If you’re a woman navigating both menopause and an autoimmune disease at the same time, you might have noticed your symptoms shifting in ways your doctor didn’t fully prepare you for.
For example, unpredictable flare-ups, stubborn signs of inflammation, and hormonal chaos can all occur during this transitional phase and can feel like a storm no one warned you about.
Below, we'll unpack what’s really going on beneath the surface if you're a woman in menopause with an autoimmune condition (or you suspect you might be), and what you can do about it.
In this article:
- Quick Summary: What to Know About Menopause and Autoimmune Disease
- What Is Autoimmune Disease and Why It Affects Women Differently?
- Can Menopause Trigger Autoimmune Flares and Inflammation?
- Why Autoimmune Flares Often Get Worse in Perimenopause and What to Do
- What Happens to Autoimmune Conditions During Menopause?
- Essential Tests for Women with Autoimmune Disease in Menopause
- How to Manage Autoimmune Disease in Menopause with Diet, Lifestyle, and Supplements
- Frequently Asked Questions: Menopause and Autoimmune Disease in Women
- Final Thoughts on Managing Menopause in Women with Autoimmune Disease
Quick Summary: What to Know About Menopause and Autoimmune Disease
- 80% of autoimmune disease cases affect women, and hormone shifts during perimenopause and menopause can worsen or trigger symptoms.
- Common symptoms like fatigue, brain fog, joint pain, and mood swings may be mistaken for menopause alone, but they could signal immune dysfunction.
- Estrogen and progesterone protect immune balance and their decline increases inflammation, gut permeability (“leaky gut”), and immune dysregulation.
- Conditions like Hashimoto’s, lupus, rheumatoid arthritis, MS, and endometriosis are all influenced by menopausal hormone changes.
- You may experience new flares, increased pain, worsened fatigue, or medication resistance during this transition—even if your condition was previously stable.
- Conventional care often misses the autoimmune-menopause connection, leaving women unprepared and unsupported.
- Hormone replacement therapy (HRT) may help, but it must be customized, especially for autoimmune patients.
- Testing is key: Ask for thyroid hormones, antibodies, inflammatory markers, and sex hormone levels to uncover hidden causes of symptoms.
- Diet, nervous system support, blood sugar balance, and targeted supplements (like Omega-3s, magnesium, curcumin, vitamin D, and B vitamins) are essential tools.
- You’re not imagining it. Menopause and autoimmunity intersect in real, physiological ways and there’s a path forward.
What Is Autoimmune Disease and Why It Affects Women Differently?
Autoimmune diseases occur when your immune system mistakenly attacks your own body. Instead of protecting you from foreign invaders (like pathogens), your immune system turns its firepower on your own healthy tissues, organs, and glands.
Overall, autoimmune diseases are estimated to affect about 7% of the general population, with most cases occurring in women, and rank among the 10 leading causes of death among women1 under age 75 years.
Common autoimmune conditions include:
- Hashimoto’s thyroiditis, a thyroid gland autoimmune disorder and a type of hypothyroidism
- Lupus, a systemic autoimmune disease that can impact multiple organs
- Rheumatoid arthritis, an autoimmune arthritis marked by joint damage and pain
- Multiple sclerosis, an autoimmune attack on the nervous system itself
- Psoriasis and eczema, which affect the skin and can cause dryness, sensitivity, and redness
- Celiac disease, an allergy to gluten, which is found in grains like wheat and barley
- Crohn's disease, a type of inflammatory condition affecting the gut and digestive tract
- Endometriosis, which is not officially classified as an autoimmune disease, endometriosis but exhibits autoimmune and inflammatory characteristics. The immune system fails to clear endometrial-like tissue that grows outside the uterus, leading to chronic pelvic pain, inflammation, and sometimes infertility
These autoimmune conditions are far more common in females, especially those of reproductive age. In fact, around 80% of all autoimmune patients are female2. 9 out of 10 cases3 of lupus affect women, and other autoimmune conditions, including sclerosis and rheumatoid arthritis, affect 3x to 4x more women4 than men.
