Vaginismus is a type of sexual pain disorder characterized by involuntary muscle spasms in the pelvic floor that make vaginal penetration of any kind painful or impossible. Someone with symptoms of vaginismus can't control these spasms, and the pain can range from mild to extreme. It can seriously disrupt relationships, quality of life, and self-esteem. Painful intercourse is only one sign of vaginismus.
The good news is that vaginismus is a treatable condition. Open conversations about sex and sexual dysfunction are key to finding pleasure and reducing pain. In this article, I'll explain the symptoms, causes, and treatment options for vaginismus, so you can make an informed decision about your care.
Sex and sexuality are complex topics, so if you struggle with pain or the inability to have sex, you may feel completely alone. Pain during sex is one of those topics that people don't always feel comfortable discussing. But here's what I want everyone to know—chronic pelvic pain and pain during sex is incredibly common.
Content warning: This article discusses sexual abuse and trauma. Please take care of yourself while reading.
In this article
What is Vaginismus?
The simple definition of vaginismus1 is pain during any kind of vaginal penetration—sex, tampons, toys, fingers, or vaginal exams.
People with vaginismus2 experience involuntary tensing of the pelvic floor muscles around the vagina, which leads to pain. If you've ever stopped urine flow while peeing or done kegel exercises, you've found your pelvic floor muscles. While vaginismus doesn’t interfere with arousal, if these muscles are contracted, penetration is impossible without pain.
Up to 6 percent3 of women in the U.S. have vaginismus (although this number may be higher given not everyone is comfortable discussing symptoms and many women feel shame or stigma). Some research4 suggests that rates of vaginismus are higher in geographical locations and cultures where sex and sexuality are not openly discussed.
In cases of severe vaginismus, the muscles may become so tight that nothing can enter the vagina, which is why this is sometimes referred to as a penetration disorder. This not only results in an inability to achieve penetration during sex, eliminating all penetrative intercourse, but also an inability to undergo routine a routine physical exam, like a pelvic exam or gynecologic examination.
There are several categories of vaginismus5:
- Primary: Considered lifelong vaginismus, this is a condition where pain with penetration begins early like the first time trying to use a tampon or having sexual intercourse. Pain with penetration has always been present.
- Secondary: Occurs when sex or penetration used to be possible but is no longer possible. Secondary vaginismus may happen after trauma or a medical procedure affecting pelvic floor muscles, like childbirth.
- Global vaginismus: Pain occurs every time penetration occurs.
- Situational: Pain and contractions only happen under certain conditions. For example, using a tampon may be possible, but sex is not.
Vaginismus can impact your quality of life, causing serious stress in relationships and self-esteem. It's often referred to as a psychological condition6 where fear or anxiety influences the body to tense and a physical condition where the vaginal muscles tense and contract involuntarily. But this doesn’t mean it’s acceptable for your medical provider to skip working you up and investing potential causes of your pain. Additionally, as we’ll discuss, there can be other conditions that coincide with vaginismus.
Vaginismus has a high treatment success7 rate even compared to other sexual pain disorders. This is why I'm passionate about helping women find their voices and asking for help — by talking about it and understanding what's happening in the body, it's possible to find relief.
My mission is to help women have open conversations about their body and health care needs, which is why I wrote a book about it. “Is This Normal” delves into everything you may wonder about your body, sexual health, hormones, and more but have been too embarrassed to ask.

Can I Have a “Normal” Sex Life with Vaginismus
Before we jump into therapy for vaginismus, risk factors, and what may be the cause of genital pain associated with vaginismus, I want to answer this common question I receive—can I have “normal” sex or an orgasm with vaginismus.
Firstly, there is no such thing as “normal” sex. There's what brings pleasure for you and your partner, which doesn't always include penetration.
For those with vaginismus, even finger penetration can prove problematic. But when it comes to enjoyable sexual activity, clitoral stimulation is still the primary way all vulva owners achieve orgasm. And there are many ways that people achieve orgasm and enjoy sex that doesn't include penetrative sex.
