Endometrial hyperplasia can be the cause of heavy periods, large clots in the menstrual blood, and in some cases, cancer. Often excess estrogen in the absence of sufficient progesterone, known as estrogen dominance, causes the cells in the lining of the uterus (the endometrium) to grow abnormally thick. When the endometrium becomes too thick, you end up with a condition known as endometrial hyperplasia.
In this article, I’m going through everything you need to know about endometrial hyperplasia: the causes, types, treatments, risk factors, and possible complications.
In this article:
- What Is Endometrial Hyperplasia?
- Endometrial Hyperplasia Symptoms
- What Causes Endometrial Hyperplasia?
- How Common Is Endometrial Hyperplasia?
- How Is Endometrial Hyperplasia Diagnosed?
- Types Of Endometrial Hyperplasia
- What Are The Risk Factors For Endometrial Hyperplasia?
- What Is The Treatment For Endometrial Hyperplasia?
- Should I Have A Hysterectomy For Endometrial Hyperplasia?
- What Is The Difference Between Endometrial Hyperplasia and Endometriosis?
- Can Hyperplasia Become Cancerous?
- Endometrial Hyperplasia — Don’t Go It Alone
- Citations
What Is Endometrial Hyperplasia?
Endometrial Hyperplasia is a condition in which the lining of the uterus thickens because estrogen stimulates the tissue to grow. It can progress to cancer or coincide with endometrial cancer.
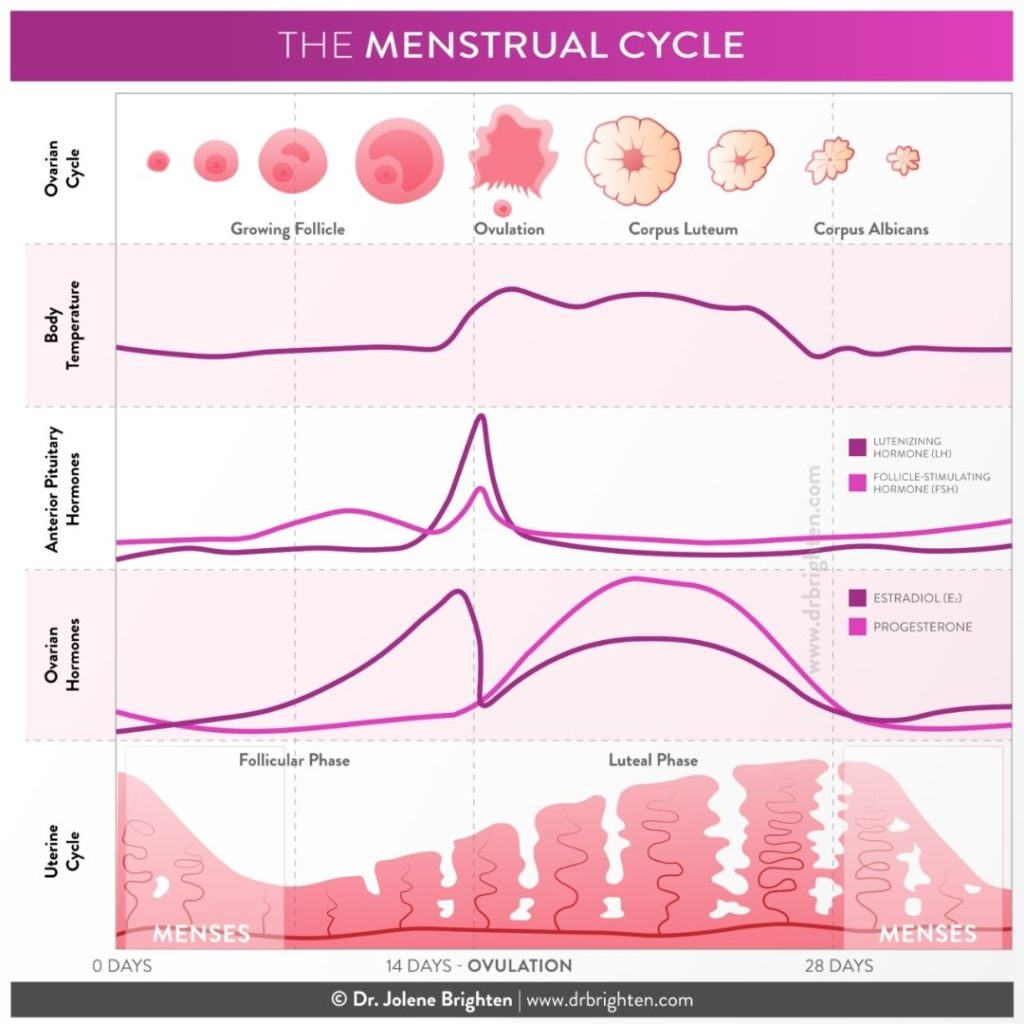
Typically, estrogen levels are challenged by progesterone during the luteal phase, which prevents estrogen from going overboard with driving tissue growth. Typically, this condition comes with heavy menstrual bleeding. But, heavy periods alone aren’t enough to diagnose endometrial hyperplasia since heavy bleeding can be caused by other common disorders of the reproductive system — like uterine fibroids or endometriosis. Diagnosing endometrial hyperplasia requires medical investigation.
Endometrial Hyperplasia Symptoms
There are several symptoms that you may experience if you have overgrowth of the uterine lining. Keep in mind, these can be common signs and symptoms for several other reproductive conditions, so be sure to be very specific with your doctor about your symptoms to help them arrive at a correct diagnosis quickly.
Some of the Symptoms of Endometrial Hyperplasia May Include:
- Heavy menstrual bleeding
- Bleeding or spotting between periods