Why are women more prone to autoimmune conditions? Hormones are a big piece of the puzzle. For instance, studies show that hormone shifts during menopause (especially lower estrogen levels) can often trigger autoimmune symptoms5 and make them more severe.
Related: The Autoimmune Hormone Connection
What Are the Early Signs of Autoimmune Disease in Women?
What types of symptoms do autoimmune conditions cause?
Symptoms of autoimmune diseases vary by condition and can include:
- Chronic fatigue
- Brain fog
- Joint or muscle pain
- Digestive problems
- Rashes or skin issues
- Autoimmune disease hair loss
- Sensitivity to cold, heat, or sunlight
Related: 10 Odd Symptoms of Menopause and Connection Between Gut Health, Menopause, and Perimenopause

Can Menopause Trigger Autoimmune Flares and Inflammation?
Can menopause cause inflammation? Yes, and for women with autoimmune conditions, that matters a lot.
Menopause is already a big shift. But if you're one of the millions of women living with an autoimmune condition, your symptoms might intensify, change, or become harder to manage during the perimenopause and menopause transition.
Unfortunately, most conventional care doesn’t prepare women for how autoimmune disease and menopause interact. You're left wondering why your joints suddenly hurt more, your fatigue has deepened, or your thyroid medication doesn't seem to be working like it used to. So let’s talk about what’s really happening during this stage…
How Estrogen Decline Worsens Autoimmune Disease During Menopause:
Estrogen is more than a reproductive hormone; it also plays a protective role in the immune system6 and immune modulation. As estrogen declines during perimenopause and menopause, your immune system becomes more dysregulated. Lower estrogen can tip the body toward having heightened inflammatory responses7.
For example:
- Estrogen helps control inflammatory messengers, including cytokines8, which are involved in immune activity. Without enough estrogen, these messengers can become overactive, worsening autoimmune flares.
- Menopause shifts the Th1/Th2 immune balance, making some autoimmune diseases worse (like rheumatoid arthritis or multiple sclerosis) while others might possibly stabilize.
- Declining estrogen and progesterone can also contribute to gut permeability9, often called “leaky gut,” which is a known trigger for inflammation and autoimmune reactions.
Related: Complex Trauma, Cortisol Chaos & the Autoimmune Connection with Justin Janoska
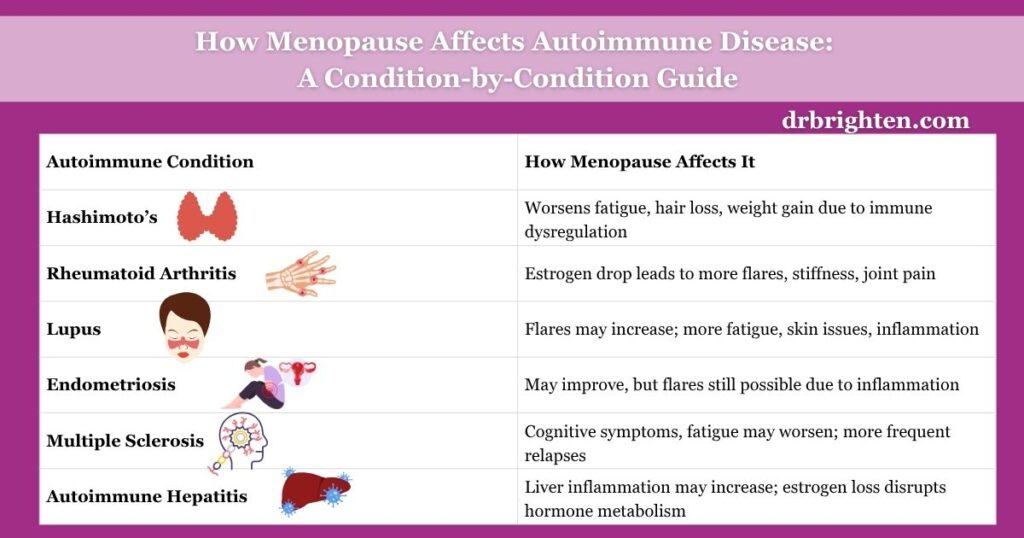
How Menopause Affects Common Autoimmune Conditions
| Condition | Impact of Menopause | Suggested Support |
| Hashimoto’s | May worsen symptoms and increase fatigue | Adjust thyroid meds, support with selenium & myo-inositol |
| Rheumatoid Arthritis | Often flares due to estrogen drop | Omega-3s, HRT discussion, anti-inflammatory diet |
| Lupus | Flares can increase | Vitamin D, adrenal support, liver detox pathways |
| Endometriosis | May improve, but flares still possible | Nervous system support, inflammation-focused protocols, NAC |
| Multiple Sclerosis (MS) | Symptoms may worsen | Sleep optimization, HRT, magnesium, B vitamins |
Why Autoimmune Flares Often Get Worse in Perimenopause and What to Do
Perimenopause—the transitional phase before your period stops for good—can last for several years and is basically a hormonal rollercoaster. Estrogen and progesterone swing wildly, which can aggravate symptoms tied to increased inflammation, like joint pain, mood issues, and fatigue.
