Struggling with mood swings, anxiety, or depression before your period and wondering if it’s more than just “PMS”? You’re not alone. In this episode of The Dr. Brighten Show, I sit down with Dr. Sarah Hill, trailblazing researcher and author of This Is Your Brain on Birth Control and The Period Brain, to uncover the hidden symptoms of PMDD and PMS that most doctors miss. We dive deep into how hormones shape your brain, why birth control may not be the fix you think it is, and the groundbreaking science behind progesterone, progestins, and your mental health.
This conversation reveals the truth about hormone sensitivity, trauma, neurodivergence, and perimenopause, offering insights that could transform the way you understand your body and your brain.
Symptoms of PMDD and PMS: What You’ll Learn in This Episode
- Why almost 70% of women with major depressive disorder or bipolar disorder report worsening symptoms before their period.
- How progesterone’s metabolite, allopregnanolone, acts like a superhero for your brain and why progestins can’t do the same.
- The shocking reason why teen girls on birth control have up to 6x higher suicide risk than peers who don’t use it.
- The truth behind the phrase “Franken-hormones” and why synthetic progestins act more like testosterone than progesterone.
- How the HPA axis (your stress system) is disrupted by hormonal birth control and why this blunts your ability to cope with stress.
- Why perimenopause is the most dangerous time for women’s mental health, including peak rates of anxiety and suicide.
- The surprising research showing women choose sexier outfits around ovulation and what this says about your brain’s natural cycles.
- Why ovulation isn’t “optional” and how suppressing it robs your body of critical brain-protective hormones.
- The role of trauma and high ACE scores in increasing risk for PMDD and how it rewires the stress response.
- What studies reveal about the link between neurodivergence (ADHD, autism) and PMDD, with nearly 90% of autistic women reporting symptoms.
- Why the “bikini medicine” model of research has left women without answers for decades and what needs to change.
- Treatments that can help: from SSRIs dosed only in the luteal phase, to lifestyle interventions like exercise, vagus nerve stimulation, and saffron.
Diving Deeper into Symptoms of PMDD and PMS
PMDD isn’t just “bad PMS.” It’s a debilitating condition tied to hormonal sensitivity, not necessarily hormone levels. In this episode, Dr. Sarah Hill explains how changes in progesterone and estrogen reshape your brain each month—sometimes making you feel powerful and radiant, and other times sending you into a spiral of anxiety or despair. We break down:
- How estrogen acts like miracle grow in the brain, boosting sensory awareness and even attraction cues.
- Why the brain’s GABA receptors struggle to adapt in women with PMDD, making hormonal shifts feel like “falling off a cliff.”
- The difference between PMS and PMDD, including suicidal ideation as a defining feature.
- Why progesterone therapy can be life-changing in perimenopause, yet so few doctors prescribe it.
- The gaps in women’s health research, where women are often only studied in the first 9 days of the cycle to “make them more like men.”
This episode will help you connect the dots between your cycle, your brain, and your mood, while offering actionable ways to navigate PMDD and PMS with science-backed strategies.

About the Guest:
Dr. Sarah E. Hill is an award-winning researcher, professor, and bestselling author whose work is transforming how we understand women’s brains and hormones. With over 100 scientific publications, she is the author of This Is Your Brain on Birth Control and The Period Brain. Dr. Hill’s groundbreaking research uncovers how hormones shape mood, behavior, and mental health across a woman’s lifespan, making her one of today’s leading voices in women’s health and psychology. Her work has been featured in outlets like The New York Times, The Washington Post, and Time Magazine, establishing her as a trusted authority on the science of women’s health.
This Episode Is Brought to You By
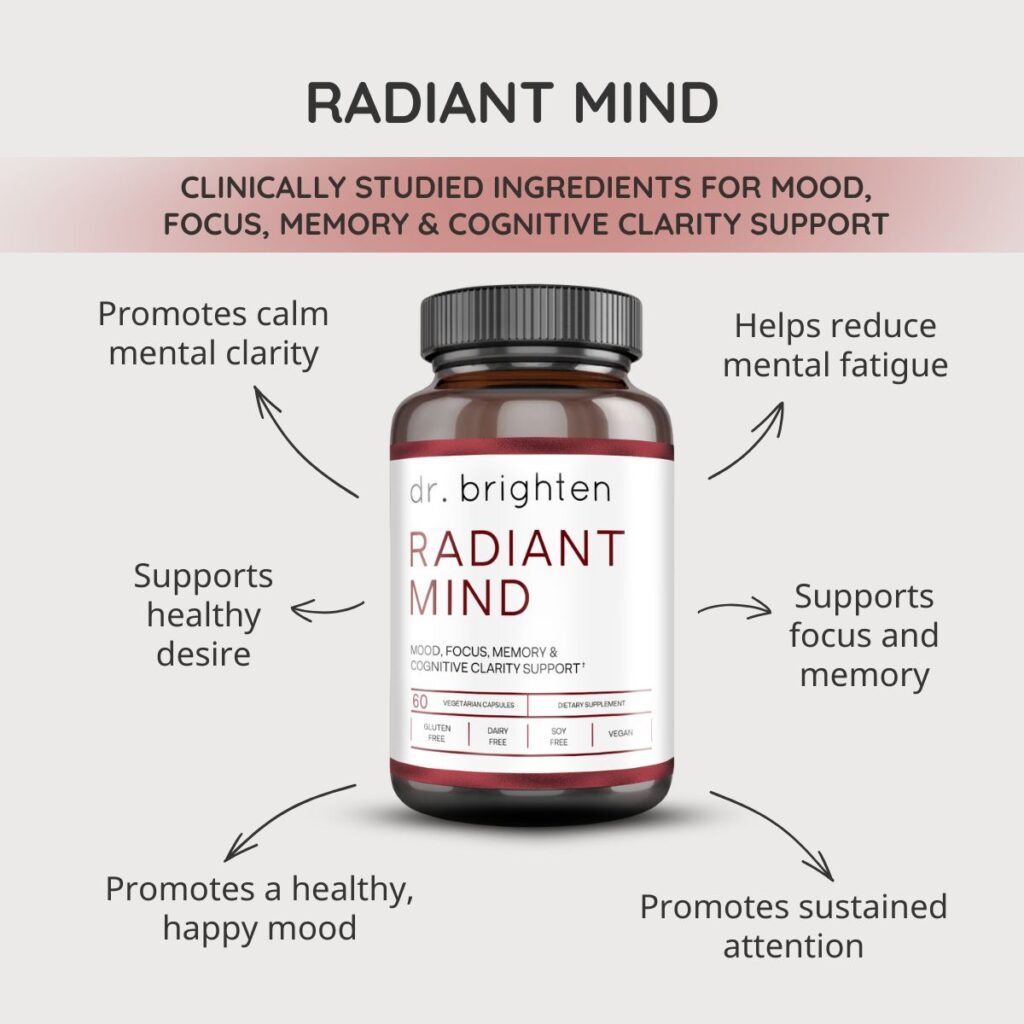
Dr. Brighten Essentials Radiant Mind—a science-backed formula created to support women’s brain health through every stage of life. If you’ve ever felt the brain fog of perimenopause or noticed how ADHD can amplify challenges with focus, memory, mood, or sleep, you’re not alone. Radiant Mind combines clinically studied saffron extract, Bacognize® Bacopa, Cognizin® Citicoline, and zinc to help nourish your brain chemistry and support clarity, calm, and resilience. And for a limited time, when you order Radiant Mind, you’ll also receive a free bottle of our best-selling Magnesium Plus—the perfect partner for restorative sleep and steady mood. Learn more at drbrighten.com/radiant.
Sunlighten Saunas
Want a gentle, science-forward way to sweat, recover, and unwind? At Sunlighten, infrared saunas deliver soothing heat that supports relaxation, muscle recovery, and deep, comfortable sweating—without the stifling temps of traditional saunas. With low-EMF tech and options for near, mid, and far infrared, you get a calm, restorative session tailored to your goals.
Exclusive for podcast listeners: use the code DRBRIGHTEN to save up to $1,400 on your sauna
Links Mentioned in This Episode
- This Is Your Brain on Birth Control by Dr. Sarah Hill
- The Period Brain by Dr. Sarah Hill
- Guide to Treating PMDD (Premenstrual Dysphoric Disorder) A practical guide to understanding PMDD and the most effective strategies to find relief.
- Histamine and PMDD: The Hidden Link Worsening Your Symptoms Discover how histamine intolerance may secretly intensify PMDD symptoms and what to do about it.
- ADHD and PMDD Hormone Connection Learn how ADHD and PMDD intersect, and why hormones make symptoms so much harder to manage.
- Progesterone Intolerance: Symptoms, Causes & What To Do About It Unpack the real reasons behind progesterone intolerance and how to ease the side effects.
- PMDD in Autistic Women: Symptoms, Causes & Effective Solutions Explore why autistic women are more likely to experience PMDD and solutions that can help.
- How Hormones Affect Mood Throughout Your Menstrual Cycle See how monthly hormone shifts change your mood, focus, and energy—and how to work with them.
- Sleep Problems Before and During Your Period Find out why your period disrupts sleep and the science-backed steps to get deeper rest.
- Skovlund CW, Mørch LS, Kessing LV, Lidegaard Ø. Association of Hormonal Contraception With Depression. JAMA Psychiatry. 2016 Nov 1;73(11):1154-1162. doi: 10.1001/jamapsychiatry.2016.2387. Erratum in: JAMA Psychiatry. 2017 Jul 1;74(7):764. doi: 10.1001/jamapsychiatry.2017.1446. PMID: 27680324.
- Hantsoo L, et al., The role of the hypothalamic-pituitary-adrenal axis in depression across the female reproductive lifecycle: current knowledge and future directions. Front Endocrinol (Lausanne). 2023 Dec 12;14:1295261. doi: 10.3389/fendo.2023.1295261. PMID: 38149098; PMCID: PMC10750128.
- Rajabi F, Rahimi M, Sharbafchizadeh MR, Tarrahi MJ. Saffron for the Management of Premenstrual Dysphoric Disorder: A Randomized Controlled Trial. Adv Biomed Res. 2020 Oct 30;9:60. doi: 10.4103/abr.abr_49_20. PMID: 33457343; PMCID: PMC7792881.
Other Episodes Not to Miss
- Unlocking the Power of the Menstrual Cycle: Hormone Health, PMDD & Period Care | Ashley Greene Discover how understanding your menstrual cycle can transform hormone health, period care, and even PMDD.
- Progesterone Side Effects & Intolerance: Why You Feel Worse on Progesterone| Dr. Jolene Brighten Learn why some women feel worse on progesterone and how to tell if you’re dealing with progesterone intolerance.
- Feel Sick Before Your Period? It Might Be Menstrual Flu and You Can Fix It | Dr. Jolene Brighten Unpack the surprising reason you feel flu-like before your period and what you can do to fix menstrual flu.
- How to Sleep Better by Fixing Blood Sugar and Sleep Disruptors | Dr. Jolene Brighten Explore how blood sugar crashes and hidden disruptors wreck your sleep—and how to finally rest better.
- Top AuDHD Expert: Shocking Risks of Undiagnosed Female ADHD & Autism | Dr. Samantha Hiew Hear the truth about the hidden risks of undiagnosed ADHD and autism in women, and why so many are missed.