- Bleeding or spotting after menopause
- Loss of period (amenorrhea) before menopause
- Short menstrual cycles (under 21 days)
Does Endometrial Hyperplasia Cause Weight Gain?
While this condition does not cause weight gain per se, excess estrogen (the underlying cause) has been known to add extra pounds for some women.
Women who are obese are at a higher risk of developing endometrial hyperplasia and uterine cancer. This isn’t to body shame, but rather, to make you aware of potential risk factors. Adipocytes (fat cells) can produce estrogen, so more fat cells can mean more estrogen to stimulate the uterine lining.
What Causes Endometrial Hyperplasia?
Endometrial hyperplasia is caused by a common culprit, estrogen. When there is frank estrogen dominance, overall excess estrogen, or relative estrogen dominance, insufficient progesterone to challenge estrogen, endometrial hyperplasia develops. Excess or unopposed estrogen stimulates the endometrial glands to enlarge or grow into an unusual shape, which thickens the lining of the uterus.
While it is commonly thought this condition affects only people during the perimenopause and menopause phase, it can occur during the fertile life phase of life as well.
Hormone Replacement Therapy
Hormone replacement therapy can result in endometrial hyperplasia if you’re taking too high of a dose of estrogen or not using sufficient progesterone. This is why working with an experienced practitioner and having your therapy monitored is so important.
Anovulatory Cycles
Conditions that are linked to anovulation (lack of ovulation) or oligomenorrhea (in frequent periods) like polycystic ovarian syndrome (PCOS) or undiagnosed thyroid issues can put women at greater risk. You need ovulation in order to make sufficient progesterone. If you miss the surge of progesterone that helps keep estrogen in check, it can lead to you can end up with abnormal thickening of the uterine lining.
Excess Estrogen
Women who are obese are considered at a higher risk for the condition because fat cells can produce estrogen and lead to elevated levels. There is also speculation that gut dysbiosis (imbalance of gut flora), liver conditions and other factors which contribute to excess estrogen contribute. To learn how to optimize estrogen naturally using nutrition and lifestyle with the free hormone starter kit.