Vaginismus doesn't necessarily affect your sexual desire, but the stress and worry about not achieving pain-free penetration can certainly put you out of the mood. We understand through sexual health research that roughly eighteen percent of women can achieve orgasm by penetration alone, which means penetration isn't completely necessary for enjoyable sex.
If you are struggling with your sex life, please keep reading for successful treatment of vaginismus. But know that many women have found sexual satisfaction without penetration by working with qualified sex therapists.
What Causes Vaginismus
The causes of vaginismus aren't entirely understood, but it's generally linked to fear and anxiety surrounding sex. In fact, some research suggests that women with vaginismus8 experience more stress than women without.
For so many people (especially women), sex is as much about being emotionally turned on as physically. Often our thoughts and feelings dictate our ability to have sex — lubrication, arousal, and overall comfort — even without vaginismus.
Studies show that when a woman feels stressed or threatened in any way, the pelvic floor muscles9 respond by tensing up, making sex painful or uncomfortable. Vaginismus is like the body is constantly under stress anytime penetration is attempted.
Clearly, there's a physical manifestation10 where the vaginal muscles contract, but this response could be closely tied to fear or anxiety about the pain that only makes things worse. Plus, distress about your partner and how vaginismus may impact your relationship makes it much harder to relax and let go.
In other words, vaginismus causes are complex. It's a situation where psychological distress impacts the physical spasms and vice versa. The anxiety11 and fear of pain can stem from so many factors, including:
- Childbirth injury
- Chronic infections like UTIs, yeast infections, and STIs
- Chronic health conditions like endometriosis or adenomyosis
- Sexual abuse or trauma (directly or witnessing)
- Previously painful sexual encounters or vaginal intercourse
- Fear or shame surrounding sex from cultural or family influence
- Worry about becoming pregnant
- Painful pelvic exams in the past
But here's what I'd like you to consider if you are dealing with vaginismus: in some ways, your body is doing what it's supposed to do, protecting itself against perceived harm12, especially if there's any history of trauma or abuse. Like chronic stress, the body is stuck in the “on” position, so it needs gentle redirection and reminders that it's okay to relax. Hold space for self-compassion, and know it's not your fault.
Let's look at some of these situations a bit more closely.
Response to Physical Pain
Response to physical pain13, whether from an injury or medical condition, is also linked to vaginismus development. Treatment of vaginismus should account for pelvic trauma like the following in order to use the right interventions for vaginismus.
Childbirth
Pain or injury from childbirth can be a significant cause of secondary vaginismus. This underscores the need for sufficient postpartum support and considering working with a pelvic floor physical therapist following vaginal birth and C-section.
Chronic Pain Conditions
Chronic pain conditions like endometriosis and adenomyosis can also be a root cause of vaginismus. Both of these conditions can result in pelvic pain, including painful periods (dysmenorrhea), which may contribute to the development of vaginismus.
Low Estrogen
In certain conditions, where estrogen is low, vaginal atrophy and vaginal dryness can occur. We see this in postmenopause, as well as with early menopause, functional hypothalamic amenorrhea, primary ovarian insufficiency, and other conditions.
If sex or penetration hurts, the body's natural response is to protect itself by tensing up and avoiding the pain.
Chronic Skin Conditions and Infections
Lichen sclerosus, a chronic skin condition, is associated with sexual dysfunction and pain. In fact, approximately 60% of lichen sclerosus patients14 suffer from sexual dysfunction.
Recurrent urinary tract infections (UTIs), yeast infections, and STIs may contribute to pain and the development of vaginismus. It is important to address underlying infections in the treatment of vaginismus.
Sexual Trauma or Abuse
While studies15 are a bit mixed, sexual trauma or abuse is considered a significant factor in the development of vaginismus.
Research may be limited in that not every person who experiences abuse feels comfortable sharing details about pain during sex (or even reporting the incident), but estimates from research that more than 20 percent16 of reported cases of vaginismus also have a history of sexual abuse.
