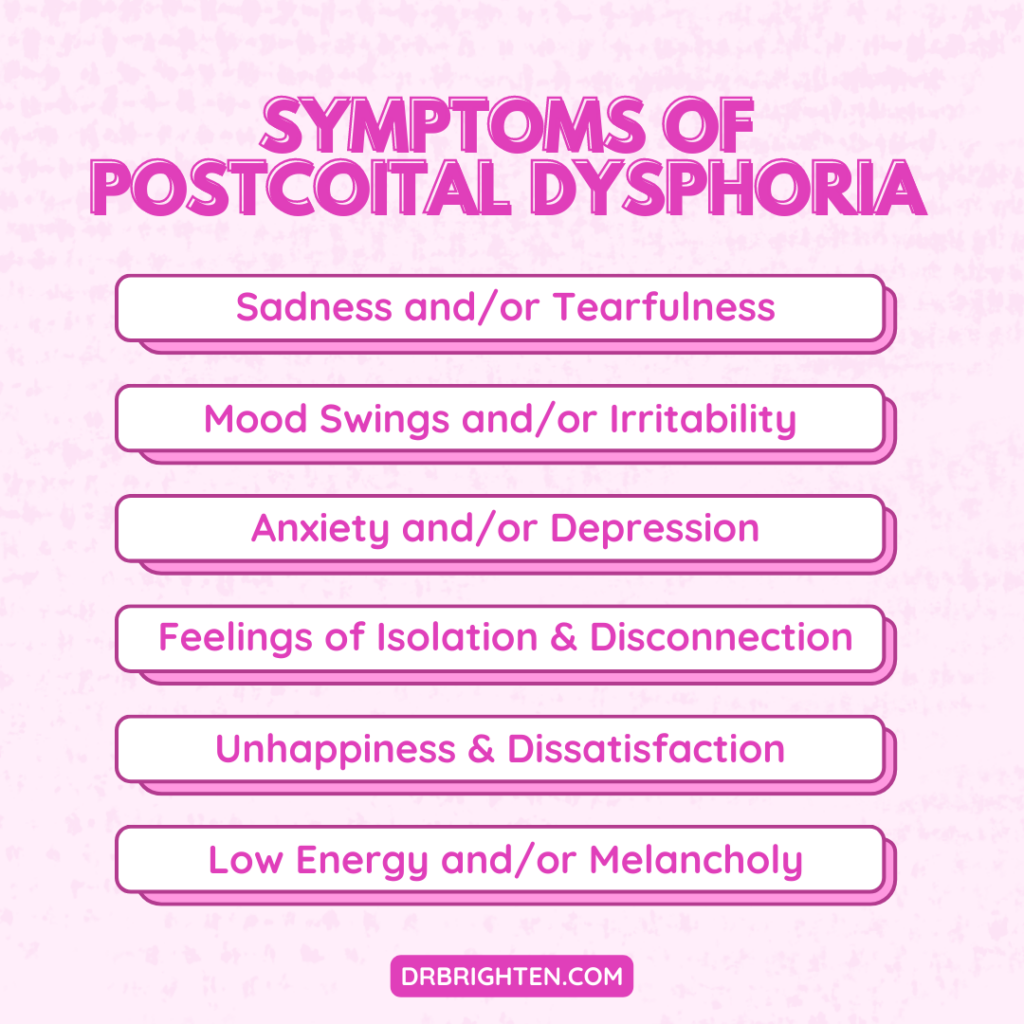
Postcoital Dysphoria Symptoms
PCD symptoms can be more varied than initially suggested and include broader symptoms than dysphoria. Some propose changing the name of the condition from postcoital dysphoria to postcoital symptoms.
PCD symptoms may include:
- Sadness
- Tearfulness
- Mood swings
- Irritability
- Depression
- Anxiety
- Feelings of isolation and disconnection
- Unhappiness and dissatisfaction
- Low energy
- Frustration
- Melancholy
- Agitation
- Aggression
- Desire to distance self from partner
Women are more likely to experience sadness and mood swings, while men report unhappiness and low energy as common symptoms during a PCD episode.
