About 60–70% of perimenopausal women1 experience symptoms such as headaches, hot flashes, mood swings, depression, decreased libido, and sleep disturbances. Headaches during perimenopause and menopause are very common, yet rarely talked about. Many women ask, “Can menopause cause headaches?”— and the short answer is yes.
Shifting hormones, especially lower levels of estrogen and progesterone, can create the perfect environment for daily tension headaches and true menopause migraine headaches. Women who have a history of experiencing hormonal headaches in the past are even more at risk, since they can experience the perfect storm of causes that lead to migraines.
While these types of headaches can be frustrating, they are usually manageable with the right approach. Below, I'll help you understand what causes headaches from menopause, natural remedies and treatment options (including medication), and when it’s time to talk to your doctor.
In this article:
- Can Menopause Cause Headaches?
- Why Does Menopause Cause Headaches?
- How Common Are Menopause Headaches?
- Risk Factors for Menopause Headaches
- Natural Remedies for Menopause Headaches
- Diet Support for Headache Relief
- Other Treatment Options for Headaches
- When to See a Doctor
- Frequently Asked Questions About Menopause Headaches
- Final Thoughts: Why Are Headaches a Symptom of Menopause, And How Can They Be Treated?
Can Menopause Cause Headaches?
Yes. Menopause can cause headaches due to fluctuating and declining estrogen and progesterone levels, which affect blood vessel tone, serotonin signaling, inflammation, and nervous system sensitivity.
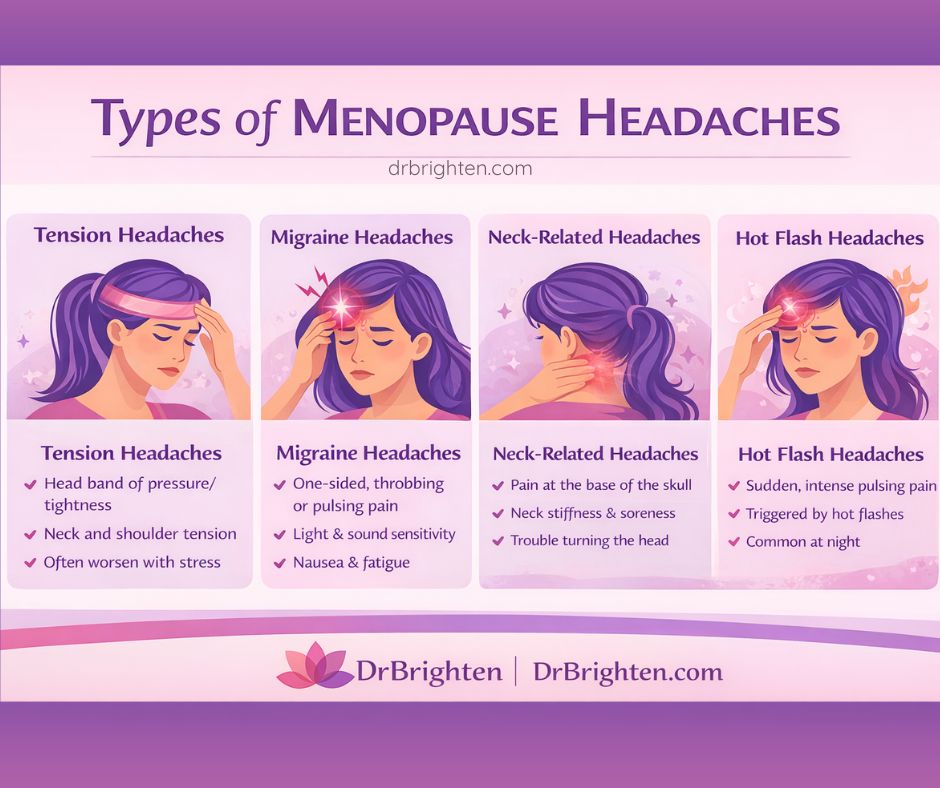
These headaches may present as tension headaches, migraines, neck-related headaches, or headaches associated with hot flashes and sleep disruption.
Why Does Menopause Cause Headaches?
Hormonal changes are the biggest reason for headaches in menopause.