- Menopause Brain Fog Is Real: 7 Science-Backed Ways To Clear It | Dr. Jolene Brighten Find out why menopause brain fog happens and 7 proven strategies to sharpen focus and memory.
- Side Effects of Stopping The Birth Control Pill: How to Stop Mood Swings, Acne & More | Dr. Jolene Brighten Get the inside scoop on what really happens when you stop the pill and how to smooth the transition.
- The Medical System Is Misleading Women About Symptoms of Menopause | Dr. Tara Scott Discover the myths and misinformation around menopause symptoms and what women really need to know.
- ADHD Burnout? Your Hormones Might Be Sabotaging You Uncover how shifting hormones fuel ADHD burnout and what to do to reclaim your energy and focus.
FAQ: Symptoms of PMDD and Treatment
What are the early symptoms of PMDD?
Early symptoms of PMDD often look like PMS but are more severe. They can include mood swings, anxiety, irritability, fatigue, food cravings, and difficulty concentrating that begin in the luteal phase (the two weeks before your period) and resolve once bleeding starts.
Can nutritional supplements support women experiencing PMDD symptoms?
While supplements are not a treatment or cure for PMDD, many women find that supporting their overall brain and hormone health can make a difference in how they feel. Nutrients like saffron, bacopa, citicoline, and zinc — the ingredients in Radiant Mind from Dr. Brighten Essentials — are researched for their role in supporting mood, focus, and concentration. By nourishing the brain and promoting calm clarity, supplements like Radiant Mind may be a helpful part of a comprehensive self-care plan that also includes sleep, nutrition, movement, and professional medical guidance.
How can you tell the difference between PMS and PMDD?
While PMS may cause mild mood and physical changes, PMDD includes debilitating mood symptoms such as intense sadness, rage, or even suicidal thoughts. PMDD interferes with daily life, work, and relationships, whereas PMS is usually manageable.
Is saffron helpful for PMDD symptoms?
Research suggests saffron may play a role in supporting mood and emotional well-being, which can be especially valuable during the luteal phase when PMDD symptoms appear. In a randomized controlled trial, women with premenstrual complaints who took 30 mg of saffron daily experienced significant improvements in mood compared to placebo. The researchers of this study concluded, “based on the findings of this study, saffron was an efficacious herbal agent for the treatment of PMDD with minimal adverse effects”.
Additional studies have also shown saffron to be supportive for stress resilience and emotional balance.
While saffron is not a treatment or cure for PMDD, it may be a helpful part of a broader self-care strategy. Radiant Mind by Dr. Brighten Essentials includes saffron extract (affron®), alongside bacopa, citicoline, and zinc, to provide nutritional support for mood, focus, and concentration. For women navigating cyclical mood changes, formulations like Radiant Mind can complement lifestyle practices such as exercise, sleep optimization, and stress management, always in consultation with a healthcare provider.
Can birth control pills cause or worsen PMDD?
Research shows that for some women, hormonal birth control can blunt the stress response and increase risks of depression or anxiety. In adolescents, studies found a six-fold increase in suicide risk among those using the pill. While some women find birth control helps, others experience worsening PMDD symptoms.
What treatments are available for PMDD?
Treatment depends on individual hormone sensitivity. Options include:
- SSRIs, sometimes taken only during the luteal phase
- Bioidentical progesterone therapy
- Lifestyle approaches such as exercise, improved sleep, vagus nerve stimulation, and saffron supplementation
- Cognitive behavioral therapy (CBT) and neurofeedback
Is PMDD linked to neurodivergence or trauma?
Yes. Studies suggest nearly 90% of autistic women and almost half of women with ADHD report PMDD. A history of trauma or high ACE (adverse childhood experience) scores also increases risk by disrupting the stress system and hormone sensitivity. See the episode links for resources specific to this.
Does progesterone therapy help with PMDD?
For some women, yes. Progesterone and its metabolite allopregnanolone support calm, resilience, and neuroplasticity in the brain. Unlike synthetic progestins, bioidentical progesterone can restore the soothing, GABA-supporting effects that are often missing in PMDD.
Transcript
[00:00:00] Perimenopause is a time when most women get worsening of everything. PMS has been used to describe even minor experiences that we have. PMDD is more serious. It's generally a suicidal ideation. Women who've been through traumatic events do have a greater risk of developing PMDD, and it's pretty significant.
Studies show that almost 70% of women with major depressive disorder and bipolar disorder experience exacerbation premenstrually.
It usually takes women a very long time to get A-P-M-D-D diagnosis. Those things may resolve and feel better once you're in full menopause. When you're in this state of hormonal transition, things can get a whole lot worse.
Dr. Sarah E. Hill.
Is a trailblazing researcher, award-winning professor and bestselling author uncovering how women's hormones shape their brains bodies and lives
with over 100 scientific publications and viral books. Like this Is Your Brain on Birth Control and the upcoming The Period Brain. Dr. Hill is transforming the way we understand female [00:01:00] health, one breakthrough at a time.
We're wondering why they're leaving their career. They regret being a mom. We just took a really hard time and we just threw
gasoline on that. It causes all kinds of changes throughout the body outside of the uterus. People almost don't wanna listen to it because it just seems to very fairy. What we find is that there is a greater risk of being.
Welcome to the Dr. Brighten Show, where we burn the BS in women's health to the ground. I'm your host, Dr. Jolene Brighten, and if you've ever been dismissed, told your symptoms are normal or just in your head or been told just to deal with it, this show is for you. And if while listening to this, you decide you like this kind of content, I invite you to head over to dr Brighten.com where you'll find free guides, twice weekly podcast releases, and a ton of resources to support you on your journey.
Let's dive in. We are gonna spend a lot of time in the luteal phase today. I'm so excited. We're gonna talk about P-M-S-P-M-D-D, what's going on with [00:02:00] progesterone, allopregnanolone, all of the things. But in your new book, you said something interesting and it was a study I hadn't seen before, and that is women during their ovulatory phase select sexier outfits.
In fact, like they actually drew like these ideal outfits and they were definitely sexier. Why do you think that's important for women to know?
I think that it's important to know that, you know, throughout the cycle, your brain is essentially guiding you down two different paths, right? And this is because for a woman to reproduce, there's two different jobs that her body needs to do, right?
She has to pick a mate and um, and find a mate, and attract a mate and have sex with that mate, right? So that's job one. Mm-hmm. And then job two is implantation. So allowing an embryo to implant and then for pregnancy to occur. And so understanding that our body and our brain is. Sort of all gearing up and, and acting in a way that is consistent with each of these two goals, I think is really interesting and important for women to understand because it's like, [00:03:00] it can really help us understand ourselves.
And indeed in that study, what they found is that in, uh, during the, you know, first 14 days of the cycle, we'll just roughly call that, you know, the follicular phase, but especially ramping up toward ovulation. So in that five days or so prior to ovulation, um, that women as estrogen is rising, that they become increasingly, almost exhibitionist.
Mm-hmm. Like women feel sexier. Yeah. You know, they're, they're selecting sexier clothes. And I think that that's really important a just to understand yourself, right. And understand what happens across the cycle, but also in some ways to understand what can happen when your hormones are suppressed. And, you know, of course, you and I have a shared interest in the birth control pill and the research on the birth control pill.
And just to veer really quickly into this. One of the things, and I didn't write about this in my, in my book about the birth control pill, but one of my own experiences that I had when I went off of it was I had that experience of having that increase in estrogen. Mm-hmm. And having that feeling of, you [00:04:00] know, like, wow, like I feel really good in my skin and I just feel sexy and like I wanna be out there in the world.
And I was missing that. And then when I went off the pill, you know, 'cause I was on it for 10 years and when I went off of it, I had that experience of feeling like, hello world. Yeah. You know, and it's like such a wonderful feeling and to feel that good about yourself and to have that kind of body positivity.
Um, and I think that this is something that women really do experience, you know, peri ovulatory and the research suggests that this is the case. And, um, yeah, it really just helps us understand ourselves.
Mm-hmm. We're gonna circle back, we're gonna talk more about the pill today For sure. 'cause I think it's really important in the context of P-M-D-D-P-M-S.
Mm-hmm. We know it's one of the top, uh, prescribed hormones. Uh, you know, across the board, right? Um, you and I actually had dinner last night and I had said to you, do you find it crazy that we are told our entire lives that the birth control pill is safe? But as soon as we get to menopause, we are told that these bioidentical hormones are suddenly dangerous.
Yeah. As [00:05:00] we talked about last night, I mean, there's. So many double standards in the world of women's healthcare. Mm-hmm. And this to me is one of them. And, and I think it's one of the, the key ones, this idea that giving women these synthetic hormones is somehow better for them than giving women who are in perimenopause and menopause, biologically identical hormones is just absolutely ludicrous.
And it's not supported by the data. Mm-hmm. I mean, the data support, the idea that for most women, hormone therapy is safe. Right. And obviously there are exceptions to this, but like by and large, and particularly when we're talking about biologically identical hormones, and you know, like one of my biggest pet peeves, and I'm sure that you've had this as well, are you gonna go to Progestin?
Yes.
I tried
nuts. So crazy about it is like, not only there, the confusion in practitioners where they don't quite understand the difference between these things, um, but the way that it's written about in the literature. Yeah. You'll have a study where they're giving women birth control pills or they're giving them progestin and then they're writing about it as progesterone.
Yeah. And so we [00:06:00] wonder why there's all this confusion in the literature about whether hormone therapy is safe or whether it's not safe. And it's because even the researchers themselves don't always know what they're doing. Mm-hmm. And like what they're describing. And it's really frustrating and I think that it's made a lot of women, um, unnecessarily afraid of hormone therapy.
Yeah. And a lot
of these women are women who would really benefit from it.
Yeah. As we were talking last night, I'm like, we should have recorded our conversation for you guys, but I was telling you about how like, um, going through IVF, this was just a few years ago, I went back on the pill. Within five days, I'm like the worst human ever.
And I'm gaslighting myself being like, this onset of mood symptoms cannot be this quick. It won't be this rapid. And my husband's like, no, you're either crying or you're yelling at us like what is happening? And then fast forward with endometriosis treatment. I was also given a round of progestin and I was.
You know, asking my doctor like, why not progesterone? And he's like, no, I wanna try this because this is what the research supports. Again, I was not a pleasant person, but when I take progesterone, as I was telling you, like I love [00:07:00] life, it's so good. My toddler cannot get on my nerves. Like it's fantastic.
So we see, especially ob gyn. Really we'll fight, like on the internet about how like, no progestin is the same as progesterone and there's no evidence that there's a difference. What does the research actually say? 'cause
they ain't reading it. Uh, no, I mean, that's just so crazy. It just makes my mind, you know, go like, what?
Because I mean particularly, you know, this is true when we look at the brain. Mm-hmm. And so just to like, back up on this, you know, progesterone is this like really beautiful hormone and it's really gotten a bad rap. And I think one of the big reasons it's gotten a bad rap is that people conflate it and, and sort of assume that it's the same as a progestin.
Mm-hmm. But the two things are very different Molecularly. So progestins, the majority of them are synthesized from testosterone. Yeah. Right? And so the, the chemists, the monkey with the, the molecules in a way where it does stimulate progesterone receptors. Right. And [00:08:00] so it will, you know, shut down ovulation in the brain.