Even if someone hasn't experienced the sexual abuse directly, being exposed to others' negative sexual experiences17 or trauma can lead to reported feelings of “disgust” or phobia about sex and the body.
Living in an abusive environment18 or an abusive relationship as an adult — even without direct sexual abuse — may also influence vaginismus. Physical abuse can be a risk for developing vaginismus.
This is why working with a mental health specialist can be an important piece of addressing vaginismus, especially when considering the psychological toll the condition can take on someone’s mental health.
Sexual Dysfunction
Vaginismus can lead to what is termed sexual dysfunction. A negative or uncomfortable first sexual experience or fear of penetration and worry around sex may precede the development of vaginismus. However, it is the uncontrollable spasm that occurs with vaginismus that leads to the symptoms of pain or difficulty with penetration.
Sexual intercourse isn't necessarily the cause of vaginismus, but it's often the trigger or catalyst. For women with primary vaginismus, pain with sex may be the first sign that something is amiss. What happens next? Anxiety about having sex means the body is on high alert every time, leading to pain, and the cycle continues.
While penetrative sex may be difficult for those with vaginismus—there are many other ways to be intimate. As I detail in chapter 5 of Is This Normal, pain with sex is common, but it doesn’t have to stop you from enjoying pleasure and intimacy with your partner.
Cultural and Religious Views on Sex
The social environment we are exposed to as we grow up and learn about sex can significantly impact feelings about sexual pleasure and our bodies. One research survey19 found a close connection between vaginismus and the belief that sex was immoral or wrong. Similarly, studies have found a close link to cultures and religions with strict morality codes or shame surrounding sex and female pleasure20.
One study21 stated, “strong adherence to conservative values and strict moral related standards were found to be correlated with vaginismus and to play an active role in the defensive reflex of the pelvic floor muscle.”
Religions that forbid discussion about sex may lead to fear or lack of knowledge of sexual pleasure or anatomy, creating a difficult environment to explore and an even more difficult one to heal.
Does this mean every person who grows up in a conservative or religious household will develop vaginismus? No. Rather, this underscores how culture and societal influence can impact how we think and feel about sex, along with the development of vaginismus.
Negative beliefs and experiences—no matter where they come from — may contribute to the development of vaginismus.
How to Know if You Have Vaginismus
There is no single test for the diagnosis of vaginismus. If you have symptoms of vaginismus, it is important to visit your health care provider to be assessed.
A vaginismus diagnosis is best obtained through a visit with an OB-GYN because they will also be able to rule out underlying medical issues.
If you suspect you have symptoms of vaginismus, it is important to make an appointment with your medical provider.
Symptoms of Vaginismus
Vaginismus symptoms can present as pain with sex or pain with any type of penetration, including inserting a tampon or a speculum exam. In many cases, the pain symptom of vaginismus can be so great that someone is unable to have sex or requires additional therapies to successfully have a pap smear performed.
Patients with vaginismus may have a history of sexual, physical, or emotional trauma. Understand that your sexual history and medical history all play a role in helping you get the right diagnosis and treatment.
The Diagnostic and Statistical Manual of Mental Disorders-5 (DSM-5) states that a diagnosis of vaginismus requires at least one of the following22 symptoms present continuously for the past six months.
Symptoms of Vaginismus
- Difficulty during vaginal sex and/or penetration
- Vulvovaginal or pelvic pain, burning, or stinging during sex and/or penetration
- Involuntary spasm or contraction of pelvic muscles during penetration attempt
- Significant fear or anxiety about pain during vaginal penetration
If you meet the criteria for vaginismus, it is important to meet with a licensed health care provider.
Is it Necessary to Have a Pelvic Exam for Diagnosis?
Your doctor may or may not require a pelvic exam to diagnose vaginismus (this also depends on the degree of any associated fear and trauma). Your practitioner may visually inspect the vulva during a gynecological exam for signs of trauma, infection, or irritation to rule out any other medical conditions that could cause pain.
