Let’s talk about sex—specially sexual health. So much about sexual health is kept quiet, but if you read my articles or follow me on Instagram, you know I’m all about open conversations about sex and intimacy—and that includes the not-so-fun topic of sexually transmitted infections (STIs).
We need to be more open about safer sex because awareness and education are key for preventing STIs in the first place. The more you know, the more empowered you will be regarding your own sexual health. And here’s the truth: The CDC1 is reporting record numbers of STIs in recent years, so you want to protect yourself.
In this article, you’ll get the scoop on STIs, including what they are, recognizing the signs and symptoms, and what treatment options are available if needed. And when in doubt, I want to encourage you to meet with your provider.
In this article:
What Are STIs?
STIs2 are infections caused by bacteria, viruses, or parasites passed from one person to another during sexual activity, including oral, vaginal, or anal sex. Some can also be passed by close skin-to-skin contact.
There are many types of STIs with varying levels of severity. Some can have no symptoms at all, while others are more noticeable. Luckily, treatments are available for many STIs, but others stay with you for life. Early intervention is critical to avoid some of the more severe health problems listed below.
Are STIs and STDs the Same Thing?
STIs and STDs (sexually transmitted diseases) are often used interchangeably but are technically different. Infection is the initial part of illness when the bacteria, virus, or parasite enters your body, but disease is the term used when the condition progresses, as is the case in warts or cancer..
So an STD is the resulting disease caused by an STI. One example is human papillomavirus (HPV). HPV is an infection that often resolves on its own, but certain types of HPV can lead to cellular changes that develop into cancer. Another example is hepatitis, which is caused by a virus and can lead to liver cancer.
How Are STIs Transmitted?
As I mentioned earlier, STIs are transmitted through unprotected sexual activity. Any intimate contact that includes genital touch or bodily fluid like sperm, saliva, or blood could spread STIs.
Foreplay that involves close skin-to-skin contact could also transmit certain STIs like herpes (more on this below).
But certain conditions considered STIs can also be spread via non-sexual contact. Hepatitis B can occur through contact with infected fluids.

Who is Affected by STIs?
Studies3 estimate that more than 25 million people are infected by STIs annually, and nearly half of those infected are between the ages of 15 and 24.
While STIs don’t discriminate and can affect people of all backgrounds, health inequities still exist. Certain minority groups4, especially women within these groups, experience higher rates of STIs because of challenges associated with lack of access to quality health care, distrust or discrimination from health care providers, or overall higher rates of STIs within a community. This information shouldn’t be used to pass judgment on these individuals, but rather, to look at how we can improve medical services and examine the public health issues that need to be addressed in these communities.
Can STIs Cause Health Problems?
Some STIs cause no symptoms and go away on their own. Others can cause significant health problems if left untreated. There are also types of STIs that can be managed with medications but can’t be cured. Currently, trichomonas, gonorrhea, chlamydia, and syphilis are curable with treatment5.
According to the National Institute of Health6 (NIH), some of the health problems associated with STIs include:
- Reproductive health concerns like infertility or maintaining the pregnancy
- Birth defects or infant death if left untreated during pregnancy
- Organ damage
- Certain types of cancer
- Pelvic inflammatory disease7 (PID) a bacterial infection that spreads to the ovaries, fallopian tubes, and uterus.
- Ectopic or tubal pregnancies
How Do STIs Affect Women Differently?
While STIs affect all genders, women or people with female anatomy are impacted differently. Vaginal tissue is thin, making it easier for bacteria or viruses to enter the body. Additionally, women may not have some telltale signs of infection like men do, so they may go longer without treatment. In fact, many STIs can be “silent” or in other words, not show symptoms right away, which is one reason why regular screening is so important.
Also, since women have discharge, occasional itchiness, or other symptoms that could be chalked up to non-STI infections like yeast infections, they may assume it’s something else and not get prompt treatment.