So it tells the hypothalamus, like enough progesterone receptors are being stimulated, um, to, uh, to actually shut down ovulation, right? Mm-hmm. And to prevent the, the cascade that leads to ovulation, but it also stimulates a bunch of other stuff because it's a molecular weirdo. I mean, it's a Franken hormone.
It's such a molecular weird, it's, it's a Franken hormone. Yeah. No, it's a, it's a, it's, it's, it's like been pieced together in a lab. Yeah. And so it'll stimulate progesterone receptors and it doesn't even have great binding affinity, meaning that a lot of times it'll stimulate them and then fall off and then it will stimulate other receptors.
And so we know, for example, from research that it will stimulate glucocorticoid receptors, which is what picks up cortisol. Mm-hmm. Right? And so it can lead your body to go in a complete stress overdrive situation. And it can stimulate testosterone receptors, which is why women sometimes will end up with acne and facial hair.
Yeah. Depending on how androgenic their progestin is. And so pro. Skin is, has more in common with testosterone mm-hmm. Than does [00:09:00] progesterone. And most importantly, like to me, you know, everybody assumes that it's like, like a hormone is a hormone is a hormone, but like part of what makes progesterone so magical is what happens when it's broken down in the body.
Mm-hmm. And it's those metabolites that get released when progesterone is, is, um, is metabolized. And one of the things that you had already mentioned is this, is this like really beautiful neurosteroid called Allopregnanolone. And Allopregnanolone is, um, is only released from the breakdown of progesterone.
It is not released from the breakdown of progestin. Mm-hmm. Because they're just molecularly different products. And Allopregnanolone is like a superhero in the world of women's mental health. Yeah. And people don't know this. They don't know that they're missing out on this really beautiful product that our brain benefits so much from.
And the reason our brain benefits so much from Allopregnanolone is that it's. Stimulates GABAergic activity in the brain. And that's a really ugly word. I [00:10:00] hate the word GABAergic. Um, but it's stimulating your GABA receptors in your brain. And, and GABA is the primary, um, inhibitory neurotransmitter that our brain uses to calm itself down.
Mm-hmm. Right. And so for people who aren't familiar with gaba, um, it is what is released in high quantities when you're doing things like meditating, when you're doing yoga, when you put on your PJ pants and sit in front of the fire and you feel that really calm, relaxing feeling. Mm-hmm. And that feeling that you were talking about when you were taking progesterone where you just kind of feel a kumbaya.
Yeah. And that is like things kind of roll off your back. That's allopregnanolone. That is, um, that is your GABA receptors being stimulated. It's calming your brain down. It also produces, um, it increases neuroplasticity. Mm-hmm. It prevents over excitation in neurons in the brain. And so it has a lot of these really protective benefits to the brain and it also helps, um, increase.
Um, sort of, um, our, our brain's ability to adapt to things by increasing neuroplasticity. Mm-hmm. And so it's this [00:11:00] really beautiful hormone that's found to do things like help regulate our moods. Um, it helps to regulate stress. It has all of these really beautiful effects. You don't get that with progestin.
Yeah.
And what happens is, is especially, you know, if women are not ovulating and producing their own progesterone, they're not getting all of these benefits. Mm-hmm. Right? Because they're never getting exposure to actual progesterone. And so they're feeling. Anxious and stressed out and they're not able to regulate their stress response and their mental health is in the toilet and they can't understand why they can't calm down.
It's 'cause they're not getting enough GABAergic activity in their brain. Mm-hmm. Right. And they're not getting the effects of this really beautiful, wonderful hormone. And when you think about the idea of putting perimenopausal women or like, you know, who, who are already anxious and stressed out on, on something that's going to just further stress them out by diminishing any levels of allopregnanolone that they're actually producing from their little minimal amounts of progesterone that their body is producing while they're [00:12:00] still actually having active cycles.
It's all ludicrous. It's a recipe for poor mental health. Mm-hmm. And that's what we're doing.
Yeah. It's interesting because when it comes to perimenopausal women, we do see this increase of anxiety and depression. I mean it is a peak suicide rate, life, life cycle right there. Like, and that is so serious.
And what's interesting is that we've seen the research. It's the loss of progesterone diminishing in early perimenopause, the loss of allopregnanolone that is leading to this HPA dysregulation, and then you put them on something like the birth control pill, which is blunting cortisol response, which is further aggravating that whole, and for people listening, hypothalamic pituitary adrenal axis, that's the HPA axis, your stress system.
And we're wondering why divorce rates are going up. People are like falling out of love with their life. They're leaving their career. They regret being a mom. It's because like we just took a really hard time of, of someone's [00:13:00] life and we just threw gasoline on that. We just said, let's amplify that. I wanna ask you because there is such a habit.
To put a teenage girl on the pill and just say, just take it for the rest of your life. Like until you wanna have kids or until you're through menopause, like, don't worry about it. Do we actually have any long-term data on what happens when you put a teen on the pill and she essentially doesn't get exposed to progesterone across her lifetime?
Yeah, that's a really great question, and unfortunately, like this is one of these questions that science has. Barely answered. Mm-hmm. Um, because of, I've got a whole soapbox I could get on about teenagers and I'm just not going to, again, and I have teenagers, so I'm like particularly sensitive to, um, how vulnerable they are.
Mm-hmm. Because here they are in this process where their brain is, is completely transforming itself Yeah. From a child brain to a grownup brain. And so their brains are so sensitive and we just treat them like little adults. Mm-hmm. Because they look like grownups, but their brains are still [00:14:00] remodeling themselves.
And so there's so much research that's lacking on teenagers and just about everything. And I think that they're a really grossly understudied group. Mm-hmm. And I think that we need to be more careful with them. So with that sort of soap box aside with birth control, you know, again, here's your brain going through this big remodeling project and like the lead architect in that remodeling project.
Sex hormones. Mm-hmm. Right. Sex hormones, puberty, we all know the story. And, uh, they play an important role in guiding appropriate brain development. And very few researchers have thought to ask the question of what happens then when you put women on the pill? These young women whose brains are still developing and are relying on their sex hormones to guide appropriate brain development.
Yeah. And including allopregnanolone and some of these other things that, um, play an important role in things like neuroplasticity and, and just even the, the, the ability of the brain to learn to regulate our hormones, right. So that our brain getting comfortable with communicating with our ovaries. Right.
That takes a long time. Which is why girls periods are [00:15:00] so wonky the first couple of years that they're cycling. 'cause their brain and their ovaries are still learning their, they're figuring each other out. Yeah. And learning how to regulate themselves. And so stopping all of that, um, from the little research that exists does seem to be linked with some long-term effects.
And so there's been research now using both mouse models and looking at longitudinal studies in humans that have found that. If girls or adolescent mice, um, are using hormonal birth control during, um, in, in the way that they usually characterize adolescents is like 12 to 19. Mm-hmm. So if women are on it between the ages of 12 to 19, um, and then they look at their risk of developing different types of, um, mood disorders over the course of their lifetime.
What the research finds in mice is that you get a long-term risk of anxiety like behavior. Yeah. Right. Because we can't ask the mice whether they're sad or anxious, but we see that there's greater anxiety like behavior even after they've gone off of, even after they've stopped administering the birth control pill.
And in humans, what we find is [00:16:00] that girls, adolescent girls who've been on hormonal birth control during that time are at a greater risk of developing major depressive disorder throughout their lifetime. After they discontinue the pill.
Mm-hmm.
Right. And this is serious. I mean, it's like, I don't think that, um, you know, and, and of course I've got teens.
Yeah. And, um, and you know, most people, like when their adolescent is put on the pill, it's not for regulating fertility. Right. It's for things like acne or, you know, having irregular cycles, which again, is so normal for the first couple of years of cycling. Yeah. And just really trying to find ways to help girls cope with that instead of trying to mask it mm-hmm.
Is really the best thing that we can do. But a lot of times girls are put on the pill and then parents aren't told, because a lot of times the doctors aren't familiar with any of this research. Yeah. That, you know, hey, just so you know, like, you know, this form of acne regulation that we're like, we're gonna try to help your teens acne, but oh yeah, this is going to put them on the road for developing major depressive disorder as an adult.
Mm-hmm. I think most parents and most children would [00:17:00] say, no thank you. Like, why don't we try something else? Yeah, like maybe I'll clean up my diet a little bit. But that's not what's happening because this risk isn't being communicated to women. It's not being communicated to girls. It's not being communicated to families.
Yeah. It's so important that you bring this up and I think people automatically, when we have these conversations, they're like, you must be antibi control. You must not wanna anyone to have access to it. And yet what you're advocating for is informed consent. Why is the birth control pill the only medication that gets a free pass where a woman doesn't have to be informed?
A lot of it is because of this, basically treating women at any age like their children and doctor knows best, daddy knows best. Like you. Just take your pill and be thankful that you have access to it, and I think that's really problematic. And it's, you know, I, I wanna say that when I brought up then the on the pill in my book that like, what I observed clinically is that women who developed mood symptoms when they were on the pill didn't come off and the mood symptoms just went away, right?
Like, it didn't, it didn't happen. [00:18:00] And there were so many clinicians were like, that's not true. I've never seen that, and I'm like, well, how many SSRI prescriptions are you doling out? Right? Like, have you stopped to ask yourself about this road of birth control to SSRI? Like we, we see this phenomenon happens,
right?
Yeah. There was a really beautiful study that was done on the entire population of Denmark. Yeah. So we're talking about millions of women. What they find is that the risk of being prescribed in antidepressant goes up significantly after you get a birth control prescription. Mm-hmm. And they find this to be true even after you statistically control for like how many medications they've been prescribed otherwise.
So it's not just that people who get prescriptions written and take prescriptions are more likely to then take more prescriptions. Mm-hmm. Even after you statistically control for that, what we find is that there is a greater risk of being diagnosed with depression. There's greater risk of then having to subsequently go on an antidepressant after you begin hormonal birth control.
And this is especially true for our adolescents. When you look at the risk of developing, um, a depressive, uh, [00:19:00] disorder or mood disorder of any type, including anxiety disorder, um, the, the risk that from taking the pill, um, on teenagers is so much higher. Mm-hmm. It's twice as high as it is for, for an adult.
And so this is a really vulnerable population that we need to look out for. And I think that the su There was a, another really beautiful study done in Denmark that looked at the suicide risk. Yes. And I think that they found that it was something like six times higher in teenagers, um, who are on the pill relative to teenagers who are not on the pill.
And the, the increased risk was greater for adults, but not like that. I mean, the, the teens are a really vulnerable population. Again, it's 'cause their brain is so receptive to sex hormones at that time. Mm-hmm. You know, it's like that is what's leading the charge in the pubertal transition and transitioning their brain from, you know, a child brain to a grownup brain.
And when you think about. How different a child brain is to a grownup brain. I mean, there's so many differences. It's like you're a completely different person. [00:20:00] Yeah. And the idea that you're going to mask and like shut down the sex hormones that through for millions of years has been what has guided our brain development during that time.
Mm-hmm. Is ludicrous. It's nuts
that I believe that Denmark study was the 2016 study. I'll link to it in the show notes. I remember when that came out and how many women felt validated. Mm-hmm. They've been telling their doctor for years, like, I'm getting mood symptoms. And doctors are always like, well, there's no research to support that.