I want to reiterate that you have every right to say no to a pelvic exam if you aren't comfortable or it feels traumatic. Gynecological exams are an essential general health check-up, but it may take time to do so in this case. If your OB-GYN does believe it's necessary, there may be ways to make it more comfortable for you to have one. An open discussion is essential, where you feel safe and confident in the options presented.
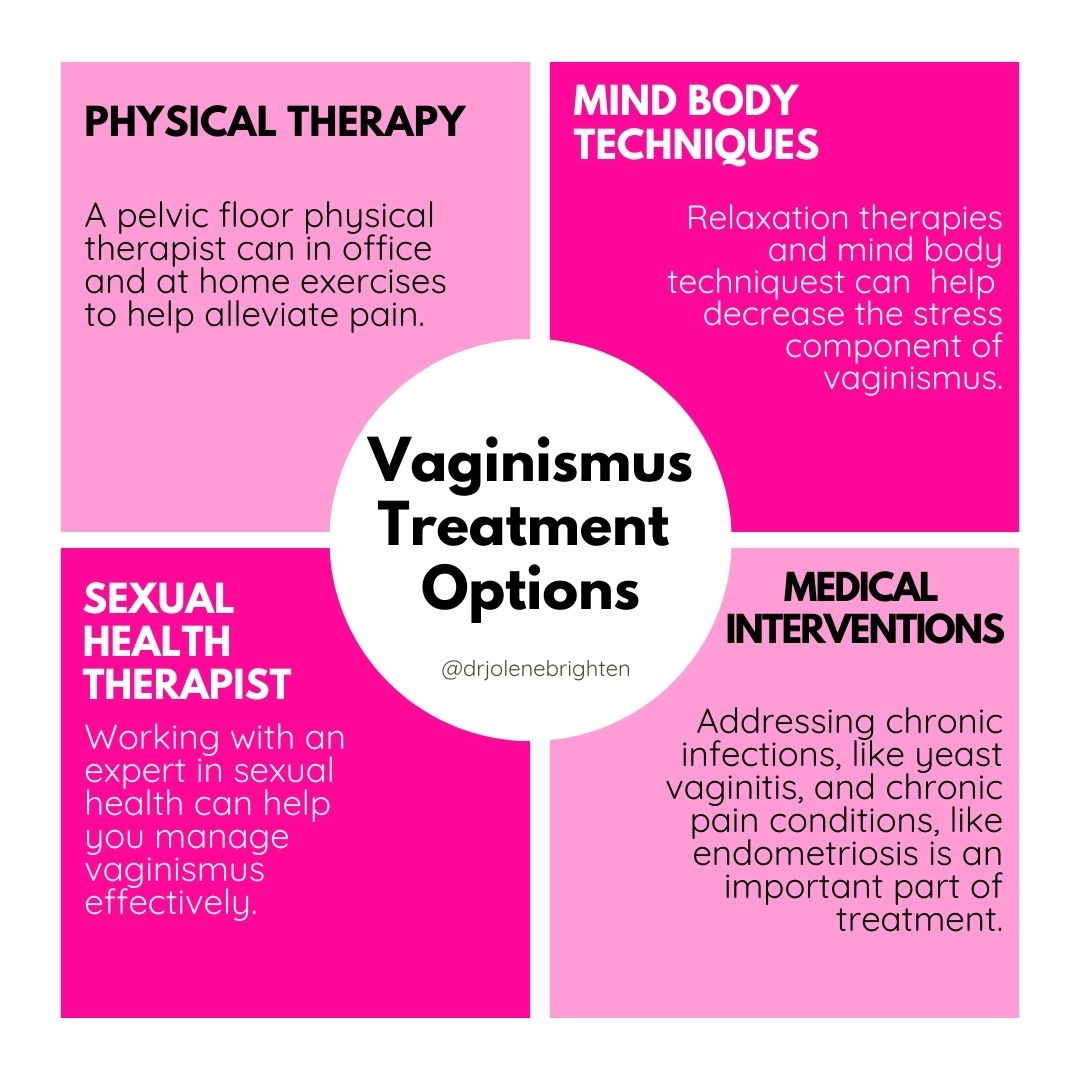
Vaginismus Treatment
The most effective vaginismus treatments include pelvic floor physical therapy, vaginal dilators, psychological support, mind-body therapies, trigger point therapy, and at home exercises. The key is to have a multidisciplinary team to offer you therapies for your specific needs.