Luckily, research8 shows that women are more likely to visit their doctor regularly, and you can include regular screenings for sexual health (which we will discuss below) as part of your annual check-up.
What Are the Symptoms and Signs of STIs?
Symptoms can include:
- Sores, blisters, or warts on genitals or mouth
- Painful or frequent urination
- Unusual discharge
- Itching or burning in the genital or anal area
- Pain with sex
- Changes in vaginal odor
- Fever
STIs can be asymptomatic or more noticeable. Some symptoms can look like urinary tract infections, bacterial vaginosis, or yeast infections, so checking with your doctor anytime you notice any changes is important so you can get the right treatment.
What Are the Different Types of STIs?
The most common types of STIs include:
- Chlamydia
- Gonorrhea
- Hepatitis B and C
- Human Immunodeficiency Virus (HIV)
- Human Papillomavirus (HPV)
- Herpes
- Syphilis
- Pubic Lice
- Trichomoniasis
Chlamydia
Chlamydia9 is caused by a bacteria called Chlamydia trachomatis and is one of the more common STIs—up almost 20% between 2015 and 2019, according to the CDC10. It’s passed via sexual contact but can also infect a baby during childbirth.
Chlamydia can be completely asymptomatic or take weeks to show up, so it can easily be passed unknowingly with unprotected sex. If symptoms are present, they can include:
- Strong-smelling vaginal discharge
- Burning when you pee
- Pain with sex
- Fever
- Upset stomach
- Lower abdominal pain
Sometimes the bacteria can infect the anal area, so pain, discharge, or bleeding can also appear in the rectum.
If untreated, chlamydia can cause pelvic inflammatory disease (PID) as it spreads to the uterus and fallopian tubes, which can cause infertility.
Luckily, chlamydia is easily treated with antibiotics, but starting treatment early is essential to prevent long-term damage.
Gonorrhea
Like chlamydia, gonorrhea is caused by bacteria and passed via sexual contact or from mother to baby in childbirth. It also has minimal symptoms in early phases but can include abnormal bleeding, increased discharge, or pain while urinating as it progresses. Gonorrhea numbers are also rising in the US, up more than 50% since 2014, according to the CDC11.
Untreated, gonorrhea can also cause PID and infertility. The good news is, gonorrhea generally responds well to antibiotics. It’s important to note that research12 points towards gonorrhea becoming more resistant to antibiotics, so some cases can be more challenging to treat and may require prolonged treatment.
Hepatitis B and C
There are several types of hepatitis, but hepatitis B and hepatitis C can be transmitted via sex. Hepatitis means inflammation of the liver, and symptoms like stomach pain or yellowing of the skin and eyes usually don’t show until the disease progresses.
Aside from practicing safe sex, hepatitis B has a vaccine for prevention. While hepatitis C doesn’t have a vaccine, curative treatment is available.
It’s also important to note that hepatitis B and C can be contracted via shared needles.
Human Immunodeficiency Virus (HIV)
HIV attacks and weakens the immune system. It’s spread via unprotected sex or from mom to baby during pregnancy, delivery, or breastfeeding. Having other STIs13 can increase the chance of getting an infection with HIV.
Early symptoms of HIV can look like the flu, including fever, aches, rash, night sweats, chills, but not everyone feels sick in the early phases. Eventually, the immune system progressively gets weaker and unable to fight off infections. AIDS is the most severe stage of HIV, but having HIV does not automatically mean a person will end up with AIDS.
While HIV can’t be cured, people can still live long, healthy lives thanks to research14 and progress with antiretroviral therapies. There are also medications available for people in high-risk groups for prevention.
Human Papillomavirus (HPV)
HPV refers to a group of more than 200 viruses, but about 40 of them are spread through sexual or skin-to-skin contact. In many cases, HPV resolves on its own, but some of the HPV viruses can cause cervical, anal, oral, throat, and other cancers.