The result? Even if your autoimmune condition was stable before perimenopause, it can flare unexpectedly, or you might even be newly diagnosed with an autoimmune disease during this time.
For women who are prone to developing autoimmune conditions, perimenopause can lead to:
- Unpredictable immune activity: One week your body is calm, the next it’s launching an inflammatory attack.
- Poor sleep and cortisol spikes: Sleep disruption increases stress hormones, which usually worsen inflammation.
- Increased gut permeability (“leaky gut”): Hormonal shifts can weaken the gut lining, contributing to flare-ups.
- Mood instability: It's common for depression and anxiety to worsen with both menopause and autoimmune disease.
What Happens to Autoimmune Conditions During Menopause?
Menopause can affect different autoimmune conditions10 in very different ways because each autoimmune disease interacts uniquely with hormone levels, inflammation, and immune signaling.
Hormonal shifts of menopause act as either a trigger or a tipping point, depending on the condition and how your body responds to immune and endocrine changes.
Here's more about what typically happens during menopause with different autoimmune conditions:
Hashimoto’s Thyroiditis and Hypothyroidism:
One of the most common autoimmune diseases in women is Hashimoto’s, which affects the thyroid gland and often leads to low thyroid hormone levels.
Hashimoto’s thyroiditis often worsens in menopause due to declining estrogen and increased immune dysregulation.
During menopause, your thyroid needs may shift, sometimes requiring adjusted medication doses. Plus, symptoms like fatigue, weight gain, and mood swings can be mistaken for menopause alone when they’re really thyroid-related.
Hashimoto’s hair loss also tends to worsen during menopause due to combined hormonal and autoimmune changes.
What are the best Hashimoto’s supplements? These can include selenium, myo-inositol, zinc, and Omega Plus to support inflammation and thyroid hormone conversion.
Common Symptoms of Hashimoto’s Thyroiditis
Hashimoto’s thyroiditis is an autoimmune disease that affects the thyroid gland and often leads to hypothyroidism. Many of its symptoms overlap with menopause, which can make it difficult to recognize during perimenopause or after.
Common symptoms of Hashimoto’s include:
- Chronic fatigue that doesn’t improve with rest or sleep
- Unexplained weight gain, even with regular diet and exercise
- Hair thinning or hair loss, especially at the crown or outer eyebrows
- Cold intolerance or feeling cold when others are comfortable
- Constipation and slower digestion
- Brain fog and trouble with memory, focus, or concentration
- Depression or low mood that seems hormonal but persists
- Dry skin and brittle nails
- Menstrual irregularities or heavier-than-normal periods
- Puffy face or swelling in the neck (enlarged thyroid or goiter)
These symptoms may worsen or change during menopause, especially as estrogen and progesterone decline. If you’re experiencing several of these symptoms, ask your doctor for a thyroid panel and antibody testing (see the FAQ section of this article for the exact tests) to rule out or confirm Hashimoto’s.