So it's just in your head. It can't be the birth control pill like you are broken. It's not a medication side effect. Right. And why are you trying to villainize the pill? I never understand this, like protecting the pill over protecting the patient, uh, mindset. But that study came out. So many doctors lined up across the internet to say that study was invalid.
It was a poor study. And women, you are still wrong. You're still making things up. And that was a moment that I just sat back and observed and I was like, this is a catalyst moment for the distrust women have for their providers. Now, women have been saying it for [00:21:00] years. Providers said, we need to study. We don't have a study.
There's not good enough research. Study comes out. They're like, no correlation's, not causation. Pass it off. And that was the moment that I think women really started to question their doctors birth control. They started to look at the generations before them, and now we see. Here we are almost a decade later and doctors are still like, oh, it's just influencers.
Villainizing the birth control pill that makes women not wanna use it. It is doctors being dishonest and gaslighting women that have made them not want to use it. And I think that not taking responsibility has landed us in a very serious situation in women's health. So we've been talking a lot about the pill, which is your first book.
Um, but you have your new book and I wanna talk more 'cause you go, um, more into PMDD talking about different aspects of what's going on with the HPA access and something that was interesting that when I was reading your book, so you know, I'm working on a book, so this I actually [00:22:00] wrote in my book, is that research has shown that cortisol hyporeactivity, which is like called blunted cortisol response in early puberty, is predictive of major depressive disorder.
So as I was, as I was reading your book, when I thought is like, we know the pill. May lead to a blunted cortisol response in some women. We also know teens using the pill are the greater risk for mood disorders. So I'd like to get your thoughts on this HPA issue, this cortisol hyporeactivity, and, uh, I was gonna go into like what uh, parents should know for their teens, but I feel like you covered that.
But it was just something that struck me is that I wrote this in my book about how, you know, seeing a disruption in the HP axis and the cortisol response early in puberty. Can co, can put you at risk for major depressive disorder. How does that relate to what the pill can do for your, for cortisol blunting?
Right. So we know, um, from research that, uh, if you go on the pill, and [00:23:00] this is particularly probably true in adolescents, I haven't seen it broken down this way, but generally what we tend to see is that you get a blunted cortisol response to stress as noted. And it's believed that this happens because again, these.
Progestins are Franken hormones. They bind to lots of different types of receptors, including glucocorticoid receptors, which pick up cortisol. And when the body is getting too much cortisol, it will just shut down the HPA axis. It'll say no more stress hormone for you. And the reason for this is that cortisol is a major mobilizer of resources in the body.
And so one of the things, you know, we always tend to think about cortisol and stress, but cortisol just mobilizes, um, glucose and it mobilizes triglycerides and other things to help mobilize energy to our brain and to the rest of our body during times when things are consequential. Right. It's essentially a sign that this, this is meaningful.
Mm-hmm. Like what you're doing right now matters. Right. Whether it's running away from a bear Right. Or whether it's your wedding day. Right. It's saying this matters like pay attention, have all of your, have all boots [00:24:00] on the ground. Um, but that's really metabolically expensive. Yeah. When you have cortisol in the system, it's taking that glucose and triglycerides from doing other things.
Mm-hmm. Right? Because that would be used to do things like fuel, the immune risk. Bonds, right. And create, you know, cell cellular repair and all of the other jobs that our body has to do. And so cortisol is disruptive when it's, when it's, um, released for long periods of time. Yeah. Because it's essentially taking all these resources, having them circulating in the blood for the brain and the muscle tissue, and then our immune system isn't able to do what it's supposed to do.
Our cell, you know, our cell repair isn't able to do what it's supposed to do. And so our body will just say enough. Mm-hmm. You know, because it doesn't want the body to completely fall apart because that is what will happen. The reason that salmon fall apart after swimming upstream is because of cortisol release.
Yeah. Constant cortisol release literally makes the body fall apart, and so the body will just shut it down. If there's like chronic, um, exposure to glucocorticoids, it's like, alright, enough, no more stress for you. And then the, the, the system gets shut [00:25:00] down. And with the pill, when you have this, these progestins that are stimulating these cortisol receptors, it's making the brain and body think that it is in a, you know, a state of trauma.
Mm-hmm. Right? Like chronic exposure to stress. And so the body seems to be shutting it down. And this is consistent with what we tend to find with women on the pill because they have these really high levels of glucocorticoid binding globulins in their bloodstreams that are essentially the liver saying, no more cortisol for you.
Mm-hmm. Right. And this is the reason we get that blunting and that blunting. At first it might sound like, wow, that's great, then you don't experience stress. But of course that's not what happens. Yeah, that would be nice. But it's not the reality. Yeah. Yeah. Not the reality. Because cortisol is how we cope with stress.
Mm-hmm. It's how our body mobilizes resources so that way we can deal with things that are meaningful, again, whether bad or good. And so when you blunt that you're actually blunting your ability to recover from stress, you're blunting your ability to manage stress or blunting your ability to sort of move smoothly, move from situation to situation.
'cause cortisol [00:26:00] is part of how we adapt to our environment. Yeah. And so it minimizes your ability to adapt to the environment. And this of course can cause problems, right? This can cause problems with mood because when you aren't able to cope with your environment, I mean that causes anxiety, which ultimately leads to depression.
Right? It also can create issues with arm. Ability to cope with hormonal changes. Mm-hmm. And so one of the things that I write about in the, in the new book, the Period Brain, is I talk about the, you know, when we look at women who tend to suffer from really bad PMS and PMDD, many of them have a history of trauma or they have a history of, um, having blunted, uh, HPA access response.
Mm-hmm. And what seems to be happening when you look at all of the pieces together, the puzzle seems to be revealing a picture where these women aren't able to cope. They don't have what, what I refer to in the book as resilience. To hormonal changes. Yeah. Because when our hormones are going through rapid periods of change, our body and our [00:27:00] brain are going through rapid periods of change, and there's a lot of adaptation that has to go on.
Um, there has to be adaptation in terms of our hormone receptors, right? So receptors for things like estrogen or progesterone, but also, um, there has to be a lot of, um, plasticity in terms of things like our, our, um, GABA receptors. Because allopregnanolone levels for naturally cycling women mm-hmm. Are rising and falling during the second half of the cycle in ways, given that they stimulate GABA receptors in the brain.
Our brain has to be able to adjust to those things. Cortisol is the master coordinator of adjustment. Right. It's, it's saying mobilize resources to help us deal with this change. Right. We can think of it as a hormone that helps our body cope with change. Mm-hmm. Right? Because that's kind of one of the, the principle elements of stress and, and, and hormonal change is a form of stress.
Right. Because it's something that is an event that our body needs to cope with, and that's generally the way that we define stress. And so when you're lacking what I call like HPA access tone. Mm-hmm. Right? Like when you've got like a really [00:28:00] nice dynamic cortisol response, like when things are stressful, you get big cortisol release and when things are not, it goes back to normal.
Um, when you're lacking that and have that blunted response that we see in women who've experienced trauma or women who've been on hormonal birth control, um, this. Can diminish your ability to navigate smoothly between hormonal transitions and the luteal phase of the cycle that lasts two weeks of the cycle when you have this huge ebb and flow of the sex hormone, progesterone, right.
And the rise and fall of progesterone happens at levels that are 10 times higher than the rise and fall of estrogen. So even though we all see that little menstrual cycle map that shows this like big shift in estrogen in the first half of the cycle, and then this, you know, just slightly larger shift in progesterone, those things aren't drawn to scale.
Mm-hmm. And the y axis that's showing levels of progesterone is actually scaled at 10 times, um, 10 times higher than the estrogen side. And so we have this huge increase and huge [00:29:00] decrease in progesterone during the luteal phase. And you also get a big increase in decrease in estrogen mm-hmm. That many people don't really pay any attention to because they're always focused on the estrogen shift that happens in the first half of the cycle.
Yeah. Right. Prior to ovulation. And that's a lot of adjustment that our brain and the rest of our body is having to do to cope with that rise and fall of, of hormone. And, and again, it, this isn't just with our hormone receptors, it's with our GABA receptors in our brain because they're getting this. Big rise and fall in Allopregnanolone, and if you're not able to adjust to those changes quickly, it's gonna make you feel messed up.
Mm-hmm. Right. And what we tend to see is that a lot of women who experience PMDD, that's exactly what's happening when they've done studies. These are usually done using animal models and just looking at the, their ability of their neurons to um, like sort of increase and decrease GABA receptors as needed and modulate their GABA receptors in response to that rise and fall of Allopregnanolone.
And [00:30:00] it suggests that it's compromised mm-hmm. Right. In these women. And so they're not able to like, sort of gracefully navigate their way through the luteal phase. And the results of that is they feel absolutely terrible. Mm-hmm.
I wanna zoom out a bit, um, because you said like your brain's changing across the menstrual cycle, but something you, well, let me just say, I also appreciated that graph in your book.
'cause I think you had on there like arbitrary units of like how we always present the menstrual cycle and the way. As I we're having this conversation, like we always present it this way so that the patient can wrap their head around it. But I, as you're saying it, I'm like, I do think some clinicians have taken it as fact.
Yeah. Like they're like, fact, this is exactly what it looks like right now. In your book, you said estrogen acts like miracle grow in the brain. So tell us how that plays out in terms of brain function and behavior.
Yeah, so estrogen essentially primes your brain to be its most alert, sensitive self. Mm-hmm.
Right? And the reason for this is like, this is a period [00:31:00] in time when. Sex can lead to pregnancy and there is no better time for your brain to roll out the red carpet in terms of your sensory Yes. Acuity during than during this time because you're essentially choosing who your genes are going to be intermingling with mm-hmm.
In the next generation and future generations beyond that. And so the process of evolution by selection, this process that has shaped our brain and shaped us to be, you know, the way that we are as human beings, has shaped us to be incredibly sensitive to the environment, and particularly cues related to, uh, mate attraction, uh, during this time in our cycle.
And what we tend to see is that women are more alert, they're more energetic, and they get, um, new dendritic spines on their neurons. So their sensory for people who don't know what that is. Yeah, yeah. Can you explain it? Yeah. Yeah. So, so our neurons, if we always think about the brain as being this like lump, right?
Yes. We know. It's just like this lump and it's so like, and, and, and then it nothing does. Nothing changes, right? Yeah. We just think that it's this like lump and it [00:32:00] sort of is what it is. But that couldn't be further from the truth. The, the brain is just like this beautiful, it's a process. Mm-hmm. And it's always shifting based on the environment and the hormonal environment is one of those things that makes it shift.
And as our hormones change, um, you know, as estrogen is rising in the cycle, you get these little spines that pop out of neurons and they're there to be more sensitive to any information that's coming in. Mm-hmm. Right? So the more of those that are out, the more sensitive we are. And when they retract, the less sensitive that we are.
And the reason our brain isn't always rolling out the red carpet is that that's incredibly metabolically expensive to have all of these dtic spines that are like very aware of like even fine tune differences in scent and fine tune differences in appearance. And this is what we find in women when they're in the estrogenic phase of the cycle.
Particularly prior to ovulation, you get like, women are able to tell the difference between really small [00:33:00] differences in, um, things like cues, for example, related to testosterone. Yeah. So we find that when women are in the estrogenic phase of the cycle, they're better, better able to determine and notice what we just noticeable differences between, um, testosterone markers in men's faces.