It’s so common that it’s estimated that nearly every person who is sexually active has had at least one strain of HPV at some point.
HPV can cause genital warts but often doesn’t lead to other symptoms. Since HPV can cause cancer, it’s so important to get screened for HPV along with your pap test. There’s also a vaccine for certain strains of HPV that you can discuss with your doctor.
Herpes
Herpes simplex (HSV) is a virus that lives in the nerves and causes sores. HSV-1 is linked to oral cold sores, and HSV-215 is usually found on genitals, buttocks, thighs, or rectum. It’s passed via skin-to-skin or sexual contact, even if there aren’t any sores. Moms can also pass it to babies in childbirth, and your doctor may recommend a cesarean delivery if you have an outbreak close to your due date.
The main symptom is the sores themselves, although sometimes people can feel fatigued around the time of the outbreak. Some people can carry the virus but aren’t even aware they have it.
Herpes can never be cured, but it can be treated with antiviral drugs that shorten or reduce how often outbreaks occur. In some instances, your doctor may recommend preventative antivirals for procedures or ongoing when the outbreaks are frequent.
Syphilis
Syphilis is caused by bacteria and spread by unprotected sex. Once again, the CDC16 tells us that rates are growing fast, up 74% between 2015 and 2019! Luckily it can be treated with antibiotics.
Syphilis can be pretty severe if left untreated. Early phases of syphilis are characterized by sores in the genital area or around the mouth that eventually go away. Over time if untreated, syphilis progresses to secondary syphilis17 and causes rash and hair loss.
Eventually, syphilis can progress even further and cause significant damage to the heart, brain, and even death—but early treatment stops progression before getting close to this point.
Pubic Lice
Pubic lice (AKA crabs) are itchy parasites that primarily live in pubic hair. You can pick up pubic lice from skin-to-skin contact, clothes, or bedding. Symptoms are intense itching but can be treated with lotions that kill the eggs and lice.
Trichomoniasis
Trichomoniasis is another parasite transmitted during sex that causes vaginal infections with symptoms like:
- Gray or green discharge
- Pain or discomfort during sex
- Painful urination
- Unusual vaginal odor
- Burning in the vagina or vulva
Sometimes there are no symptoms, and it’s treated with antibiotics.
I’ve written an article on discharge to help you understand what the different types might be a sign of.
Is Monkeypox an STI?
Monkeypox is a viral illness. Symptoms of monkeypox18 include fever, headaches, swollen lymph nodes, and rash. The rash, which looks similar to a blister or pimple, can show up on the hands, face, feet, and genitals. Because it is common for the rash to present on the anus or other genitals, many people have mistakenly thought it to be an STI.
Monkeypox is not an STI. It can be contracted through close contact, which includes sex, but can also occur through shaking hands, hugging, and other activities that include skin-to-skin contact. The virus can also be transmitted through coming into contact with respiratory droplets or objects that are contaminated with the virus.
Can You Prevent STIs?
If you research STIs, you’ll often see some websites tell you that the best way to prevent STIs is to not have sex, but that’s just not realistic for most people. STI prevention ties back to making safe sex choices, using protection, communication with your partner, and getting tested for STIs regularly.
Testing for STIs
Regular STI testing is crucial for preventing STIs because you are less likely to pass something to a sexual partner. Testing also can help catch an infection earlier.
If you are sexually active and have a new sexual partner, getting tested regularly is extra important because some STIs don’t have symptoms as you just read. Open communication with your partners about sex and making testing a part of your relationship can keep you safe.
If you are starting a new relationship, have multiple partners, or are experiencing symptoms, testing is important. Testing before having sex with someone the first time (and asking them to do the same) is an important safe sex practice and allows you to fully understand what you are consenting to. If you change partners, get tested for STIs. If you are non-monogamous, consider scheduling annual testing so that you are sure this is done at least yearly.