Several available treatment techniques23 for vaginismus show success. Some focus directly on the body's physical response, like vaginal dilation or pelvic floor exercises in order to alleviate pelvic floor muscle tension. Others address the emotional and psychological aspects, like cognitive behavioral therapy or relationship counseling. Usually, treatment requires a combination of both physical and emotional approaches. And with all treatments, informed consent that allows you to make the best decision for yourself is important.
My goal is always to remove the stigma or shame associated with your body, sex, or sexuality. If you get a vaginismus diagnosis, there are treatments available that can help you find comfort and joy in sex with your partner. While a healthy sex life isn’t the only goal in vaginismus treatment, it is a very common goal among those who struggle.
Below I'll share details about the evidence-based treatments for vaginismus, but I also believe it's especially essential to consider the health of your whole body when working through a condition like vaginismus that requires such emotional energy. Supporting your foundational wellness by emphasizing restorative sleep and deep nourishment for the adrenal system through diet, lifestyle, and supplements can help you soothe the nervous system.
I've created a free Hormone Balancing Starter Kit packed with nutrition and lifestyle tips for healthy hormone balance (including a 7-day meal plan with recipes) to use as a starting point.
You and your gynecologist can decide what approach will work best for your situation, but treatment options may include the following:
Physical Therapy
Physical therapy24 focuses on the muscles in the pelvic area to help regain function, enhance movement, reduce discomfort, and alleviate anxiety.
Pelvic exercises and biofeedback are methods used to accomplish this. Pelvic floor exercises focus on strengthening and relaxing the muscles to improve tone, while biofeedback involves using technology to change muscle tension and relaxation.
Breathing relaxation techniques and manual feedback also may help reduce involuntary contractions.
Vaginal Dilators
Physical therapy may also prescribe vaginal dilator therapy to retrain the vaginal muscles to respond without spasms. Dilators are used to stretch and relax the muscles.
Vaginal dilators come in different sizes and are made from various materials to help you become more comfortable with penetration. A healthcare provider can provide guidance on the best size and techniques for your case.
Studies25 show that while vaginal dilator therapy can be helpful, working with a professional for guidance provides better results.
Botox Therapy
Botox (the same injectable used in cosmetic procedures) can be an effective pharmacological treatment for vaginismus. An early study26 found that a botox injection in a muscle found in the perineum successfully helped women have sex with their partners—and the success continued throughout the follow-up period of 8 to 14 months. Another study27 reported a 75% success rate of pain-free sex for women that lasted an average of 12 months after receiving an injection.
A recent meta-analysis28 found that although more studies are needed, botox injections may significantly improve pelvic floor pressure, resulting in improved quality of life for women with pelvic pain.
Topical Therapy
Lidocaine is a numbing cream that may occasionally help with pain with sex or medical exams. The cream does not address muscle contractions, so it's not commonly suggested in most research studies on treatment approaches.
Sexual Counseling
Sex therapy29 can open up communication and be a safe space to discuss all the fears and anxiety that come up—from pain to negative connotations about sex or even sex education. Research reports this type of support can provide excellent results for people with vaginismus.
You can use the American Association of Sexuality, Educators, Counselors, and Therapists website to find a practitioner to work with or ask your medical provider for a referral.
In many cases of vaginismus, relationship factors can affect you or your partner. This is where working with a licensed therapist or counselor can help your mental, relationship, and sexual health—enabling you to have pain-free intercourse.