Throughout your reproductive years, estrogen and progesterone rise and fall in a predictable monthly rhythm. As you enter perimenopause, these hormones become irregular. Progesterone typically declines first, followed by fluctuating and eventually decreased estrogen.
This instability can trigger what many women describe as hormonal headaches in menopause, headaches post menopause, and even headaches associated with hot flashes.
Some women also experience a “climax headache,” where intense vasodilation during a hot flash leads to a sudden throbbing sensation. Sometimes, intense headaches are also accompanied by symptoms like sound sensitivity, light sensitivity, or nausea and vomiting.
Estrogen is at the root of many hormonal headaches—including in women who are still menstruating (such as women who get menstrual migraines), those in perimenopause, and those who are menopausal.
Estrogen affects how your brain, blood vessels, and nervous system function. When levels drop too low or swing too quickly, it can affect neurotransmitters like serotonin and worsen inflammation, both of which are major drivers of headaches.
Related:
Menopause Fatigue Solved: Proven Ways to Reclaim Energy, Focus, and Vitality
How Common Are Menopause Headaches?
They're quite common. Research shows that women who are prone to menstrual migraines and headaches often see an increase in symptoms during perimenopause2, particularly when periods become irregular.
For example, one study3 found that about 30% of women experience their most frequent migraines during perimenopause, due to fluctuating hormones. Migraines are also known to affect women three times more often than men.
For women in perimenopause or menopause, headaches can occur:
- Right before or after a period (a classic perimenopause headache)
- With major hormone drops
- With hot flashes or night sweats
- During periods of sleep disruption
- Daily, due to chronic stress or muscular tension
Some women experience menopause headaches almost every day during the peak of their transition. Others only have them occasionally, maybe when they're very stressed or tired.
Related: Perimenopause Brain Fog: Causes, Symptoms, and Treatment Options
What Causes Menopause Headaches?
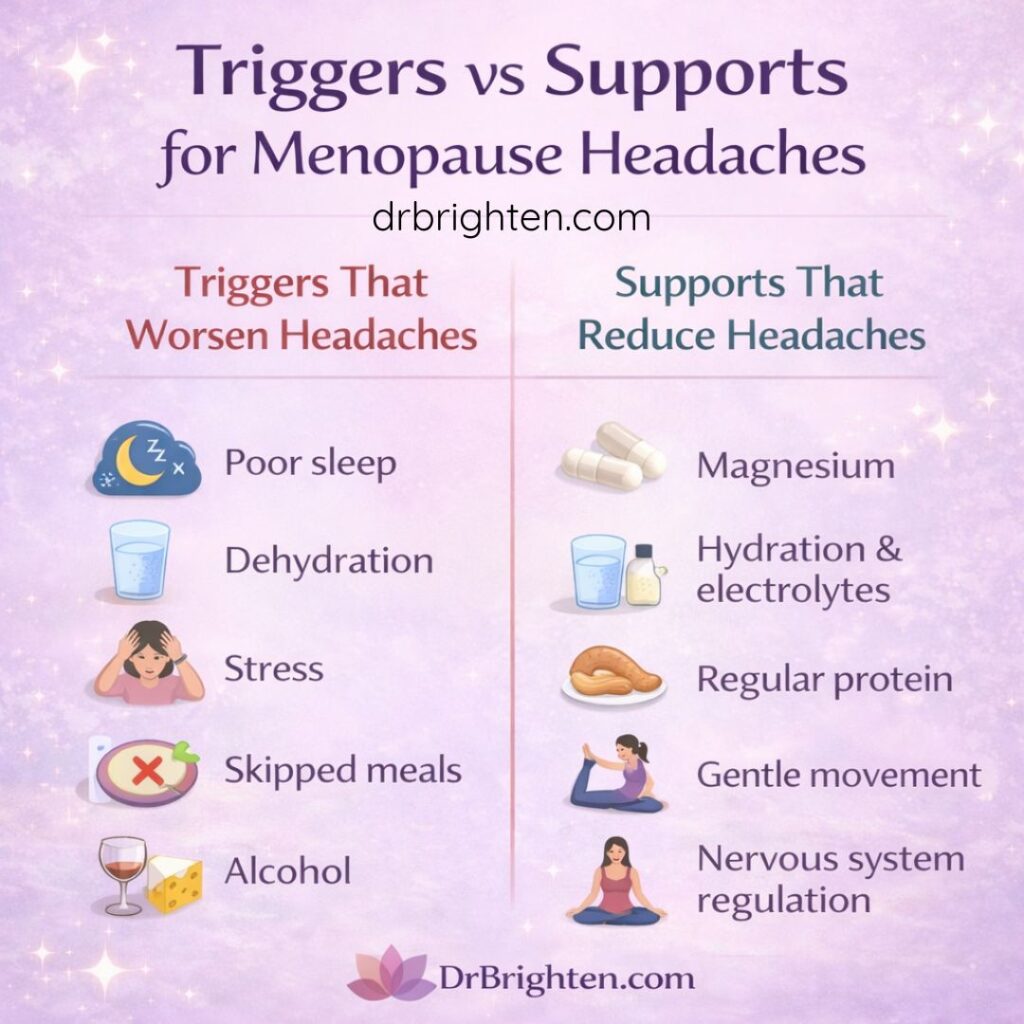
Like headaches during other stages of life, those that happen during menopause can be triggered by several things, such as hormones, stress, sleep, and your diet.
Even if you never had headaches before, shifting or declining hormones during perimenopause/menopause can make you more sensitive to triggers you previously tolerated.
Here are the biggest causes of most menopause headaches or migraines:
1. Hormone Fluctuations
Rapid changes in estrogen are the most well-known driver. For example, estrogen impacts vasodilation and blood flow. Drops in estrogen can cause blood vessels to spasm or dilate too quickly, triggering “throbbing” vascular migraines.
Low progesterone can also contribute to headaches, as progesterone is naturally calming and helps balance estrogen’s effects. When these hormones drop, poor sleep, stress, fatigue, and anxiety can increase, all of which can contribute to headaches.
2. Estrogen Dominance
Many women experience a phase of estrogen dominance as progesterone falls more quickly than estrogen. This imbalance can potentially lead to headaches, as well as breast tenderness, mood swings, and increased fluid retention.
3. Stress and Cortisol Dysregulation
Chronic stress alters your adrenal function, contributes to neck and shoulder tension, and makes you more vulnerable to inflammation-driven headaches.
4. Serotonin Drop
Estrogen directly influences serotonin production and how your brain uses it. When estrogen drops, serotonin drops too—this is a key reason for:
- Lower pain tolerance
- Increased sensitivity to light and sound
- Worsening migraines
This helps explain why headaches in menopause feel different from younger hormonal headaches.
5. Sleep Disruption
Night sweats, insomnia, and early waking can create a pattern of headaches and decreased pain tolerance. Not to mention, when you're sleep deprived, you tend to be in a worse mood and deal with more intense negative feelings, including pain.
6. Nutrient Deficiencies and Dehydration
Low magnesium, B vitamins, and omega-3 fats4 can increase the frequency and intensity of menopause headaches, along with other symptoms like low mood and fatigue.
Many women still have irregular bleeding during perimenopause, sometimes heavier than usual. This can lead to: iron deficiency and possibly anemia and oxygenation issues, which sometimes directly increase headache frequency.
Hot flashes and night sweats can also contribute to fluid and electrolyte losses—and then low sodium or potassium can trigger or worsen headaches.
7. Environmental, Diet, and Lifestyle Triggers
Alcohol, aged cheeses, skipped meals, dehydration, artificial fragrances, and even bright light can trigger headaches or migraines during menopause.
Histamine intolerance is another potential issue. Estrogen and histamine feed one another. During perimenopause, estrogen surges raise histamine, which can potentially trigger headaches.
8. Neck and Muscle Tension
Some women specifically report menopause headaches with neck pain because of chronic tension, posture habits, or sleep disturbances.