Rheumatoid Arthritis (RA):
Rheumatoid arthritis symptoms can temporarily improve during pregnancy (due to high estrogen), but worsen again after menopause. Rheumatoid arthritis (RA) often flares during perimenopause and early menopause because estrogen normally protects joints, so when it declines, joint pain and stiffness can become more intense.
Women with RA can also experience more fatigue and swelling. Rheumatoid arthritis and lupus can overlap in symptoms, and both can worsen during menopause.
Common Symptoms of Rheumatoid Arthritis (RA)
Rheumatoid arthritis (RA) is a chronic autoimmune disease that causes the immune system to attack the joints, leading to pain, inflammation, and progressive joint damage. Symptoms can become more noticeable or severe during perimenopause and menopause due to hormonal shifts and increased inflammation.
Common symptoms of rheumatoid arthritis include:
- Joint pain that is symmetrical (affecting both sides of the body)
- Morning stiffness that lasts longer than 30 minutes
- Swollen joints, especially in the hands, wrists, and knees
- Fatigue and low energy that feels constant or unrelenting
- Warm or tender joints, particularly after periods of rest
- Reduced range of motion or difficulty with fine motor tasks
- Muscle aches that are not related to exercise or injury
- Low-grade fevers or flu-like symptoms that come and go
- Weight loss that is unintentional and accompanied by fatigue
- Depression or mood changes, often related to chronic pain
During menopause, the loss of estrogen’s protective effects can make RA symptoms worse. Joint pain, swelling, and fatigue may increase, and some women experience new RA diagnoses during perimenopause due to immune shifts.If you suspect rheumatoid arthritis, ask your doctor for testing including rheumatoid factor (RF), anti-CCP antibodies, CRP, and ESR to evaluate inflammation and confirm diagnosis.
Lupus and Autoimmune Hepatitis:
Lupus is a complex autoimmune disease that affects multiple organs. Like other autoimmune diseases, it can flare due to hormonal shifts. Many women report increased fatigue, skin rashes, and even autoimmune hepatitis symptoms as they enter menopause. Lupus flares can become more frequent or severe as hormonal fluctuations cease and inflammation increases.
Common Symptoms of Lupus in Women
Lupus (systemic lupus erythematosus or SLE) is a complex autoimmune disease in which the immune system attacks healthy tissues, often affecting the skin, joints, kidneys, heart, lungs, brain, and blood cells. It’s more common in women, especially during hormonal transitions like perimenopause and menopause, when symptoms may worsen or become harder to manage.
Common symptoms of lupus include:
- Chronic fatigue that is not improved by rest
- Joint pain and swelling, especially in the hands, wrists, and knees
- Butterfly-shaped rash across the cheeks and nose (malar rash)
- Photosensitivity, or heightened sensitivity to sunlight
- Hair loss, often in patches or with overall thinning
- Low-grade fevers that come and go without infection
- Chest pain when breathing deeply (pleuritis or pericarditis)
- Mouth or nose ulcers that don’t heal easily
- Brain fog, memory issues, or difficulty concentrating
- Anxiety and depression, often linked to inflammation and chronic illness
- Raynaud’s phenomenon, where fingers or toes turn white or blue in response to cold or stress
- Kidney issues or swelling in the legs, ankles, or around the eyes
During menopause, the drop in estrogen can increase inflammatory pathways and disrupt immune regulation, potentially leading to lupus flares. Some women also report new lupus symptoms appearing in the menopausal transition due to heightened immune dysregulation and cortisol disruption from poor sleep.
If you suspect lupus, ask your doctor about testing for ANA (antinuclear antibodies), anti-dsDNA, anti-Smith, CRP, ESR, and kidney function markers.
Common Symptoms of Autoimmune Hepatitis
Autoimmune hepatitis is a chronic inflammatory liver disease where the immune system mistakenly attacks liver cells, leading to liver inflammation and, over time, possible scarring (cirrhosis). It affects women far more often than men and may flare or become newly diagnosed during perimenopause or menopause due to hormone-driven immune shifts.