Cognitive Behavioral Therapy
Cognitive behavior therapy (CBT) or cognitive therapy is a type of psychotherapy that examines how our thoughts, beliefs, and attitudes can influence our feelings and actions. It's a way of addressing thought patterns that cause distress and anxiety and creating alternative coping behaviors that help.
In one study30, CBT helped 81% of women with vaginismus successfully have sex and feel more confident and valuable in their sexual relationships and as individuals.
Additional Nervous System Support
Because there is a nervous system component and supporting a calm state can be so beneficial for those struggling with vaginismus, I utilize a couple of supplements in my practice, along with the treatment options listed above.
Magnesium is a mineral that can help with muscle tension and relaxation. It can also be beneficial when inflammation or stress is present. I recommend magnesium glycinate as the best absorbed form, which is what you’ll find in Magnesium Plus.
L-theanine, passion flower, and Ashwagandha are all herbs and nutrients that can help with nervous system relaxation. When combined with certain B vitamins, they can help bring your body into a calm, relaxed state so you can better deal with stress. You’ll find this combination in Adrenal Calm by Dr. Brighten.
Is Vaginismus Curable
With the right support and treatment, vaginismus is curable31. How quickly you find relief depends on the severity, how long it's been present, and how often someone follows up and continues with treatment.
One study32 found that treatment with a multi-modality program resulted in pain-free sexual intercourse for an average of 93% of participants with primary vaginismus. Severe vaginismus meant a longer treatment time was needed, but healing was still achieved in most cases.
Patience, self-compassion, and open communication with your partner and healthcare provider are all critical factors in treating vaginismus.
Working with a licensed healthcare provider who is experienced in the treatment of vaginismus is key in helping resolve this condition.
References
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7169926 ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7169926 ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7169926 ↩︎
- https://www.tandfonline.com/doi/full/10.1080/14681994.2021.2007233 ↩︎
- https://www.tandfonline.com/doi/full/10.1080/14681994.2021.2007233 ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5440634 ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5440634 ↩︎
- https://www.tandfonline.com/doi/full/10.1080/14681994.2021.2007233 ↩︎
- https://www.tandfonline.com/doi/full/10.1080/14681994.2021.2007233 ↩︎
- https://www.tandfonline.com/doi/full/10.1080/14681994.2021.2007233 ↩︎
- https://www.tandfonline.com/doi/full/10.1080/14681994.2021.2007233 ↩︎
- https://www.tandfonline.com/doi/full/10.1080/14681994.2021.2007233 ↩︎
- https://journals.sagepub.com/doi/10.2217/WHE.10.46 ↩︎
- https://www.sciencedirect.com/science/article/abs/pii/S1743609522015454 ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7169926 ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7169926 ↩︎
- https://www.tandfonline.com/doi/full/10.1080/14681994.2021.2007233 ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7169926 ↩︎
- https://www.tandfonline.com/doi/full/10.1080/14681994.2021.2007233 ↩︎
- https://www.tandfonline.com/doi/full/10.1080/14681994.2021.2007233 ↩︎
- https://www.tandfonline.com/doi/full/10.1080/14681994.2021.2007233 ↩︎
- https://www.sciencedirect.com/science/article/pii/S2050116121000878 ↩︎
- https://pubmed.ncbi.nlm.nih.gov/24894201/ ↩︎
- https://journals.sagepub.com/doi/full/10.2217 ↩︎
- https://bmcwomenshealth.biomedcentral.com/articles/10.1186/s12905-015-0201-6 ↩︎
- https://pubmed.ncbi.nlm.nih.gov/17012454/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/15516379/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/35362767/ ↩︎
- https://www.tandfonline.com/doi/full/10.1080/14681994.2021.2007233 ↩︎
- https://www.tandfonline.com/doi/full/10.1080/14681994.2021.2007233 ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7169926 ↩︎
- https://www.sciencedirect.com/science/article/pii/S2050116121000878 ↩︎