Mm-hmm. Right. So for a woman in the luteal phase, when estrogen levels are lower and progesterone is high, they'll be like, they all look the same to me. You show that to a woman near peak fertility in the cycle, and she's like, that guy's different than that guy. That guy's different than that guy. And that one's hot and that one's not.
Yeah.
And you get this, these really interesting differences in just being able to detect these fine tuned differences. We also find this with scent. So they've done this looking at what a woman's sense sensory threshold is for picking up fine tuned differences in a metabolite of, uh, testosterone that's picked up in sent.
And women are more sensitive to that as well. And so it's like our brain is just primed for information and it's like, you know, wants to make good mating related choices. And so it's really sensitive to all of these different types of cues. So the brain [00:34:00] is primed for all of these cues because conception is possible.
Mm-hmm. And so estrogen does act like miracle grow in the brain. It just makes it, you know, this really sensitive, um, version of itself where it's very much aware of a lot of these fine tuned differences that are important in partner choice. And it ends up making us more sensitive to the world. And this is also why the seizure threshold, um, uh, becomes lower.
Yeah. Um, during, like right prior to ovulation is because our brain is so sensitive to sensory stimuli that it can become overwhelmed. Mm-hmm. Right? And that of course, um, can produce migraine headaches and it can produce seizures.
Yeah, everything you just pointed out, it's so controversial. Why is it so controversial to say that women are attracted to a certain type of man, especially if they're natural, naturally cycling versus birth control, that they can pick up on these scents?
Because whenever I talk about this, whenever you talk about it, I see people punching back hard, right? And they're like, stop reducing women to this and, and women select mates for we're, we're way more intelligent than that. And I'm [00:35:00] always like, at your core, you are an animal, right? Yeah. You just are an animal that has a language that you understand.
So you think you're unique, but you are an animal.
Right. Yeah, no. Part of that wisdom, 'cause we do have so much wisdom. We have millions of years of inherited wisdom on our shoulders, right? We have a brain that is the result of an uninterrupted chain of successful reproduction for millions of years, knows a soundbite right there.
It's so amazing. Well, it is. Well, I mean, think about this. If even one of your direct ancestors would've failed to be able to attract a mate. Reproduce and have a baby successfully, you would not be here. Mm-hmm. So each one of us is an evolutionary success story, and I think that's incredibly empowering.
We have this brilliant brain that has managed to get genes down from the, you know, generation to generation to generation for millions of years. It's brilliant. And so why do people have a problem with that? You know, I, I think that it's. [00:36:00] There's still this, but you know, and I think part of it is, you know, the field of medicine in particular was created before we understood that the Cartesian mind body split just wasn't true.
Yeah. You know, like where we used to think that the body was, you know, the sack of meat that followed these laws of, of biology and that the brain was a product of the soul and that it, it had its own sets of properties and that the two things shall never meet, but we know better now. Mm-hmm. We know that the brain is a body part.
It is governed by the same rules that govern the rest of the body. And so the idea that our brains are influenced by our hormones, it's just, I mean, it's biology 1 0 1. Mm-hmm. It would be impossible for them not to. Uh, and, and, and it's like the most important body part we have is our brain. And the idea that it would somehow be immune to our hormonal influences is completely cuckoo nuts because our hormones make us better.
They don't make us worse. And I think that there's also this like belief out there that. There's something [00:37:00] wrong with our hormones and that our hormones make us somebody other than who we are when it's like our hormones are who we are. I love that your eye
roll in that statement. I mean, it's like
they're, they're who we are, you know?
And, and in my first book, I have a chapter and I want, I wish I could write the same chapter in every book I write, but it's just you are your hormones. Yeah. You know, they're part of like the, the cr, the like what your brain uses to create the experience of who you are. So who you are is created by all of these gears and sprockets going on inside your brain that are influenced by, you know, neurochemicals and neuromodulators and neurotransmitters and electrical activity and hormones.
And that is this version of yourself that you've created in your head, and that's the version of yourself that creates behavior and makes you who you are in the world. We're so much better for it because our hormones help us adapt. Yeah. You know, we talked about cortisol and it's like when you don't have that, you're not able to adjust your behavior appropriately and
evolutionary speaking, you would've died.
Yeah, you would've died. You would've been like, as I escape the predator. Not ever. No, no, no, no. Yeah,
no. You'd just be chilling with your. [00:38:00] Friends, you know, when the saber tooth tiger's coming or you'd be chilling with your friends when there's a potential romantic partner that's high quality. 'cause another uh, domain in which cortisol just gets absolutely flooded in the body is attraction.
Mm-hmm. You know, so it's like we, you know, stress is, is, is a lot of different things. Right. It's just your body saying this is important. Right. This hasn't, this has consequences for your ability to survive or your ability to reproduce. Yeah. Pay attention, mobilize all the resources. Right. Pull up some of that energy that you're using to divide cells and, and deal with the, and deal with the immunological challenges.
Mm-hmm. And let's direct that to the brain right now because it needs to do whatever it needs, you know, to attract that mate or to get away from that saber-tooth tiger.
Yeah, and I think, you know what came up when we were talking at dinner last night and I had said to you like, I think that the women who came before us.
And we definitely see it's that boomer generation of gynecologists who I know. I'm like, is boomer a bad word? I don't know. But it's the generation that it is. I don't know, you guys can tell me in the comments, I don't mean that with disrespect, but is that generation of [00:39:00] gynecologists who were like, just suppress your hormones with birth control.
There's no reason that you need them. You can be just like a man and work just like a man. If you do that, don't ever acknowledge that our hormones make us different, make us act different, make us think different, make us do anything different. Like that is just, you know, crazy talk. And I get that they did that because they were like, we feel like we have to.
Tell men we're the same as them to be able to advance our careers. But I absolutely think they did tremendous harm in women's health. And I don't say that as like people, you know, in general, I'm talking about practitioners. Mm-hmm. Who were telling women that your hormones are something to be suppressed mm-hmm.
Ignored. Mm-hmm. And never acknowledged. Mm-hmm. Because they'll find a way to weaponize it and say, we're weaker, which. I have always said, your hormones give you superpowers. And I believe very much in everything you're just saying. It really demonstrates that they absolutely do give us superpowers. And the dynamic change across the cycle is something that when you understand, you can [00:40:00] absolutely leverage.
I wanna go into that, 'cause I feel like you've talked about like the changes with estrogen. What's going on in the follicular phase? We've kind of alluded to like, you know, the allopregnanolone, the GABA receptors, but can we just go across the menstrual cycle and kind of put it together for women, what's happening with their brain?
Right. Let's just talk about why we have two hormones instead of one. Mm-hmm. Right. And And as you noted, I mean, for a long time it was assumed that there must be something wrong. Yeah. With having two hormones instead of one because men have one there, right? They have one primary sex hormone. They have
like a very basic operating mode.
Right. Altogether. Right. And I don't mean that with disrespect people. I'm raising two boys, but like. They don't have to do anything fancy. Right. Right. 'cause they just have to ejaculate. Yeah. But we actually have to gest state, like Right. There's so much more going on.
Yeah. No, it's like our bodies have two jobs to do for reproduction.
Right. There's made attraction and sex and then there's implantation and pregnancy. Mm-hmm. And so it's like our, we have two hormones because our bodies and our brains have two different [00:41:00] jobs to do in order to pass down genes. Men have one. And the only reason that we think that that's better and superior is because men were studied first.
Yep. So all of our default assumptions about what it means to be a human and like a functioning human is based on a male typology. Mm-hmm. And that just doesn't work for women. And as you noted, it's like for a very long time, um, it was assumed that, yeah, there was something wrong with our way of being.
That's simply not true. And, you know, we could turn that argument on its head. And, you know, just to give you an example, you know, there's this idea that, oh, well women are fickle. Mm-hmm. Right? Because our hormones change and therefore, like, who are we? We could turn that on its head and say, men are overly simplistic.
Mm-hmm. You know, like if you can't look at things through two different lenses, then you're completely inefficient. You know, you're, you're, you're inept. But we've embodied Yeah. This idea of inferiority. And I think that that's what's guided this decision making where it's like, we need to suppress the discussion of [00:42:00] hormones and like, why they're important.
Because women have embodied this idea of inferiority that's simply not true. Hmm. You know, it's like our hormones are part of our wisdom, they're part of our bodily wisdom. When we tell women they don't matter, it makes them feel pathological.
Yes.
Right. And so part of this, my book is, you know, even though I think we've gotten more comfortable societally.
With the idea that women cycle, right? Everything is focused on estrogen. Right? And this is true, um, in popular discussion. So when we talk about like, oh, you know, hormones matter and you know, estrogen does this and estrogen does that, and estrogen does this. Um, and this is also true in research because, um, because men were studied first, um, the way that researchers decided to deal with women's hormonal cyclicity in research was to try to study women only when they're most like men.
Yeah. And so, I know, right? I just have to laugh when you say that. 'cause it's like, oh, thanks for including us in drug studies, but also not really including right. In our entirety.
[00:43:00] No. Yeah. So it, so one thing that, um, people aren't usually aware of is that in most biomedical research, women are only included as research participants during the first nine days of their menstrual cycle.
Mm-hmm. Right? And the idea is that they're trying to keep, they're trying to study women only when their hormone levels are maximally low, to make them maximally similar to men. The problem with this is, of course, is that women are not in that. Hormonal state most of the cycle.
Yeah.
Right. They never study us when hormones are high.
And so we have this whole other set of assumptions that our body is following when it's under progesterone that are never, ever studied. Right. So it's like we're we're studied. Um, they, they now include women in research, but they don't study us as women. Right. Because women are cyclical. Yeah. And so we have these two, we have these two primary sex hormones.
Estrogen, again, gets all of our gears working together for attraction and, um, and sex. And then progesterone gets all the gears working together for implantation and [00:44:00] pregnancy. And this doesn't sound like that big of a deal. Like, oh, okay, well, whatever. I don't care what that has to do with anything. Um, it has a lot to do with everything.
Mm-hmm. And the reason for this is that for pregnancy to occur. The female body has to absolutely change the rules of engagement for almost every system in the body. What our brain does has to differ, right? We have to become, for example, less interested in sensation seeking and wasting energy, going out and chasing opportunities because our energy levels are gonna be lower when we're pregnant, right?
So it actually dampens. Our, um, reward sensitivity to rewards in the environment. Right? It also lowers our threshold for when we see something as threatening, because women, when they're pregnant are in a more vulnerable state. They're not able to get away as quickly. And so we become more sensitive to threats, both social threats and physical threats.
Our immune system has to change what it's doing because our very inflammatory immune system that we have during the first half of the [00:45:00] cycle, and not inflammatory in a bad way, but just a very reactive immune system, estrogen is, is it helps to prime the immune system in a lot of ways. Mm-hmm. Um, and.
Progesterone has to tamp down the brakes on that because if you have a super active immune system and you have an embryo that's trying to implant, it looks a lot like a pathogen because it has genetic material that doesn't belong to self. And that's what the immune system will go after if it's in its heightened state.
And so it shifts our immune system from a, a, what, what we call a th one response to a th two type anti-inflammatory response. Our circulatory system has to change what it's doing because all of a sudden it has to have a lot more blood flow going to the uterine area. And this is something that happens in pregnancy, but also in pre-pregnancy.