Common symptoms of autoimmune hepatitis include:
- Fatigue that feels persistent and unrelieved by sleep
- Joint pain or aches, especially without visible swelling
- Upper right abdominal discomfort or tenderness near the liver
- Jaundice, or yellowing of the skin and eyes
- Dark-colored urine or light/clay-colored stools
- Unexplained nausea or loss of appetite
- Itchy skin (pruritus), even without a rash
- Spider veins or visible blood vessels on the skin
- Menstrual irregularities or missed periods (especially in premenopausal women)
- Brain fog or difficulty concentrating (hepatic encephalopathy in severe cases)
- Swelling in the legs or abdomen (in advanced liver disease)
During menopause, lower levels of estrogen and progesterone may disrupt immune regulation, increasing the risk of autoimmune flare-ups affecting the liver. Additionally, liver function plays a key role in hormone metabolism, so symptoms may be compounded by hormonal imbalances.
If autoimmune hepatitis is suspected, request testing for:
- Liver enzymes (ALT, AST, ALP, GGT)
- Bilirubin and albumin levels
- ANA, SMA, and LKM antibodies (autoimmune liver markers)
- IgG levels
- Liver ultrasound or elastography, if needed
Endometriosis:
Although not always classified as autoimmune, endometriosis behaves like one, with inflammatory tissue growing outside the uterus, often triggering pain and immune reactions.
Menopause typically reduces estrogen levels, which can shrink endo lesions and improve symptoms for many women. But the transition can still include endo flares for some women, such as those with estrogen dominance and high levels of inflammation. That’s why supporting your immune system and nervous system during this time is key.
If you have endometriosis, my Endo Flare Tool Kit can help, which is full of strategies to help calm inflammation and regulate hormones.
Common Symptoms of Endometriosis
Endometriosis is a chronic, inflammatory condition in which tissue similar to the uterine lining grows outside the uterus. While not officially classified as an autoimmune disease, endometriosis shares many immune system dysfunctions and inflammatory pathways seen in autoimmunity. Symptoms often shift during perimenopause and menopause, especially in women with high estrogen or unresolved immune triggers.
Common symptoms of endometriosis include:
- Chronic pelvic pain, especially before or during menstruation
- Painful periods (dysmenorrhea) that interfere with daily activities
- Pain during sex (dyspareunia), particularly with deep penetration
- Pain with bowel movements or urination, especially during menstruation
- Heavy menstrual bleeding or bleeding between periods
- Digestive issues, including bloating, constipation, or diarrhea (often misdiagnosed as IBS)
- Fatigue, especially around the menstrual cycle
- Infertility or difficulty conceiving
- Lower back or leg pain that worsens with your cycle
- Mood swings, anxiety, or depression tied to chronic pain and hormone imbalances
Although estrogen levels decline in menopause—which can shrink endo lesions and relieve symptoms—some women still experience endometriosis flares due to lingering inflammation, hormone imbalances (like estrogen dominance), or HRT that isn’t properly balanced.
If you have endometriosis or suspect it, talk to your doctor about:
- Pelvic ultrasound or MRI
- Laparoscopy
- Hormone testing (estrogen, progesterone, LH/FSH)
- Inflammation markers (CRP, ESR)
- GI testing if digestive symptoms are prominent
Menopause does not always resolve endometriosis symptoms and in some women, HRT or immune dysregulation can reignite them. Targeted support for gut health, stress reduction, and immune balance is key.

Multiple Sclerosis:
During menopause, many women with multiple sclerosis (MS) notice changes in their symptoms, and not always for the better. As estrogen declines, so does its protective effect on the nervous system, which can lead to increased inflammation, worsened fatigue, and a potential acceleration of disease progression.
Some women with MS also report more frequent relapses or a shift in cognitive symptoms. Additionally, sleep disruptions, hot flashes, and mood changes common in menopause can further complicate MS and make it harder to manage.