How Common Is Endometrial Hyperplasia?
Studies suggest that this condition is most common in women who are aged 44-64. While not typical in younger women, it’s not unheard of for younger women to develop it. Due to declining levels of estrogen, women over 65 are unlikely to experience endometrial overgrowth.
How Is Endometrial Hyperplasia Diagnosed?
Your doctor will likely not be able to diagnose endometrial hyperplasia by simply evaluating your symptoms. There are different types of endometrial hyperplasia, which is determined by evaluating tissue samples. This is why your doctor will need to get a biopsy to make a diagnosis.
Endometrial Hyperplasia Ultrasound
When diagnosing the overgrowth of uterine lining, physicians will often first perform a transvaginal ultrasound. This involves using sound waves to create an image of your reproductive organs, and measuring the thickness of the uterine lining using the rendered image on the screen.
Endometrial Hyperplasia Biopsy
If the ultrasound shows an abnormally thick uterine lining, your doctor may then order a biopsy. This is when a sample of the tissue from the endometrium is removed so that it can be evaluated with a microscope. The tissue is retrieved via biopsy, hysteroscopy or dilation and curettage (D&C). Sometimes, the doctor may widen the cervix and retrieve a tissue sample that way. This procedure is known as dilation and curettage.
It’s a good idea to discuss the pros and cons of both options (anesthesia, discomfort, accuracy, etc.) with your doctor when you’re planning your testing. Be sure to make a list of questions before going to your appointment so you can have a thorough understanding of the procedure.
Types Of Endometrial Hyperplasia
There are different types of endometrial hyperplasia. They are divided into 3 basic categories:
- Simple hyperplasia
- Complex hyperplasia
- Simple Hyperplasia with Atypia
- Endometrial Hyperplasia with Atypia
Simple Hyperplasia
Simple, or basic endometrial hyperplasia is generally considered benign, or minimal risk. This is when the endometrial glands are considered oversized, but not necessarily crowded or atypical.
Complex Hyperplasia
Complex endometrial hyperplasia is characterized by a “crowding” or “budding” of the endometrial glands. This condition is generally not considered precancerous unless it is accompanied by atypia.
Simple Hyperplasia with Atypia
This is a rare form of hyperplasia.
Endometrial Hyperplasia With Atypia
Endometrial hyperplasia with atypia, also known as atypical endometrial hyperplasia, is largely considered a precancerous condition. It is the least common type of hyperplasia, but the most likely to develop into type 1 endometrial carcinoma. Your doctor may refer to this as endometrial intraepithelial neoplasia (EIN).
Your doctor may specify whether atypical endometrial hyperplasia is simple, meaning only the endometrial glands show abnormal growth, or complex, where the endometrium and blood vessels show abnormality.
What Are The Risk Factors For Endometrial Hyperplasia?
According to the American College of Gynecology and Obstetrics, endometrial hyperplasia is more likely to occur in women who:
- Have never been pregnant
- Have been through menopause
- Are over the age of 35
- Are obese
- Have diabetes
- Have PCOS
- Have thyroid disease
- Have gallbladder disease
- Are caucasian*
- Are or have been smokers
- Got their first period at an early age
- Have a family history of ovarian, colon, or uterine cancer
- Have or have had ovarian tumors
*It’s important to note that with regards to endometrial cancer, African American women tend to be diagnosed later, which may account for caucasian women being considered at higher risk for hyperplasia. Some cases of hyperplasia progress to cancer, which is why early detection is important.
An additional risk factor may include, using estrogen alone after menopause.
What Is The Treatment For Endometrial Hyperplasia?
The treatment for endometrial hyperplasia is dependent upon the type you may be diagnosed with. You provider should discuss with you natural, pharmaceutical and surgical options for your specific case.