Risk Factors for Menopause Headaches
You’re more likely to develop headaches during menopause5 if you have:
- A history of menstrual migraines
- Having had PMDD, which can cause headaches and other types of pain
- Family history of migraines
- High stress or poor sleep
- Estrogen dominance symptoms
- Thyroid dysfunction
- Blood sugar instability
- High caffeine or alcohol intake
- Exposure to endocrine-disrupting chemicals
- Nutrient deficiencies (especially magnesium)
Related:
Hangover Remedies: What Happens to Your Body When You’re Hungover + How to Recover

Natural Remedies for Menopause Headaches
Many women prefer to start with natural remedies for menopause headaches, especially when symptoms are mild to moderate. These strategies support hormonal balance, reduce inflammation, and address root causes.
1. Magnesium
Magnesium is one of the most researched nutrients and helpful remedies for hormonal headaches, considering it supports blood vessel relaxation, reduces inflammation, balances neurotransmitters, and helps calm the nervous system.
Some evidence suggests that women who experience menopause migraine headaches are often deficient in magnesium, which can make their symptoms more intense.
The American Migraine Foundation6 recommends taking magnesium supplements from day 15 of the menstrual cycle (if you still get your period) through the next period as a helpful prevention strategy for headaches.
For women experiencing menopause headaches, especially daily tension headaches or migraine-type headaches, Magnesium Plus is often used as a foundational nutrient to support vascular stability, nervous system regulation, and sleep quality.
Magnesium Plus can be taken daily for headache prevention, and some women find additional benefits when taken in the evening to support sleep. Dosage should be individualized, but magnesium is commonly used in the range studied for migraine prevention.
Why Magnesium Plus Is My Preferred Magnesium for Menopause Headaches
- Uses magnesium glycinate, a form shown to support relaxation of blood vessels and the nervous system without causing diarrhea
- Well tolerated in women with gut sensitivity, which is common during perimenopause
- Supports sleep quality, stress resilience, and muscle relaxation — all key drivers of menopause headaches
- Appropriate for daily preventive use, not just acute headache relief
Types of Magnesium
| Magnesium Form | Absorption | Gut Tolerance | Headache Support |
| Oxide | Low | Poor | Poor quality |
| Citrate | Moderate | Can cause diarrhea | Lower quality |
| Glycinate | High | Gentle | Preferred |
Related:
Magnesium for Menopause Symptoms: Your Comprehensive Guide
Magnesium for Sleep: Complete Guide to Best Forms and Dosage
2. Vitamin B2 (Riboflavin)
Vitamin B2 has been shown to reduce migraine frequency7 when taken consistently, usually in amounts of about 400 milligrams/day. It supports mitochondrial energy production in brain cells, which is especially important when fluctuating estrogen increases neurological sensitivity.
B2 can be particularly helpful for menopause migraine headaches because it improves energy metabolism in the brain, where hormonal shifts can disrupt normal cellular activity.
3. Feverfew
Feverfew has been used traditionally to reduce migraine intensity and support vascular health. It can potentially help reduce the frequency of hormonal headaches by calming blood vessel dilation, a major trigger during estrogen drops.
Some studies8 suggest feverfew may work best for headaches when used consistently for weeks to months. This means it's mostly a good option for ongoing perimenopause headaches rather than sudden flares. That said, it doesn't seem to work well for every person, although it's worth trying since it has little risk of causing side effects.
3. Turmeric/Curcumin
Turmeric is excellent for inflammation-driven headaches and supports overall hormone balance, including by influencing inflammatory pathways (like NF-κB). It's a beneficial herb to take during perimenopause for many reasons, including because this is when systemic inflammation often increases.
Regularly taking turmeric can help reduce the severity of headache triggers9 (including inflammatory responses) related to poor sleep, hot flashes, and stress, which are three of the most common drivers of menopause symptoms, including headaches.
4. Hydration
Even mild dehydration increases headache risk in menopause. And in dry indoor environments or after alcohol consumption, the effects can be even worse. Because estrogen affects fluid balance, many women become more prone to dehydration during perimenopause without realizing it.
Staying hydrated is also important for supporting blood volume and circulation, both of which help prevent the vascular changes that contribute to menopause migraine headaches.
5. Ginger
Ginger has anti-inflammatory effects and is well known for easing nausea, which is sometimes associated with strong headaches or migraine. It also helps calm an overactive nervous system, which is helpful when headaches accompany hot flashes or stress.