In the luteal phase, our body temperature increases, which means that our, uh, basal metabolic rate has to increase. And so we see that women's calorie needs increase by about seven to 10% in the luteal phase of the cycle. Mm-hmm. Um, our respiration rate [00:46:00] and our heart rate increases, our respiratory drive increases, meaning that we feel the need to get breath more, so women feel more, um, out of breath when they're working out heavily during the second half of the cycle.
Our ability to build muscle mass decreases because our body is taking those energetic resources and is directing them toward building an endometrial layer. Mm-hmm. Everything. Changes. Yeah. Right. And so the idea that we can take rules that were created from science conducted on men and apply that to women doesn't work.
The idea that we can take research that was conducted on women in the early stages of the menstrual cycle when estrogen is the primary hormone, and then apply that to progesterone, that also doesn't work. Mm-hmm. Right? And so a lot of what we know about ourselves. Is, is completely guided from what is sort of normal for a woman during the estrogenic phase of the cycle.
And it doesn't necessarily apply to the luteal phase. And so I talk about this book and talk about this idea that, you know, when we think about [00:47:00] estrogen, everybody's like, oh yeah, you know, it, it does sort of make me wanna have sex more. And you know, and I feel sexier and it's doing all these things that promote sex, sex, sex.
And then there's the luteal phase, and that's just. PMs, I just feel terrible. And it's like, well no. Like this is actually, there's a lot of wisdom in these psychological and physical shifts that are going on. Mm-hmm. It's just that one, they've been made to feel pathological because we've been given a one size fits all version of what it means to be human.
That does not fit for a female. It just doesn't fit. If you're a cycling female that doesn't fit, you have two sizes. Right. There's at least two right versions of what your body needs and what it does. Mm-hmm. And when we're not told about that, it feels pathological. And the other part is that our body actually creates pathology.
'cause we're following guidance that was never created for the cycle phase. Yeah. You know, so for example, you know, one of the things I talk about in my book is this idea that. You know, all of us are told from nutritionists, here's the number of calories that you need to have on [00:48:00] a given day. Right? And here's how you need, you know, from your trainer, here's how you need to work out every day of the cycle.
And that might work well and good during the first half of the cycle. But then when you shift into the luteal phase and your calorie needs go up by seven to 10%, you know, if you're somebody who usually eats about 2000 calories a day, that's between like a, an additional 140 and 200 calories a day. Mm-hmm.
Women already told this. Yeah. Right. And instead they're like, God, you know, I'm so hungry. And then we start to tell ourselves a story, right? About how we have no self-control. What's wrong with me? Right? And then because you're hungry and your body, which thinks it's gearing up for a pregnancy, is gonna see this as an emergency, right?
So your hunger hormones are gonna be telling your brain emergency. And so then your brain is going to be like, oh my gosh. Like I, you know, and then you start having food cravings and the next thing you know, right? You're in the pantry eating peanut butter outta the jar. And then you're like, what did, like, why did I do that?
You know? Like, why did I do that? And it's because we didn't do what our body needed. Yeah. We didn't listen [00:49:00] to it. And as women, you know, and, and you, you talked about this early on in the inter interview, and I really appreciated this. Um, and especially from somebody who's been in the clinical world, it's like.
Our doctors have taught us to distrust our bodies. Yes. From, from the time we're small, you know, and, and this, there's no better example of, of what happens in the luteal phase, you know? And, and we experience these shifts, right? We're feeling hungrier and we're telling ourselves a story like I am, have no self-control.
I just suck. You know, I have, I'm never gonna, you know, I have no willpower. We tell ourselves these terrible stories about ourselves. Mm-hmm. We think that our body is the enemy when it's guiding us toward the things that we're actually supposed to be doing to take care of our bodies. But because that flies in the face of the bad advice that we've been given, we learn to distrust ourselves instead of distrusting our doctor or distrusting the nutritional advice that we've been given.
Mm-hmm. And it's time that we start really taking these things seriously because even though I [00:50:00] recognize that for a very long time, women were. Treated as inferior versions of men, just because we cycle, it's time that we totally shift that narrative and we embrace the fact that we cycle. Because when we don't do that, we go through these, you know, entire two weeks of our lives, um, every single month where we feel completely outta control and pathological.
Yeah. And like it's time that we really take that seriously. It's time that we understand it and then learn about ourselves during this phase in the cycle, which is what I'm trying to do with my book. The Period Brain is really educate women about what is your body actually doing during this time and what do we need to take care of it during this time?
But then we also need to use this to change science for the better because currently the gold standard in clinical research. In biomedical research is to only study women in the first nine days of their cycle. Mm-hmm. That's the gold standard. That's considered a really well done study, and that makes absolutely no sense whatsoever.
And this is why a lot of women experience premenstrual [00:51:00] worsening or premenstrual. And I say this because a lot of times when women experience premenstrual worsening of symptoms, it's during the last full two weeks of the cycle. Yeah. And we see premenstrual worsening of things like asthma, A DHD, which of course we talked a lot about.
Um, we talked a lot about yesterday. Um, you see premenstrual worsening of, um, eating disorders. You see premenstrual worsening of personality disorders. Of mood disorders. Mm-hmm. I mean, the list goes on and on and on and on. And women report that the drugs don't work as well during certain phases of the cycle compared to other, I mean, and, and.
That's just scratching the surface, you know, it's really, we need to be studying women under control of both of their primary sex hormones, not leaving progesterone in the ghetto, and as a result, leaving women in the health ghetto during this phase of the cycle.
Mm-hmm. This is so well said, and it's, as you're saying this, I'm like, you know, part of why you and I are considered so controversial in our work is because we're challenging an entire paradigm that has told women that they're inferior, but not just told them.
That [00:52:00] actually profited off of that, actually been able to, you know, basically put us in the corner so that other things can be advanced at our expense. As you were saying, these things that get worse before your period. I was actually surprised when I read in your book where you said that studies show that almost 70% hard explanation point right there of women with major depressive disorder and bipolar disorder experience exacerbation the premenstrually.
So for people listening, everything's getting worse. Leading up to your period, and you know, in the case of PMDD, and we're gonna define PMDD and PMS in a second. When you consider that this is two weeks out of every month, that is half the year, in what world would we ever tell a man? It is okay for you to be debilitated and feel awful for six months out of the year and yet.
It is something that has been perpetuated in women, and I'm not saying this as if men [00:53:00] had it out for us in saying this, it is that medicine didn't care about us enough to study this. So wanna talk, I wanna shift gears to talking about PMDD. Let's define PMS versus PMDD. 'cause you talk a lot about this in your new book.
Mm-hmm. Mm-hmm.
Yeah. So the difference between PMS and PMDD. So PMS, it describes almost everything that women experience in the luteal phase. Mm-hmm. You know, from really minor disturbances in just feeling more tired and sluggish, which is allopregnanolone actually stimulating your GABA receptors and making you try to conserve energy.
Um, because the luteal phase is so metabolically expensive because of all that new cell creation in the endometrial area. Not
to mention
immune
risky. Yes. You wanna, you wanna stay home more? Yeah.
No, exactly. Yes, yes. No. Yes. Brilliant. Yes. And so, um, PMS has been used to describe again, you know, just even minor, um, experiences that we have during the, the second half of the cycle to a whole, you know, host of combination of things where you're feeling a little bit sad and you, you've got, you [00:54:00] know, food cravings and you've got, um, whatever.
Um, but PMDD is, is more serious. It's generally like one of the defining characteristics of PMDD that separates it from, uh, from just run of the mill PMS is, um, is suicidal ideation. Mm-hmm. Um, so, and it's, it's funny because it is a real land, it's, it's a landmine for doctors to screen for PMDD because as soon as you ask somebody about p uh, about, um, suicidal ideation, there's a whole protocol that you have to follow.
Yeah. That could lead to institutionalization of their patients. And most doctors don't want to do that, um, for a good reason because the women don't want to do that. Yeah. Yeah. And so it's like, it's really, it can be a little bit tricky to navigate, but it's also, um, characterized by really debilitating, um, mood related symptoms.
Um, the sort of crown and jewel, um, symptomology of PMDD is, is are these really severe, debilitating mood related symptoms oftentimes, um, accompanied by suicidal ideation. And, um, you know, it's funny, so in my book, I, I list what the [00:55:00] criteria are for being diagnosed with PMDD. I don't actually publish 'cause there's a, uh, the DSM, the DSM guides, which, um, is a diagnostic statistical manual, which is what the a PA uses to define different categories of psychological illness.
Um, I can't, I can't publish exact questionnaire, but all of the items are in there. Yeah. They're in a table about what you need to be paying attention to and how clinicians are able to actually distinguish whether you fall into the category of PMDD or not. And, um, but it, it is really debil these debilitating mood related symptoms.
Mm-hmm. Um, and for women who have PMDD, I mean, this is like endometriosis, which was something we spent a lot of time, um, talking about last night at our really wonderful dinner with experts. And when you
hang out with endometriosis surgeons Yeah. Is what talked about. Yeah. It
was so, like there was scans being cast around the table.
It was just,
I was saying that I was like, at some point, always in our dinner, here comes the imaging and we started talking about cases and stuff.
So Fun. No, it was just, it was just so fun. So, um, but it, it usually takes women a [00:56:00] very long time to get A-P-M-D-D diagnosis. And so this is something that, um, I always recommend that women start tracking their symptomology early.
Yeah. Because if they can go to their doctor with evidence, um, and that's, this is what your doctor's going to ask for is like at least two months of evidence. Mm-hmm. Showing that your mood changes that you're getting that are so debilitating are. Specific to the luteal phase. Um, and this is something that is incredibly debilitating to women.
Yeah. I mean, it's incredibly debilitating. I mean, some women don't, aren't able to get outta bed. They lash out at people they love, and then they've got this brain because during the luteal phase, it's really primed for, um, social sensitivity to threats. And so they're lashing out at people and then they're really sensitive to the feedback they're getting.
And I mean, it just creates these loops that are really terrible for women. It's a really heartbreaking diagnosis to get, because as you noted, this is a woman feeling on the brink 50% of the time. Mm-hmm. It's a really terrible, it's a really terrible condition.
We're gonna talk about treatments. Uh, I don't wanna jump there yet, but, [00:57:00] uh, so I didn't know I had PMDD as a teenager and now I, I didn't know I had PMDD and I didn't know I had endometriosis and my doctors could care less.
Because they were like, take the pill. But I remember, um, being on the pill and being so debilitated that I would get in the shower and I would just cry and be on the floor of the shower, physically unable to get out. And I look back at that and I just remember thinking like, why, like, what's wrong with me?
People telling me like, you just need to, you know, you need to try harder. You need to suck it up. Um, and it is something that, you know, I wor have worked a lot. It's the work that I do that I've been able to resolve my PMDD symptoms. But I shared with my audience that, so following my miscarriage and my cycle came back and it was, I felt it like I could almost, I'm like getting kind of teary.
'cause because I was, I remember I was just sitting there and I'm like, it feels like I can see how good my life is, but there is a glass panel between me and my life and I cannot touch it. And I'm stuck here in this horrible dark side. And I was like. [00:58:00] Hell no. We are not going back there. And I think that for women listening, like the minute you start to have feelings like that, it is absolutely time to take action.