Progesterone Therapy
Since excess estrogen is usually involved with this condition, the typical conventional treatment for simple hyperplasia is progestin, which is a synthetic form of progesterone, or bioidentical progesterone. This helps combat the overabundance of estrogen. Progestin can be administered in a variety of ways, including an intrauterine device (IUD), pills, shots, or topical creams.
Some women will see their endometrial hyperplasia subside in response to progestin. Studies show that patients who undergo these treatments have as much as a 90% chance of regression of their condition.
Supporting Estrogen Metabolism
Your liver, gut and kidneys work together to eliminate estrogen the body no longer needs. The liver helps ready estrogen for excretion through the urine and stool.
Whenever estrogen dominance is at play, we always have the ability to try to balance hormones naturally, as well. Excess estrogen can be reduced when we focus on supporting the liver in processing estrogen and helping the gut to eliminate it.
I have tons of resources in my article library devoted to helping you understand estrogen dominance. Clinically, I've found using supplementation in addition to diet and lifestyle to be a crucial step in brining estrogen into balance.
One reliable formula I use is Balance – Women's Hormone Support as part of a hormone balancing routine. It’s specifically designed to help maintain healthy estrogen levels. It contains DIM, B vitamins, and reseveratrol to support liver health and balanced estrogen metabolites. It also contains calcium d-glucarate, which is crucial for the gut phase of hormone detoxification.
Some of the basic things you can do to help decrease signs of estrogen dominance:
- Eat your vegetables and plenty of fiber. Grab my free meal plan and recipe guide to help you get started.
- Take a high-quality probiotic to help build up gut health
- Get plenty of rest, and make sure your room is pitch black at night
- Reduce exposure to endocrine-disrupting chemicals that are often found in cosmetics and cleaning product.
Pharmaceutical Therapies
Beyond using progesterone therapy, your doctor may also recommend a prescription to stimulate ovulation, optimize blood sugar or modulate estrogen production.
Other, less common treatments for endometrial hyperplasia include:
- Inducing ovulation with clomiphene — this helps your body produce progesterone
- Metformin (a diabetes drug) — this helps by reducing insulin resistance which can be at the heart of estrogen dominance
- Danazol therapy — this androgen helps mitigate estrogen production
Should I Have A Hysterectomy For Endometrial Hyperplasia?
Your doctor should review your lab findings and personal history to help you understand if a hysterectomy is the best course of treatment for you. If you have complex hyperplasia, especially with atypia, your doctor may recommend a hysterectomy.
A hysterectomy is a surgery to remove the uterus. Sometimes, other reproductive organs are removed along with the uterus, including the ovaries, cervix, or fallopian tubes. Since there is a risk of developing endometrial cancer for women with endometrial hyperplasia, sometimes removing the uterus and cervix is the safest option. Approximately 25% of premenopausal women with uterine cancer also have cancer cells in their ovaries, so removing them as well may be deemed the safest option.
A hysterectomy is generally reserved for post-menopausal women, women at high risk of endometrial cancer, or who do not wish to have children.
Even though endometrial hyperplasia is most common in postmenopausal women, it’s still possible for women who are of childbearing age to develop it. Those who still desire to have children may not want to resort to hysterectomy surgery before exploring other treatment options first.
What Is The Difference Between Endometrial Hyperplasia and Endometriosis?
While these two conditions have very similar sounding names, they are in fact different.
Endometrial hyperplasia is a “thickening” of the uterine lining. It happens when endometrial cells grow quickly or in excess. With endometriosis, the tissue is similar but not the same as the endometrial lining and can be found outside the uterus. Endometrial hyperplasia stays within the uterus.
Can Hyperplasia Become Cancerous?
There is definitely a correlation between endometrial hyperplasia and cancer.
Endometrial hyperplasia with atypia can progress to cancer up to 27% of the time. Some doctors warn that these numbers may be underestimated, since 36% to 59% of women undergoing hysterectomy for atypical endometrial hyperplasia also have cancer at the same time.