Common Symptoms of Multiple Sclerosis (MS)
Multiple sclerosis (MS) is a chronic autoimmune condition where the immune system attacks the protective covering (myelin) of nerve fibers in the central nervous system, leading to communication disruptions between the brain and body. It is more common in women, and symptoms often shift or worsen during perimenopause and menopause, when estrogen—a neuroprotective hormone—declines.
Common symptoms of multiple sclerosis include:
- Fatigue, often described as overwhelming or “bone-deep”
- Numbness or tingling, especially in the face, arms, legs, or torso
- Muscle weakness or loss of coordination in one or more limbs
- Balance problems or dizziness (vertigo-like symptoms)
- Blurred or double vision, sometimes with eye pain (optic neuritis)
- Brain fog, memory lapses, or slowed cognitive processing
- Bladder or bowel dysfunction, including urgency or incontinence
- Muscle stiffness or spasms (spasticity), especially in the legs
- Depression or mood swings, sometimes unrelated to situational stress
- Heat sensitivity, which can temporarily worsen symptoms (Uhthoff’s phenomenon)
- Speech or swallowing difficulties, in more advanced stages
During menopause, many women with MS notice a worsening of fatigue, cognitive symptoms, and sleep disruption, partly due to estrogen’s withdrawal and increased inflammation. Hormone loss may also accelerate disease progression or increase the frequency of relapses in some individuals.
If you’re navigating MS and menopause, ask your provider about:
- Brain and spinal MRI (to track lesion activity)
- Vitamin D levels (deficiency is linked to MS flares)
- Hormone panel (estradiol, progesterone, cortisol)
- Cognitive assessments if mental clarity or memory are concerns
- DMT (disease-modifying therapy) optimization, as HRT may influence how you respond to certain medications
Supporting nervous system resilience, stress regulation, and sleep quality is especially important for women with MS during the menopausal transition.

Essential Tests for Women with Autoimmune Disease in Menopause
If you're going through menopause and have an autoimmune disease (or suspect you might), ask your provider about testing that includes:
- TSH, free T3, and free T4 (thyroid panel)
- Thyroid antibodies (TPO and TgAb for Hashimoto’s)
- ANA and rheumatoid factor (for lupus and RA)
- CRP and ESR (markers of inflammation)
- Vitamin D, B12, and ferritin (common deficiencies with autoimmunity)
- Hormone panel (estradiol, progesterone, DHEA, cortisol)
These tests can help identify both hormonal imbalances and autoimmune markers, so you’re not chasing symptoms in the dark.
How to Manage Autoimmune Disease in Menopause with Diet, Lifestyle, and Supplements
While hormone replacement therapy (HRT) can be part of your treatment plan, foundational lifestyle strategies are key for managing autoimmune diseases long-term and reducing menopause-related inflammation. Here’s what helps:
- Eat an anti-inflammatory diet
- Support adrenal and nervous system health
- Balance your blood sugar
- Consider supplements for immune support
1. What Should You Eat to Reduce Autoimmune Flares During Menopause?
Include plenty of leafy greens, berries, wild salmon, olive oil, and fresh veggies in your diet. These foods are high in antioxidants, fiber, and essential vitamins and minerals that support your immune system.
Reduce your intake of processed foods, added sugars, and inflammatory oils (like refined vegetable oils such as safflower and sunflower oil that are found in many packaged foods). Consider removing gluten and dairy if you have autoimmune symptoms like bloating, brain fog, or autoimmune disease hair loss.
Additionally, you can add supplements to your routine to help keep inflammation under control. Omega Plus is a great way to support anti-inflammatory pathways if you're not eating fatty fish regularly. Omega Plus delivers 1600 mg of EPA and DHA per serving and includes lipase, an enzyme added to support comfortable digestion.
Related: 7 Reasons Why I Prescribe Bone Broth for Autoimmune Disease

2. How Stress and Cortisol Affect Autoimmune Symptoms in Menopause
Stress (which leads to high cortisol) is a major trigger for autoimmune flares and hormonal imbalance. Do whatever you can to manage stress and support your nervous system, such as exercising, meditating, and spending time in nature.