Some research suggests ginger (usually taken in supplement form) can be nearly as effective as certain migraine medications10 for short-term symptom relief, making it a valuable natural remedy for menopause headaches.
6. EPA (Omega-3 Fats)
Omega-3 fatty acids (such as Omega Plus) can help reduce inflammation and support healthy hormone signaling, which can stabilize the blood pressure changes that sometimes lead to pulsating headaches. They also support brain health during a time when declining estrogen affects cognitive and neurological function.
EPA-rich fish oil can even improve your mood and the quality of your sleep (two factors that can influence how often headaches in menopause occur).
7. Movement & Exercise
Low-intensity movement increases circulation, supports lymph flow, and helps manage blood sugar levels, meaning it has multiple benefits for reducing triggers of hormonal headaches in menopause.
Gentle exercise, like walking outside or doing yoga, can also relieve neck and shoulder tension, which contributes to menopause headaches with neck pain.
Activities like walking, Pilates, or light strength training may reduce the intensity of headaches over time by lowering inflammation and supporting hormone regulation.
8. Stress Reduction and Nervous System Support
Stress is one of the strongest triggers for headaches post menopause because cortisol imbalances increase inflammation and muscle tension.
Mind-body practices and parasympathetic-activating strategies can help calm down an overactive nervous system, which becomes more reactive when estrogen fluctuates. To defend against tension headaches and stress-related migraines, try:
- Progressive muscle relaxation
- Paced breathing
- Vagus nerve–supportive practices
- Meditation
9. Sleep Optimization
Since insomnia and night sweats can amplify headaches, do whatever you can to get the best sleep possible. Consider trying:
- Magnesium
- Glycine
- L-theanine
- Turning off devices 2 hours before bedtime
- Adaptogens and herbs like ashwagandha, lemon balm, and passionflower
- Getting more exercise and sunlight during the day
- Making sure your room is cool and very dark
Related: Why Can’t I Sleep? The Real Reasons for Perimenopause Sleep Issues (and What Actually Helps)
10. Essential Oils
Lavender or peppermint oil can be applied to the temples to ease tension and pain. Lavender can help lower stress and improve sleep quality in perimenopause, which indirectly reduces headache frequency.
Peppermint can help relax tight muscles along the scalp and neck, which is helpful when headaches worsen with neck pain or poor posture habits.
11. Cold Compress
A cold compress provides fast relief by calming inflammation and soothing throbbing blood vessels. Try this when you experience headaches that are combined with hot flashes, or when vasodilation triggers a sudden “climax headache.”
Using a cold pack at the base of the skull can also help reduce neck-related tension that contributes to perimenopause headaches.
12. Chiropractic Treatments, Acupuncture, or Massage
Some people find that chiropractic adjustments or therapeutic massage are helpful when headaches are linked to neck tension, muscle imbalance, or posture.
Many women unknowingly develop chronic tightness in the upper back and jaw during menopause due to stress and sleep disruptions. Improving alignment and releasing muscle tension can often help reduce daily menopause headaches and prevent them from escalating into migraines.
Additionally, multiple studies show that acupuncture can help reduce the frequency of migraines or the severity of menopause symptoms. Seek out help from an integrative practitioner who's knowledgeable about menopause care.
13. DIM
DIM (diindolylmethane) is a compound that assists with estrogen metabolism11, which is essential if estrogen imbalance or dominance is contributing to menopause symptoms like hormonal headaches.
DIM, which is found in Balance Women's Hormone Support, also assists the body in producing more favorable estrogen metabolites and can inhibit the conversion of testosterone to estrogen, which is helpful for balancing these two hormones.
14. Liver Supporting Foods
Pairing DIM with liver-supportive foods (like cruciferous vegetables, leafy greens, and beets) as well as polyphenol foods (like olive oil, dark chocolate, green tea, and berries) amplifies its benefits by helping with detoxification and assisting the body in clearing hormones.
In general, a healthy diet—especially one with plenty of polyphenols—can also often help decrease headache intensity and PMS-like symptoms during perimenopause by improving gut health12, lowering inflammation, and improving blood sugar balance.
15. Caffeine (in Moderation)
Caffeine is a popular method for managing headaches because it can constrict blood vessels and relieve pain. That said, too much can have the opposite effect by triggering withdrawal headaches or worsening your sleep.