Mm-hmm. So we're gonna talk more about taking action today, but one of the things we have to start talking about, like what are the causes of PMDD? Big floating question mark above my head right now. Right. Because, um, we just don't study the female body the way that we should, but we brought up Allopregnanolone.
Allopregnanolone for some of us is like the best thing we ever met. And we like, feel so in love with our life and we sleep well. But for others of us. It is not. Can you talk about that and, and what is going on with the GABA receptors in the brain that may, that may be potentially one of the contributing factors to PMDD?
Right. Yeah. So as noted, PMDD is very poorly understood, and in the book I talk about, there's some research into looking at, um, inflammatory processes and whether or not that might be a contributing factor. Um, looking at, um, [00:59:00] dysregulation in your, in vagal tone, so your vagus nerve and its ability to be able to communicate effectively with brain.
There's research looking at the HPA axis again, and whether or not that is at, at play, it's probably a combination of all of these things. Um, and one of the other issues that researchers have really been looking at is this issue with allopregnanolone as noted. And, um, what seems to be happening is so allopregnanolone like, like.
You know, if I had to like place a bet on what it's going to do, like let's say I'm studying a mouse model or I'm, you know, studying a, a healthy human, um, if I had to place a bet on what it's gonna do in the brain and, and then like the subjective responses we're gonna have to, it, it would be that it's gonna make you feel good.
Yeah. Because for most people it is very calming and it's very kumbaya and, um, and it is related to this calming neuro transmission. Um, but for some people, um, for some women and including some women who have PMDD, what you find is that you have this dysfunctional relationship with Allopregnanolone.
Mm-hmm. And it seems to be. [01:00:00] Again, this has to do with the, the gabaa receptors in the brain, not remodeling themselves appropriately, um, in response to changing levels of GA or changing levels of AOE or allol alone. And what, what happens during the luteal phase, if we want to just like kind of zoom out a little bit, is you get this really intense rise to progesterone.
Mm-hmm. And then you get an intense fall of progesterone if you're not pregnant. And this requires your brain and your GABA receptors, which are receiving, you know, stimulation from this really beautiful, um, allopregnanolone allopregnanolone. Operates, and it rises and falls almost in lock step with progesterone levels.
And so when progesterone is rising, your brain is getting all this beautiful activity. And then when progesterone levels start to fall, if your brain is able to adjust to that, it's not really, you can feel a little more sad. Mm-hmm. Um, but it's not very noticeable because your brain is able to ride the wave.
You know, it's sort of like coasting up and down a hill. [01:01:00] Um, but if your brain isn't able to adjust. Quickly to the amount of stimulation it's getting on the GABA receptors because of dysfunction in the, in the GABA receptors, which we can talk about. Um, this can lead to, um, it feeling like they're falling off a cliff.
Yeah. Right. So instead of coasting up and down a hill, they're climbing a mountain and then falling off a cliff because all of a sudden they're, you know, they have all of these naked GABA receptors, you know, so imagine that you're a receptor in the brain whose job it is to pull in chemicals that are soothing the brain.
Right. And all of a sudden you're naked. Mm-hmm. Right? And you're like, oh, where's, you know, where's all that soothing stuff? Like, I need that. Like, what am I gonna do? And the, the brain feels really alarmed and it feels really terrible. And so that is one of the, the factors, um, that seems to be related to some women not responding well to Allopregnanolone, is that they get withdrawal syndrome or symptoms when it goes away.
Other women, and this one's, this one's really interesting 'cause it, it again gets at how idiosyncratic each one of us are. Which is why one of the things I talk about in the book is like, you absolutely need to be tracking your [01:02:00] cycle. Mm-hmm. And you need to be tracking, like, I have a list of symptoms or exp and I, and I hate the word symptoms 'cause they're not symptoms or experiences.
Experiences. I
like that. Yeah. You need to be tracking your experiences over the cycle to understand your own personal relationship to your hormones. 'cause all of us respond differently. Like the, like, and just as a caveat and then we'll jump back on there. Or or a side note. There are some women who feel terrible near ovulation.
Mm-hmm. Like there's a small handful. It's about 7% of the population who reliably feel terrible at that time, which is. Like crazy for those of us who feel so wonderful during that time. Yeah. But, um, you know, for, with Allopregnanolone, some women metabolize it too fast. Mm-hmm. And so these women are like super metabolizers.
And what happens is, uh, progesterone is being broken down in the body and then Allopregnanolone is being released and their body's like. Like pulling it all away because it's really quick at breaking it down and then it's not getting that, again, that really soothing activity in the brain because their bodies are super metabolizers of, of the stuff.
Mm-hmm. And so, um, there's all kinds of things that can go wrong in [01:03:00] this side of the cycle just because it is characterized by such huge inconsequential hormonal changes that when things aren't working exactly as they should, it can lead women to feel pretty awful, including things like, um, developing, uh, PMDD.
So with what you're talking about with progesterone, so we'll see this call progesterone sensitivity. There's also, uh, we know that sometimes when we dose women with oral micronized progesterone, this progesterone intolerance, so they feel they might feel really groggy the next day and kind of bluesy.
And so we have to like titrate the dose down. But other times they, they don't get that, like, I feel really chilled out and calm. They get. I feel really anxious and amped up and like there's a problem going on in my body. And so there's a lot of focus on just getting the progesterone levels right? Mm-hmm.
We even see that, um, there was a newer study that came out with a progesterone modulating drug, and it's like the key is keep progesterone low, just keep it low and steady the whole time. But you [01:04:00] talk about in your book like, we need to not just focus on hormone levels, but the actual individual sensitivity to them.
Mm-hmm. Can you talk more about that?
Yeah. So when we look at differences in hormone levels between people who have like. PMS, severe P-M-S-P-M-D-D, and then people who really don't even notice the luteal phase very much. Mm-hmm. Um, they, they, their hormone levels are indistinguishable from one another.
Right. And so in the research world, um, we've long abandoned the idea of looking at hormonal, you know, imbalances or whatever as, as the key to understanding, um, different types of symptomology that we get. Mm-hmm. I mean, instead, most of the research focus is on what you've noted, um, hormonal sensitivity.
And that is, um, you know, how sensitive are you to hormonal changes. Mm-hmm. And so, you know, with PMDD, for example, one of the leading hypotheses about sort of mechanistically what's going on there is that, um, is that women are just super sensitive to hormonal changes. And again, for one of these different reasons that we talked about, whether it's that they aren't able to [01:05:00] adjust their gabaa receptors, um, quickly enough to be able to adjust to changing levels of allopregnanolone, whether they're allopregnanolone, super metabolizers and they're start breaking it down faster than, um, than it can be sort of received by the body leading to this.
Perceived shortage. Um, any dysregulation in the HPA access that's like just decreasing your ability to navigate stressors of all sorts? Um, they, I mean, it's all over the map. Mm-hmm. But, um, so the actual cause of the sensitivity, um, is, can be variable. But one thing that we do know is that yes, it is the sensitivity that seems to be causing the symptoms.
This is one of the reasons that, um, doctors will give women, um, for example, uh, birth control pills. Um, because, and, and they'll usually give them the ones that go for three months without, uh, a withdrawal bleed. Mm-hmm. Um, because going for that three months of having every day be the same day, hormonally, um, for some women can be very palliative because they are sensitive to hormonal changes and keeping things constant makes them feel better, even if that constant may, may not be as good as they would feel if [01:06:00] they were naturally cycling.
Um, and this is also why, interestingly enough, um, why it is that, um, antidepressants dosed only in the luteal phase also seem to be, um, palliative to women who are, who have PMDD. Um, and, and, and what this research finds is, you know, for people who take, uh, antidepressants for, um, uh, depression or anxiety, you have to take them for several months.
Before they actually start working and making 'em feel better. Um, and the reason for this is that the primary mechanism, by, by which they're believed or hypothesized to work, researchers still don't actually know how they work, by the way, in case you didn't know that. Um, but the leading hypothesis is that they increase neuroplasticity in the brain.
Mm-hmm. And, um, by having all of that serotonin and the synaptic cleft, which, um, is what you get when you take an SSRI, um, that this, um, causes the brain to have to sort of. Change how it's doing things in ways that increase neuroplasticity that may lead to mood stabilizing benefits. Um, with women who have PMDD, [01:07:00] um, they're able to just take, uh, antidepressants or SSRIs, um, during the luteal phase.
Yeah. Which, um, and, and it works. Um, and so there's a lot of women who find, um, support this way and it works by actually increasing, um. But it, it, it sort of smooths out the way that the body deals with gaba. Mm-hmm. Which is, which is, or, or, or deals with allopregnanolone in ways that, that, um, keep, uh, levels of allopregnanolone more constant than what you see in women who aren't using them.
Which is also, I think really, um, really interesting. And it also offers, um, you know, I'm not a big proponent of, um, I'm not somebody who loves prescription drugs, but I do love when they can help people. Um, and for women who have PMDD, there's a lot of them looking for help however they can get it. Um, and for some of them, uh, hormonal birth control can be palliative for others.
Um, taking intermittent dosing of SSRIs can be very palliative. And I like that option for women, um, better than just taking SSRIs all the time because of course it does allow them control. Mm-hmm. And I think that that's a lot of the [01:08:00] things that, that women really struggle with, with SSRIs. 'cause they have terrible side effects.
You know, and, um, yeah, and, and the idea that they can just take them when they need to, um, makes women, um, more, at least willing to try it if that's what they want to go, or that's the way they want to go. There's also non hor, you know, non-medical things that I think are always, I always think it's better to try those things first.
Mm-hmm. Um, just because the side effects of the non-medical interventions tend to be so positive. So, you know, some of the ways that research supports. Um, treating PMDD and helping women really feel better, um, even when they have pretty tough cases of PMDD. Um, cognitive behavioral therapy and neurofeedback therapy is found to be incredibly supportive to women, um, who have these types of symptoms.
And essentially what these types of therapies too, is they work with women to be able to recognize the trains of thought that they get into when they're having these episodes. 'cause a lot of times they do tend to be, um, characterized by [01:09:00] periods of rumination. Mm-hmm. Um, and teaching women to recognize when they're in one of those periods and then how to talk themselves out of it.
Um, neuro using neurofeedback, you're able to actually see the brainwaves that are happening when you're in that terrible state. And you have to learn by watching your brainwaves and just. Trying all sorts of different mental gymnastics until you're able to see it calm down, you learn what makes your brain calm down.
Mm-hmm. So why I love neurofeedback, because it's different for everybody. What, what those, um, sorts of thoughts are gonna be and then really working to, um, get in the habit of shifting into that mindset when you're starting to recognize symptoms. And those things can be very useful to women. Mm-hmm. Um, there's also some really great research, we're starting a project right now looking at, um, stimulating your, your vagus nerve and that as something that is a, um.
A non-medication based treatment. Um, because one of the things that we know is that many women who have PMDD, they do have low vagal tone. Mm-hmm. [01:10:00] So the, the communication between their periphery, so their body outside of their brain and their brain doesn't seem to be very, um, adept. Um, they don't have a good communication pathway.
Their brain and body doesn't like to communicate well. And, uh, doing vagus nerve stimulation is a way to get your body to learn and get better at, at having these kinds of connections. And it seems to be really helpful, um, with major depressive disorder. Mm-hmm. There's even some new research showing it's helpful with endometriosis.
Yeah. Which is fascinating. I
am a.