@drjolenebrighten Whether you’re struggling with perimenopause symptoms or looking to boost fertility, getting out into nature can help. It aids in lowering cortisol and increasing progesterone. This is one stress lowering tip you need to be leveraging. #hormonebalance #naturalhormonebalancing #naturetherapy #perimenopausehealth #fertilityjourney #hormonehealth #getoutside ♬ Sure Thing (sped up) – Miguel
Causes Of Post-Coital Dysphoria
I always ask the question why to get to the root causes of symptoms with patients. Here the appropriate question is: why do I feel sad after sex?
Although no research specifically looks at PCD and mental health, sexual dysfunction is more common among those with chronic stress or mood disturbances like anxiety and depression.
Possible postcoital dysphoria causes may include:
- Hormonal changes
- Neurotransmitter imbalances
- Mood disorders
- A history of sexual trauma
- Body image issues
- Feelings of shame toward sex
- Unmet emotional needs (need for aftercare, etc.)
Hormones Released During Sex
Sex and orgasm are associated with changes in the neuroendocrine system, including increased levels of certain hormones and neurotransmitters.
Hormones released during sex include oxytocin and prolactin.
Oxytocin is the hormone of love and connection. Levels rise with physical touch, sex, and orgasm. Releasing oxytocin makes you feel connected, lowers stress, and has many health benefits.
Prolactin is another hormone that surges after orgasm6. It supports feelings of satisfaction by controlling levels of dopamine and serotonin.
The dopamine surge experienced with sex is responsible for feelings of intense pleasure and reward. Serotonin promotes happiness and well-being.
These hormones and neurotransmitters naturally rise with sexual activity to make you feel good, but when you feel sad or down afterward, it’s possible that there may be a hormone or neurotransmitter imbalance at play.
For some people, the drop in hormone levels and subsequent withdrawal can trigger symptoms. If you feel depression after orgasm, it may be more of a withdrawal response.
Your naturopathic doctor can help with testing and support for hormone balance.
Past Trauma
It’s no secret that past trauma and abuse are related to increased sexual dysfunction compared to the general population. The same may be true for PCD.
In a study of 222 female university students7, 32.9% experienced PCD in their lifetime, while 10% experienced it in the previous month. The study found that the lifetime prevalence of PCD (but not the four-week prevalence) correlated with reports of childhood sexual abuse.
Keep in mind that correlation does not equal causation. Not everyone who has experienced trauma also experiences PCD, and not everyone who deals with PCD has had a traumatic past. But if you’ve experienced both, there might be something there. A trauma informed mental health professional can help you put the pieces together.
Body Image
Poor body image or body image disorders may also be a trigger or root cause for PCD symptoms. Feelings of anxiety and self-consciousness around your body lead to changes in the sexual experience.
Taking off your clothes and engaging in sex requires a high level of vulnerability. Afterward, you may experience a “vulnerability hangover.” This term, coined by researcher Brene Brown, describes a feeling of shame and other negative emotions after vulnerability and exposure in front of another person.
The Importance Of Aftercare
If you experience postcoital dysphoria, you may want to consider creating an aftercare ritual. Ask yourself what you need after sex to cope with symptoms you experience.
The goal of the ritual is to create a safe space where you can feel your feelings and allow them to pass. The ritual could include taking a bath, journaling, having your partner rub your back, or any other self-care strategies.
How To Deal With Postcoital Dysphoria
How to deal with post-coital dysphoria may depend on the woman’s symptoms and root causes. Strategies can be highly personalized.
First, I want to mention talking with your partner. Let your partner know what you need and how they can support you. It’s important to convey that your emotions aren’t a reflection of your partner or the sexual experience. You can share with them this article and the scientific studies referenced below.
In addition, please seek help when needed. Discuss your symptoms with a trusted friend, therapist, or doctor (or all three).
Self-Care
We already talked about the importance of an aftercare ritual, engaging in self-care immediately after sex. An overall self-care strategy may be supportive as well.
The basic self-care strategies include:
- Eating a nourishing, whole food diet
- Moving your body
- Managing stress
- Sleeping well
Consider these lifestyle pieces essential for hormonal balance, brain health, mood, and overall wellness. With this foundation, you can layer on additional strategies tailored to your symptoms and root causes.