When used in moderate amounts, like a small cup of coffee during the early stages of a headache, it can usually be helpful. Women who experience headaches and menopause symptoms related to sleep loss might find caffeine to be really helpful, but it should be avoided after noon so it doesn't mess with your sleep.
Diet Support for Headache Relief
Certain foods (and drinks) can both trigger and soothe headaches from menopause.
Common Triggers to Avoid or Limit:
- Red wine
- Gluten (for some women)
- Preservatives found in ultra-processed foods
- MSG
- Artificial sweeteners
- Aged cheeses
One study found that more than 60% of headaches13 were thought to be triggered by certain foods. As many as 27% of migraines may be triggered by foods, and 38% by alcohol.
Supportive Foods:
- Fatty fish (rich in magnesium and omega-3s)
- Nuts and seeds
- Avocado
- Leafy greens
- Brightly colored vegetables, like peppers, broccoli, and others
- Turmeric and ginger
- High-fiber foods to support estrogen metabolism, such as beans, veggies, berries, and whole grains
Eating protein regularly and avoiding long stretches without food can also prevent blood sugar drops that worsen headaches.
Related: Histamine Intolerance: What It Is & What to Do About It
Other Treatment Options for Headaches
If natural remedies aren’t enough, or if your headaches are severe, additional medical options can potentially help, according to the Association of Migraine Disorders14:
- NSAIDs (used wisely and not daily)
- Triptans for true migraines
- Hormone therapy (HRT), when appropriate, since some women find that stabilizing estrogen levels reduces headache frequency. Transdermal estradiol is usually less likely to trigger migraines than oral formulations
- Birth control pills (to help with hormone fluctuations)
- Muscle relaxants for tension-driven headaches
- Preventive medications when headaches become chronic and don't respond well to other treatments (like gepants and neuromodulation devices)
Your provider will help you determine what’s appropriate based on your symptoms and overall health profile.
When to See a Doctor
Not all headaches in menopause are hormonal. Seek medical care if you experience:
- A sudden, severe headache (like a “thunderclap” type of headache that's very intense and out of nowhere)
- New headaches after age 50
- Headaches that worsen steadily over time
- Headaches with other neurological symptoms (like vision changes, slurred speech, or weakness)
- Headaches with fever or neck stiffness
- Headaches after a fall or head injury
- Headaches that interfere significantly with daily life or sleep
A hormone-literate practitioner can help determine whether your symptoms are due to estrogen fluctuations, nutrient deficiencies, thyroid issues, blood pressure changes, or something else entirely.
For example, hypothyroidism is more common in perimenopause and menopause, and headaches are a common symptom, which means testing thyroid hormones can be a helpful place to start.
Frequently Asked Questions About Menopause Headaches
Yes. Headaches are a common symptom of perimenopause and menopause, largely due to fluctuating and declining estrogen and progesterone levels. These hormonal shifts affect blood vessel tone, serotonin signaling, inflammation, and nervous system sensitivity, all of which can contribute to headaches and migraines.
Yes. Some women experience daily menopause headaches, especially during perimenopause when hormone fluctuations are most pronounced. Daily headaches are often linked to unstable estrogen levels, poor sleep, chronic stress, magnesium deficiency, neck and muscle tension, or blood sugar instability.
Menopause headaches can vary widely and may feel different from headaches earlier in life. Common presentations include:
– Tension-type headaches with neck or shoulder pain
– Throbbing or pulsating migraine-type headaches
– Headaches associated with hot flashes or night sweats
– Headaches with light or sound sensitivity
– Headaches accompanied by nausea or fatigue
Some women also experience sudden, intense headaches during hot flashes due to rapid vasodilation.
The most common causes of perimenopause headaches include:
– Rapid estrogen fluctuations
– Declining progesterone levels
– Serotonin changes
– Sleep disruption from night sweats or insomnia
– Chronic stress and cortisol dysregulation
– Magnesium and B-vitamin deficiencies
– Dehydration and electrolyte imbalance
Even women who never had headaches before may develop them during this transition.