Consider practicing gentle exercise like walking, stretching, or yoga most days of the week. Try breathwork, reading, or journaling instead of scrolling on your phone.
You can also supplement with Magnesium Plus to promote calm, support sleep, and regulate your stress responses. Magnesium Plus contains a bioavailable form of magnesium in an easy-to-take capsule. This mineral supports hundreds of biological processes and is often included in wellness protocols for overall balance, including among women navigating hormonal shifts.
3. How Blood Sugar Imbalance Triggers Autoimmune Flares and Hormone Chaos
Stable blood sugar means more stable hormones and less immune overactivation.
- Make a point to eat enough protein, fiber, and healthy fats with every meal. Avoid long gaps between meals (especially in perimenopause).
- Avoid added sugars, sugary drinks, and refined grains. You can also add cinnamon, apple cider vinegar, or chromium-rich foods to your diet for extra support.
4. Top Supplements to Manage Autoimmune Disease and Hormonal Fluctuations
These supplements can often help reduce inflammation and regulate immune activity:
- Omega-3s (like Omega Plus): Omega-3 fatty acids can help lower inflammation11 and support hormone balance, including during and after menopause, which may ease joint pain and immune flare-ups.
- Magnesium: Magnesium supports adrenal and nervous system function, reduces stress-related inflammation12, and may ease hot flashes and muscle tension in menopause.
- Curcumin: As the active compound in turmeric, curcumin helps regulate immune activity and can help reduce systemic inflammation13, which is linked to autoimmune flares and menopausal symptoms.
- Vitamin D: Vitamin D is an important player in immune regulation and can help prevent worsening autoimmune symptoms14 and mood issues during menopause.
- B vitamins: B vitamins support energy, cognitive function15, and methylation pathways involved in hormone metabolism and immune health.
- NAC or glutathione: These antioxidants help protect cells from oxidative stress16, support liver detox pathways, and help reduce inflammation common in autoimmune and menopausal conditions.
- Myo-inositol and selenium: This combination helps improve thyroid function17, support hormone balance, and reduce autoantibody levels in conditions like Hashimoto’s.
It's best to work with a provider to customize your plan, especially if you take medications and are actively managing an autoimmune condition.
Related: Low-Dose Naltrexone for Women’s Health: Benefits for Hormones, Autoimmunity, and Chronic Pain

Frequently Asked Questions: Menopause and Autoimmune Disease in Women
Menopause can worsen autoimmune conditions due to the decline in estrogen and progesterone. These hormones play important roles in regulating immune function and controlling inflammation. As they drop, many women experience increased flare-ups, joint pain, fatigue, mood changes, and new or intensified symptoms of existing autoimmune diseases like Hashimoto’s, lupus, and rheumatoid arthritis.
Yes, perimenopause and menopause can act as a trigger for the onset of autoimmune disease in women who are genetically predisposed or already showing signs of immune dysfunction. Hormonal chaos, poor sleep, gut issues, and rising cortisol can all contribute to immune dysregulation that leads to a diagnosis during this life stage.
Roughly 80% of autoimmune patients are women. Female hormones—especially estrogen—modulate immune responses, and this interaction makes women more susceptible. Hormonal transitions like puberty, pregnancy, and menopause are common windows when autoimmune conditions are diagnosed or worsen.
During perimenopause and menopause, the following autoimmune symptoms often intensify:
– Chronic fatigue
– Brain fog
– Muscle and joint pain
– Skin rashes or irritation
– Hair loss (especially with Hashimoto’s)
– Digestive issues
– Mood swings or depression
These overlaps can make it hard to separate what’s caused by menopause versus autoimmune disease without proper testing.