Without atypia, cancer rates for endometrial hyperplasia are lower. Estimates are in the 1-8% range.
Endometrial Hyperplasia — Don’t Go It Alone
The majority of women with endometrial hyperplasia are able to manage their condition and often achieve regression, even with non-invasive therapies.
However, it’s understandable to be a little scared if you’ve received this diagnosis. After all, anything that’s even remotely associated with cancer can be scary!
Please, remember that you are not alone and you have options.
I also have a huge resource for you. If you’re just getting started in this world of hormones and you’re feeling just a bit lost, I’ve compiled a massive hormone balancing starter kit (that’s completely free), which will help you troubleshoot low progesterone, excess estrogen, and even comes with a meal plan. I’ve got recipes in there that will show you how to start eating for hormonal balance and can really help you start to get everything back on track. You can do this!
Citations
Wise MR, Jordan V, Lagas A, et al. Obesity and endometrial hyperplasia and cancer in premenopausal women: A systematic review. American Journal of Obstetrics and Gynecology. 2016;214(6). doi:10.1016/j.ajog.2016.01.175 https://www.sciencedirect.com/science/article/abs/pii/S0002937816002258
“Endometrial Hyperplasia – an overview | ScienceDirect Topics.”
https://www.sciencedirect.com/topics/medicine-and-dentistry/endometrial-hyperplasia
Urban R, Reed S. Management of endometrial hyperplasia. In: UpToDate, Post, TW (Ed), UpToDate, Waltham, MA, 2020.
https://www.uptodate.com/contents/management-of-endometrial-hyperplasia
Lethaby A, Suckling J, Barlow D, Farquhar CM, Jepson RG, Roberts H. Hormone replacement therapy in postmenopausal women: endometrial hyperplasia and irregular bleeding. Cochrane Database Syst Rev. 2004;(3):CD000402. doi:10.1002/14651858.CD000402.pub2
https://pubmed.ncbi.nlm.nih.gov/15266429/
Archer DF. Continuous combined hormone replacement therapy and endometrial hyperplasia. BMJ. 2002;325(7358):231–232. doi:10.1136/bmj.325.7358.231
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1123759/
Feeley KM, Wells MHormone replacement therapy and the endometriumJournal of Clinical Pathology 2001;54:435-440.
https://jcp.bmj.com/content/54/6/435
Eden JA, Hacker NF, Fortune M. Three cases of endometrial cancer associated with “bioidentical” hormone replacement therapy. Med J Aust 2007; 187 (4): 244-245. || doi: 10.5694/j.1326-5377.2007.tb01210.x Published online: 20 August 2007
Reed SD, Newton KM, Clinton WL, et al. Incidence of endometrial hyperplasia. Am J Obstet Gynecol. 2009;200(6):678.e1–678.e6786. doi:10.1016/j.ajog.2009.02.032
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2692753/
Yuk JS. The incidence rates of endometrial hyperplasia and endometrial cancer: a four-year population-based study. PeerJ. 2016;4:e2374. Published 2016 Aug 24. doi:10.7717/peerj.2374
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5012286/
Raychaudhuri G, Bandyopadhyay A, Sarkar D, Mandal S, Mondal S, Mitra PK. Endometrial hyperplasia: a clinicopathological study in a tertiary care hospital. J Obstet Gynaecol India. 2013;63(6):394–398. doi:10.1007/s13224-013-0414-2
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3889273/
Suh-Burgmann, Elizabeth MD1; Hung, Yun-Yi PhD2; Armstrong, Mary Anne MA2 Complex Atypical Endometrial Hyperplasia, Obstetrics & Gynecology: September 2009 – Volume 114 – Issue 3 – p 523-529 doi: 10.1097/AOG.0b013e3181b190d5