Menstrual Cycle Tracking
I suggest tracking your menstrual cycle to understand if sex hormones, and hormonal changes during your cycle might be at play in terms of PCD symptoms. Note when you experience symptoms and their severity related to the phase of the menstrual cycle.
In my new book, Is This Normal, I take you through week-by-week how your hormones impact your sexual desire, arousal, and experiences. In it you’ll find a 28 day program to help you fine tune your hormones and uplevel your sex life.
Being able to answer questions like, do you experience more PCD symptoms in the luteal phase along with PMS symptoms, can help you understand the role your hormones play. Also note, do you notice a trend with symptoms during your period or around ovulation? It may take a few cycles to track and explore this connection but gathering information will be very helpful.
For review, here is information on how the menstrual cycle works and the phases of the menstrual cycle.
Balancing Hormones
Since PCD symptoms may stem from a hormonal imbalance, supporting hormone balance is always a good idea. Here are some of my go-to supplements to incorporate along with eating a nourishing diet and implementing an active, low-stress lifestyle.
@drjolenebrighten Would you drink this? Leave me a comment if you try it. #TodayILearned #tiktokpartner #learnontiktok #hormoneimbalance #pms #pmsproblems #hormones #latinx ♬ original sound – Dr. Jolene Brighten
Magnesium
Magnesium is a critical mineral that supports hormone balance, mood support, energy production, heart function, bone health, and much more. Yet, most Americans are only getting about 50%8 of their daily magnesium needs through their diet alone.
The standard American diet is low in magnesium-rich foods, including leafy greens, nuts, legumes, and avocados. In addition, modern agriculture practices have depleted mineral levels in the soil, so magnesium levels in whole foods are even lower than they once were.
For these reasons, a magnesium supplement makes sense for many people, including women working to improve hormone levels, mood, and symptoms of postcoital dysphoria.
Magnesium supplements are incredibly safe, even at high dosages, and support hundreds of enzymatic processes in the body.
Magnesium Plus offers 300mg of highly absorbable, chelated magnesium per serving. Magnesium bisglycinate is magnesium attached to the amino acid glycine, which helps to calm the nervous system.
I recommend taking magnesium at night to promote relaxation and sleep.
B Vitamins
We can’t talk about hormonal health and mood symptoms without thinking about B vitamins, which are vital for metabolism, neurotransmitter production, brain function, hormone production, hormone detoxification, and so much more.
It can be challenging to meet B vitamins needs in the diet, and many of us require higher amounts simply because of stress levels as stress depletes these essential nutrients.
You get supplemental B vitamins when you take a multivitamin or prenatal. You can also take additional B vitamins in a B vitamin complex, such as B-Active Plus, which contains the active forms of these nutrients.
I recommend taking B vitamins early in the day as they can be stimulating.
Natural Herbs
Herbal medicine is an incredible tool for supporting hormone balance in a gentle and effective way.
Balance—Women's Hormone Support is my favorite comprehensive formula for supporting women’s hormones. It contains essential nutrients, herbs, and plant extracts to harmonize hormones and support a variety of issues.
Takeaway
PCD affects many women at one point or the other. Symptoms are a powerful messenger of something deeper that needs to be explored. Whether it’s working to improve body image issues, moving past patterns of trauma, or addressing hormonal balance, understanding the root causes can help you move past the bewildering symptoms of PCD.
Talking with your partner and healthcare team, implementing self-care and aftercare rituals, and supporting hormonal health with supplements and lifestyle changes are some places to start.
References
- https://pubmed.ncbi.nlm.nih.gov/36447696/ ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4721025/ ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4721025/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/31937518/ ↩︎
- https://www.tandfonline.com/doi/full/10.1080/19317611.2010.509689 ↩︎
- https://pubmed.ncbi.nlm.nih.gov/23014134/ ↩︎
- https://www.tandfonline.com/doi/full/10.1080/19317611.2010.509689 ↩︎
- https://lpi.oregonstate.edu/mic/micronutrient-inadequacies/overview ↩︎