The most affected autoimmune conditions during menopause include:
– Hashimoto’s thyroiditis (more fatigue, hair loss, weight gain)
– Rheumatoid arthritis (increased joint pain and stiffness)
– Lupus (more frequent or severe flares)
– Multiple sclerosis (increased fatigue and cognitive issues)
– Endometriosis (can still flare despite estrogen decline)
In some cases, bioidentical hormone replacement therapy (HRT) can help by restoring estrogen and progesterone levels, which reduces inflammation and stabilizes the immune system. However, HRT is not a one-size-fits-all solution and should be personalized, especially if you have an autoimmune condition.
Yes. Inflammation often increases during perimenopause due to fluctuating estrogen levels, rising cortisol from sleep disturbances, and gut permeability changes (“leaky gut”). This can exacerbate existing autoimmune symptoms or trigger new ones.
Ask your provider to check:
– Thyroid panel: TSH, Free T3, Free T4
– Thyroid antibodies: TPO, TgAb
– Autoimmune markers: ANA, rheumatoid factor
– Inflammation markers: CRP, ESR
– Nutrient status: Vitamin D, B12, ferritin
– Hormone panel: Estradiol, progesterone, DHEA, cortisol
These labs help identify hidden imbalances contributing to flares or unresolved symptoms.
To reduce inflammation and flare-ups during menopause:
– Eat an anti-inflammatory diet rich in omega-3s, leafy greens, and colorful vegetables
– Balance blood sugar with protein, fiber, and healthy fats
– Support your nervous system with stress-reducing practices like yoga, walking, and breathwork
– Take targeted supplements (e.g., Omega-3s, magnesium, curcumin, B vitamins)
– Work with a provider to evaluate HRT and medication needs
Helpful supplements include:
– Omega-3s (like Omega Plus): reduce inflammation
– Magnesium: supports sleep, mood, stress resilience
– Vitamin D: immune modulator, protects against mood issues
– Curcumin: anti-inflammatory and immune balancing
– Myo-inositol + selenium: thyroid and hormone support
– NAC/glutathione: cellular protection and detox support
– B vitamins: energy, hormone metabolism, cognitive health
Always consult your provider, especially if you’re on medications or have multiple diagnoses.
It’s common, but not inevitable. Many women feel worse during perimenopause due to hormone shifts, stress, and underrecognized autoimmune activity. But with the right support—including hormone testing, personalized nutrition, stress reduction, and possibly HRT or supplements—you can feel better and regain control over your symptoms.
Final Thoughts on Managing Menopause in Women with Autoimmune Disease
- So, is menopause and autoimmune disease a double whammy? It can be, but it’s also a chance to step into deeper body awareness and start advocating for more integrated care.
- Your hormones and immune system are deeply interconnected, and when they shift, your health story shifts, too.
- With the right testing, anti-inflammatory diet, nervous system support, and possibly HRT or targeted supplements, you can absolutely reduce flare-ups and feel better.
- No, you’re not imagining your symptoms. And no, you don’t just have to “just deal with it.”
Want more help with endometriosis flares? Download the free Endo Flare Toolkit for immediate relief strategies, stress-reduction tools, and an inflammation-reducing plan you can start today.
References
- https://womensmidlifehealthjournal.biomedcentral.com/articles/10.1186/s40695-015-0012-9 ↩︎
- https://www.scientificamerican.com/article/why-nearly-80-percent-of-autoimmune-sufferers-are-female/ ↩︎
- https://pmc.ncbi.nlm.nih.gov/articles/PMC11928423/ ↩︎
- https://www.health.harvard.edu/womens-health/beyond-hot-flashes ↩︎
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6501433/ ↩︎
- https://pmc.ncbi.nlm.nih.gov/articles/PMC11928423/ ↩︎
- https://www.health.harvard.edu/womens-health/beyond-hot-flashes ↩︎
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4365931/ ↩︎
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9379122/ ↩︎
- https://jneuroinflammation.biomedcentral.com/articles/10.1186/s12974-020-01998-9 ↩︎
- https://pubmed.ncbi.nlm.nih.gov/36641259/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/34908863/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/35719707/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/34989184/ ↩︎
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6372850/ ↩︎
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8211525/ ↩︎
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9709133/ ↩︎