Tests for STIs include:
- Pelvic or physical examinations to look for signs of infections
- Blood tests
- Urine tests
- Fluid or tissue samples
Pap tests are a screening tool that looks for cell changes related to cancer. They are absolutely important, but they don’t test for STIs.
Talk to Your Doctor About vaccinations Against STIs
As I mentioned earlier, vaccines are available for Hepatitis B and HPV. Depending on your age, you may have received them as part of the regular vaccine schedule, but you can discuss both of these vaccines in more detail with your doctor. If you have concerns about vaccines, talk with your doctor about your individual needs.
Use Protection and Practice Safe Sex
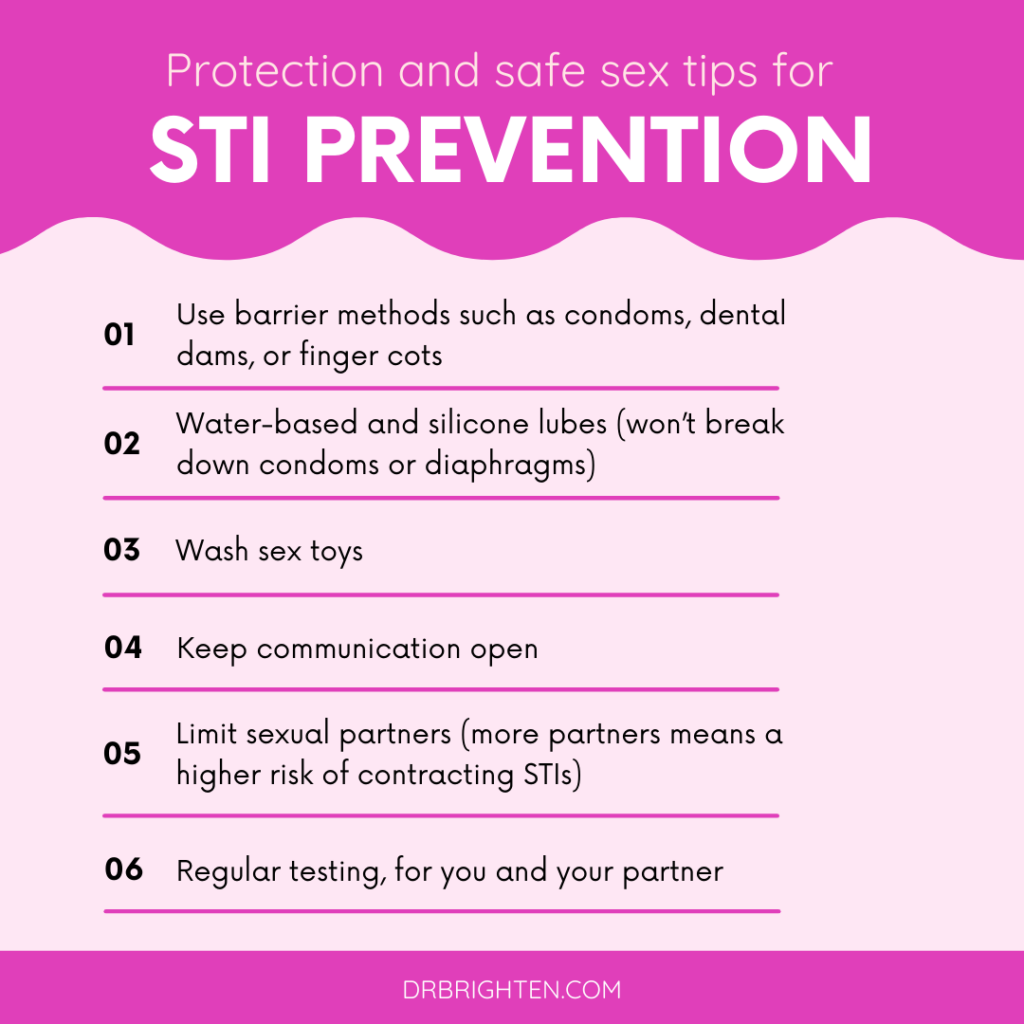
Protection and safe sex are your best tools for STI prevention, including:
- Condoms, dental dams, finger cots are examples of barrier methods that can reduce STI transmission (birth control or IUDs are contraceptives but don’t protect you against STIs)
- Water-based and silicone lubes (won’t break down condoms or diaphragms)
- Wash sex toys
- Keep the communication open
- Limit sexual partners (more partners means a higher risk of contracting STIs)
- Regular testing, for you and your partner
Also, while period sex has many benefits like reducing period cramps, it may slightly increase the chance of passing or getting STIs. Period blood is more alkaline than the pH of the vagina, making it easier for bacteria or other pathogens to infect. The ideal would be that both partners are tested so that you aren’t having sex if you have an infection. However, like any other time you want to be safe, use a barrier method.