Yes. Headaches post menopause can still occur, especially if estrogen levels remain low and unsupported. Low estrogen can reduce serotonin availability, increase inflammation, and impair blood vessel regulation, all of which may contribute to ongoing headaches or migraines after menopause.
Magnesium glycinate is often considered the best form of magnesium for menopause headaches because it is highly absorbable and gentle on digestion. It supports nervous system regulation, muscle relaxation, vascular stability, and sleep quality—all key factors in hormonal headache prevention.
Magnesium Plus uses magnesium glycinate and is commonly used in clinical practice for women experiencing menopause headaches, migraines, sleep disturbances, and stress-related tension.
Magnesium helps menopause headaches by:
– Relaxing blood vessels and reducing vascular spasm
– Supporting serotonin and neurotransmitter balance
– Calming the nervous system
– Reducing muscle tension in the neck and shoulders
– Improving sleep quality
Low magnesium levels are common in women with migraines and hormonal headaches, making magnesium a foundational nutrient for prevention and support.
Magnesium can be taken daily for prevention or as part of an evening routine to support sleep, which often reduces headache frequency. Some women find benefit from consistent daily use, while others use magnesium during periods of increased stress, poor sleep, or hormonal instability. Dosage should be individualized based on tolerance and clinical guidance.
Yes. Menopause headaches with neck pain are very common. Hormonal changes can increase muscle tension, alter posture, disrupt sleep, and heighten pain sensitivity. Addressing magnesium status, stress, posture, and gentle movement can significantly reduce this type of headache.
They can be. Rapid changes in blood vessel dilation during hot flashes may trigger headaches, sometimes referred to as “climax headaches.” These headaches are often sudden, throbbing, and may respond well to cooling strategies, hydration, and magnesium support.
Common natural remedies include:
– Magnesium (especially magnesium glycinate)
– Riboflavin (vitamin B2)
– Omega-3 fatty acids
– Ginger or turmeric
– Adequate hydration and electrolytes
– Stress-reduction practices
– Sleep optimization
Many women benefit most from combining nutritional support with lifestyle and nervous system regulation strategies.
You should seek medical care if you experience:
– Sudden, severe “thunderclap” headaches
– New headaches after age 50
– Headaches with neurological symptoms (vision changes, weakness, slurred speech)
– Headaches that worsen progressively
– Headaches that significantly interfere with daily life or sleep
A hormone-literate practitioner can help determine whether headaches are related to hormonal changes, nutrient deficiencies, thyroid function, blood pressure, or other underlying conditions.
Final Thoughts: Why Are Headaches a Symptom of Menopause, And How Can They Be Treated?
- Menopause headaches can feel overwhelming, especially if they appear daily or arrive with hot flashes, neck pain, or sleep disturbances.
- But you’re not powerless. Supporting hormone balance, reducing inflammation, and addressing nutrient needs, especially magnesium (such as with help from Magnesium Plus), can make a meaningful difference.
- If you’re struggling with persistent menopause headaches, know this: you deserve relief, you deserve answers, and you don’t have to navigate this transition alone.
- Working with a knowledgeable practitioner can help you identify the root cause and find the right treatment plan so you can feel like yourself again.
References
- https://pmc.ncbi.nlm.nih.gov/articles/PMC12089631/ ↩︎
- https://menopause.org/patient-education/menopause-topics/perimenopause ↩︎
- https://pmc.ncbi.nlm.nih.gov/articles/PMC12089631/ ↩︎
- https://pmc.ncbi.nlm.nih.gov/articles/PMC12209554/ ↩︎
- https://migrainetrust.org/news/migraine-and-perimenopause/ ↩︎
- https://americanmigrainefoundation.org/resource-library/hormonal-menstrual-migraine/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/33779525/ ↩︎
- https://www.migraineagain.com/feverfew-migraine-prevention/ ↩︎
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8724631/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/33293189/ ↩︎
- https://link.springer.com/article/10.1186/s12906-024-04708-7 ↩︎
- https://pubmed.ncbi.nlm.nih.gov/41305622/ ↩︎
- https://pmc.ncbi.nlm.nih.gov/articles/PMC7496357/ ↩︎
- https://www.migrainedisorders.org/perimenopause-and-menopause/ ↩︎