Byun JM, Jeong DH, Kim YN, et al. Endometrial cancer arising from atypical complex hyperplasia: The significance in an endometrial biopsy and a diagnostic challenge. Obstet Gynecol Sci. 2015;58(6):468–474. doi:10.5468/ogs.2015.58.6.468
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4663224/
Reed SD, Newton KM, Garcia RL, et al. Complex hyperplasia with and without atypia: clinical outcomes and implications of progestin therapy. Obstet Gynecol. 2010;116(2 Pt 1):365–373. doi:10.1097/AOG.0b013e3181e93330
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2949551/
Penelope M Webb, Commentary: Weight gain, weight loss, and endometrial cancer, International Journal of Epidemiology, Volume 35, Issue 1, February 2006, Pages 166–168, https://doi.org/10.1093/ije/dyi301
https://academic.oup.com/ije/article/35/1/166/849995
Chandra V, Kim JJ, Benbrook DM, Dwivedi A, Rai R. Therapeutic options for management of endometrial hyperplasia. J Gynecol Oncol. 2016;27(1):e8. doi:10.3802/jgo.2016.27.e8
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4695458/
Kistner RW, Lewis JL, Steiner GJ. Effects of clomiphene citrate on endometrial hyperplasia in the premenopausal female. Cancer. 1966;19(1):115–126. doi:10.1002/1097-0142(196601)19:1<115::aid-cncr2820190113>3.0.co;2-f
https://pubmed.ncbi.nlm.nih.gov/5948088/?from_single_result=5948088&expanded_search_query=5948088
Tas M, Kutuk MS, Serin IS, Ozgun MT, Oner G, Ozturk F. Comparison of antiproliferative effects of metformine and progesterone on estrogen-induced endometrial hyperplasia in rats. Gynecol Endocrinol. 2013;29(4):311–314. doi:10.3109/09513590.2012.743010
https://pubmed.ncbi.nlm.nih.gov/23305503/?from_single_result=23305503&expanded_search_query=23305503
Meireles CG, Pereira SA, Valadares LP, et al. Effects of metformin on endometrial cancer: Systematic review and meta-analysis. Gynecol Oncol. 2017;147(1):167–180. doi:10.1016/j.ygyno.2017.07.120
https://pubmed.ncbi.nlm.nih.gov/28760367/?from_single_result=28760367&expanded_search_query=28760367
Mariani L, Sedati A, Giovinazzi R, Sindico R, Atlante G. Postmenopausal endometrial hyperplasia: role of danazol therapy. Int J Gynaecol Obstet. 1994;44(2):155–159. doi:10.1016/0020-7292(94)90071-x
https://pubmed.ncbi.nlm.nih.gov/7911101/?from_single_result=7911101&expanded_search_query=7911101
Kim JJ, Chapman-Davis E. Role of progesterone in endometrial cancer. Semin Reprod Med. 2010;28(1):81–90. doi:10.1055/s-0029-1242998
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4767501/
Fernandez‐Montoli ME, Sabadell J, Martínez‐García JM, Contreras Perez NA. Fertility‐sparing treatment for atypical endometrial hyperplasia and endometrial cancer. Cochrane Database of Systematic Reviews 2018, Issue 8. Art. No.: CD013111. DOI: 10.1002/14651858.CD013111.
https://www.cochranelibrary.com/es/cdsr/doi/10.1002/14651858.CD013111/full/es
Giannella L, Cerami LB, Setti T, et al. Prediction of Endometrial Hyperplasia and Cancer among Premenopausal Women with Abnormal Uterine Bleeding. Biomed Research International. Volume 2019 |Article ID 8598152 https://doi.org/10.1155/2019/8598152
https://www.hindawi.com/journals/bmri/2019/8598152/
Walsh C, Holschneider C, Hoang Y, Tieu K, Karlan B, Cass I. Coexisting ovarian malignancy in young women with endometrial cancer. Obstet Gynecol. 2005;106(4):693-699. doi:10.1097/01.AOG.0000172423.64995.6f
https://pubmed.ncbi.nlm.nih.gov/16199623/