Lube isn’t always part of the STI talk, but it is a very important preventative measure. Lubrication prevents tissue damage, which may prevent organisms from causing an infection. In addition to barriers and testing, make sure you’re using the right lube for your adventures.
Early Treatment for STIs is Critical for Your Health
Each of the STIs has its own treatment. Bacterial-based infections can be treated with antibiotics. Antivirals reduce the viral load for STIs like herpes, and HIV can be treated long-term with antiretrovirals.
The biggest piece of advice I can give you for STI treatment is to start early to avoid any long-term health impacts—so get tested regularly and make sure to communicate with your partners. And if your partner can’t or won’t talk about STI prevention—don’t do it, it’s not worth it.
STIs: The Big Takeaways
- STIs are passed during sexual activity or close intimate contact.
- There are many different types of STIs, and anyone can become infected. Rates of STIs like syphilis, gonorrhea, and chlamydia are on the rise.
- Monkeypox is not an STI.
- Most STIs can be treated with medications, but they can lead to serious health concerns like infertility or cancer if left untreated.
- Open communication, safer sex, and regular testing are essential for protecting yourself and your partner.
The more we talk about sex, the less of a stigma about all that’s involved, including STIs.
References
- https://www.cdc.gov/std/statistics/2019/default.htm ↩︎
- https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(17)30310-9/fulltext ↩︎
- https://pubmed.ncbi.nlm.nih.gov/33492089/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/33985698/ ↩︎
- https://www.who.int/news-room/fact-sheets/detail/sexually-transmitted-infections-(stis)#:~:text=Eight%20pathogens%20are%20linked%20to,and%20human%20papillomavirus%20(HPV) ↩︎
- https://www.niaid.nih.gov/diseases-conditions/sexually-transmitted-diseases ↩︎
- https://www.cdc.gov/std/pid/stdfact-pid.htm ↩︎
- https://www.cdc.gov/nchs/data/databriefs/db408-H.pdf ↩︎
- https://pubmed.ncbi.nlm.nih.gov/32093536/ ↩︎
- https://www.cdc.gov/std/statistics/2019/default.htm ↩︎
- https://www.cdc.gov/std/statistics/2019/default.htm ↩︎
- https://pubmed.ncbi.nlm.nih.gov/31119616/ ↩︎
- https://www.cdc.gov/std/statistics/2019/default.htm ↩︎
- https://pubmed.ncbi.nlm.nih.gov/30030792/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/32119314/ ↩︎
- https://www.cdc.gov/std/statistics/2019/default.htm ↩︎
- https://onlinelibrary.wiley.com/doi/10.1111/jmwh.13241 ↩︎
- https://www.who.int/news-room/questions-and-answers/item/monkeypox?gclid=CjwKCAjwsfuYBhAZEiwA5a6CDEWkjIG4-ii8r2MSOFduAeul_Hoiv5vsSpVHkVHMXKg5HTXCiYQoOxoCmvUQAvD_BwE ↩︎