Big fan
vagal nerve stimulation. Yeah. So cool. Yeah. And we have a whole episode that we did on it, um, with a, a doctor, uh, Dr. Neva, he's a friend of mine, and that's like all he talks about, but be before we got more research on it. But with patients, like I would, and this is gonna sound bad, but I would even have patients gag themselves with a toothbrush to real, because it will stimulate that.
Yeah. Like first thing in the morning and people would say like, my day is actually better. And it sounds really awful to do, like humming singing. [01:11:00] Right. You know, there's different breathing patterns. Like there's other things you can do, but if you really wanna stimulate it, we put a toothbrush back there and it really sounds, it sounds so terrible.
It sounds so terrible. But, um, I, I picked that up actually from. Doctors who were doing a lot of work with an neurodegenerative disease, and that's something that they had patients do because they're like, when you stimulate in that way, there's an influx of like oxygen. It helps like get they're stimulating, like we need more mitochondria here.
Mm-hmm. Like it sends this really powerful signal. It's very interesting. So everything that you just talked about. PMDD we see from reports that women who are autistic, roughly 90% of them report PMDD and almost half of those with a DH ADHD report, PMD. Mm-hmm. And there's things that you brought up that I wanna connect for this community.
So one, talking about the neuroplasticity and SSRIs, we know that those with a DHD specifically, I'd have to look at the research for autism. Uh, lower levels of B bdnf [01:12:00] mm-hmm. Alpha. Mm-hmm. So brain derived neurotrophic factors. Mm-hmm. So neuroplasticity can be an issue, uh, actually generating energy in the brain.
Mm-hmm. Um, you talked about how HP dysregulation and cortisol is just very metabolically expensive, uh, event going on, how having so much estrogen priming your brain is very expensive going on. What I like to say that like basically, you know, people with a DHD, they are, they're burning like through rocket fuel, like Yeah.
To run through their day because they are metabolically using so much energy. And what's interesting is you talk about like, we can't be sensitive all the time. That's what, why we gotta dial back on the luteal phase. But we know that, you know, part of the issue with autism, and we can even see with a DH ADHD brains is that there wasn't actually pruning in their brain.
Like we, they should have went through developmentally. Mm-hmm. So they are more sensitive. Mm-hmm. They're taking in so much more of the environment. Mm-hmm. Um, they tend to have different metabolic pathways. They tend to have more inflammatory issues, [01:13:00] more, um, immune system dysregulation. So I, I just wanted to like highlight all of that for people because it's something that I talk about in this community a lot of like, why do you struggle with PMDD so much more?
Mm-hmm. And it is something that I see time and again. When we have issues with progesterone sensitivity, so often they're somewhere falling into the under in that neurodivergent umbrella. Mm-hmm. And the question is, is that, was this your brain's operating system that has made you so sensitive? Or was your brain's operating system put you at risk for trauma in your life?
Mm-hmm. And experiencing that because you have a different brain trying to fit into a neurotypical world. Mm-hmm. You're often told things like, you're lazy, you're dumb. What's wrong with you? Why are you weird? Like, and you're treated differently. And so it's a big, like, we don't know at this point. Mm-hmm.
Mm-hmm. And as you said, it's likely the kitchen sink. Right? It's like Right. Everything is everything contributing. Yeah. But I do wanna talk about that piece of trauma. 'cause you brought it up earlier. Mm-hmm. And I think it's [01:14:00] a good thing to, to bring up, because you noted in your book. The connection between trauma, uh, adverse childhood experiences or ACE scores and the risk of PMDD.
So can you talk about that?
Yeah, no, there's definitely a, a link. They've done studies where they look at the risk of developing PMDD based on whether you have a trauma background or you do not have a trauma background. Mm-hmm. So looking at ACEs scores in particular, and what you find is that women who've been through traumatic events do have a greater risk of developing PMDD, and it's pretty significant.
Mm-hmm. And, um, and again, i, I, I think that this linkage has to do with, um, dysregulation of the HPA axis and also dysregulation of, um, the ability to regulate inflammation. Because one of the things that we know about dysregulation in the HPA axis is that it also tends to be related to heightened inflammatory activity in the body.
Mm-hmm. Um, and an exaggerated inflammatory response to stress. And so one thing that, um. People don't really recognize about, um, their stress response is that it really is tightly tied to our immune response. And the [01:15:00] two things work together in concert. And, um, and you do get exaggerated inflammatory activity in response to stress, um, when you have blunted cortisol.
And, um, I think all of these things and, and you know, like in terms of, like you said, it's a big mess of spaghetti and it's likely all of these, that's a good analogy. You know, it's like, and, and everything is bi-directional, right? And so we know, for example, that is it that you have a brain that's made this way and then you're more, you know, susceptible to trauma and then the trauma then it like works in a sort of a, a, a.
Forward facing feedback loop where it's just, you know, reinforcing, um, difficult patterns in the brain. We don't know. You know, it's, it's, it's a, it's messy to study and, and as you we know, women's health is in the ghetto and it's just not, you know, whenever you look at research in women's health, it's about everything below the belt and almost nothing at looking at the actual women.
You noted the bikini
medicine in your book, and I appreciate that. Could you tell people what that is, what you mean by that?
Yeah, so bikini medicine is just this idea that the only thing that's different between men and women is the covers [01:16:00] of the, or the parts of the body that can get covered with a bikini.
Mm-hmm.
Right? And so, and this is used to justify the fact that most, uh, medical research is, is done on men, and then we apply it to women with the idea that, that women are gonna respond in exactly the same way as men. Mm-hmm. Um, you know, unless it has to do with the breasts or the ovaries or the uterus.
And, I mean, and that's completely ludicrous. Um, and you know, one of the things I note in my book is that, you know, bikini medicine is. Grounded in bikini science. Yeah. And this is, you know, and, and, and it's
not as fun as it sounds. No. It's not
a
beach party, you guys.
No, I mean, and, and you know, scientists, and again, this, this gets out to the way that women's cycles were handled by research.
It's like, it, we are treated just like men. You know? And, and when, when you look at women's health research and the women's health initiative or whatever, it's always about things that have to do directly with reproduction or menopause. Mm-hmm. And it doesn't have to do with the health of women. Yeah. And it's like, the fact is, like women, you know, our bodies are different than male bodies.
And, um, and to study women's health, that means [01:17:00] that you need to study things like Alzheimer's disease, cancer. Heart disease, lung disease, asthma. You need to study that in women as women. And, um, and, and we're not doing that. We're treating male and bo female bodies is indistinguishable, indistinguishable from one another and it's completely inappropriate.
Mm-hmm. And it's one of the reasons that, um, we are, you know, so overwhelmingly more likely to be, be misdiagnosed. It's one of the reasons that we're more likely to have. Um, bad side effects from medications. It's just because people aren't appreciating that sex runs through the body. Yeah. And it runs through the brain.
And, um, yeah. And this is part of the, the big problem that we have and, and certainly, you know, with an issue like PMDD, which is, you know, a mood related disorder primarily, um, not very well studied in women and we know very little about it. Um, one of the things that I, I can say is that, um, what research tends to support is, you know, 'cause there's all of these different factors that are oftentimes [01:18:00] working against a woman when she has PMDD.
So oftentimes there is, um, like sort of a neuro atypicality. So whether it's dyslexia, A DHD, um, autism, right? So you've got that, you've got dysregulation in the HPA axis, you've got dysregulation in the inflamma in inflammatory activity in the body. All of these things can be improved upon if we can try to increase cellular and neuroplasticity in the body.
Because like anything we can do to support the health of our body is going to support the health of our brain. Mm-hmm. And it does allow us to coast through these hormonal changes in a more graceful way. And this doesn't mean that you can sort of, you know, eat healthy and exercise your way out of PMDD because for a lot of women it's not that simple.
And it's really hard to exercise when you're so sad mm-hmm. That you don't wanna leave the house. And, um, but anything that you can do, even small changes that you can make to help support the health of your body, help support the health of your [01:19:00] brain, help support neuroplasticity and brain plasticity, and those things are going to make it a little bit more manageable.
And so, one thing that I try to. Emphasize in my book is just really, you know, really taking seriously the idea that the brain is a body part. Mm-hmm. Because I think that we forget that, you know, I think that there was this, there was this quote, and I'm gonna butcher it, but, um, there's this, uh, this was said by I think like an eastern philosopher, and they said that in the west we think about our brain in our head as this thing that just, or no.
Lemme say that again. We think about our body as this thing that just takes our head to meetings, right? Yeah. And it's just like this idea that, um, that that totally separate from one another and we totally discount how important the body is. Um, but our brain is a body part and we treat our body well.
And we do things like, um, going out and getting sunlight and trying to regulate our sleep by setting our circadian rhythms. Like getting, you know, that morning sunlight in your eyeballs is like super important, um, and [01:20:00] super helpful for getting, um, helping to regulate your circadian rhythms. That's gonna help you sleep better, better sleep, also increases cellular plasticity.
It's also gonna give you more energy to go out and go for a walk, do something in nature, right? If you walk outside and get your body moving, all of that, um, causes a cascade of hormones to get released. That increase neuro neuroplasticity, increase cellular resilience to hormonal changes. All of these things, um, are gonna help.
Sort of start getting the deck loaded in your favor. Mm-hmm. To help be able to tackle some of the ways that you're feeling, whether it's with cognitive behavioral therapy, or if you try a medical intervention. All of these things are going to be supported by better supporting your health. And so one of the things I talk about in the book is really talking about what are some of the things that we can do that are gonna help to support the health of the body that are actually doable.
Because I think that a lot of times if you tell somebody, you know, especially when they're in the throes of PMDD, like, well, you know what you need to do? You need to. Go [01:21:00] exercise. Yeah. Then you need to like eat more vegetables. And it's like, that feels like it's insurmountable for people.
I want you to know, I have definitely ugly, ugly, cried, exercised, and I was like, in my, I have a home gym and I was like doing bicep curls.
There's like crying. My husband's like, what's wrong? Like, what's going on? And I'm like, I'm so sad. And he's like, but why are you doing this? I'm like, I don't wanna be sad. Like, right. So, and I think that, um, you know, I say that because I want women to know that sometimes it doesn't look like the cover of yoga journal.
Yeah. And sometimes it doesn't look like, but there are times where it's like you just have to like do things anyways. And it's, it's hard. But you, you're right that, well what I wanna back up and say though, and I wanna get like more of like your, your natural approach because people, I think some, some people may have already left the podcast 'cause you brought up SSRIs and I think that they're really villainized and I think rightly so, um, in some instances because.
It's one of those things that a woman comes in, she has symptoms, the doctor's like, it must be, it must be [01:22:00] in your head. Just take an ssri. Right? And that definitely happens. But you did say in your book, it's highly unlikely that PMDD is ultimately caused by a Prozac deficiency. But that research does find that SSRIs like Prozac do help women to feel better.
And what I want for people listening to understand is. We are talking about someone who may take their own life and there's the question of do you give the SSRI and keep the person on the planet, or do you risk them no longer being with us? And it's a hard call in some instances to know that like, you know, whether something natural is going to be enough.
And so I also want people to understand that you can always take an SSRI. And what I love about the Saffron research coming out, which by the way, that's, that's my go-to. I love Saffron and that's what I take personally. But that like, if you start to have like the libido side effects, something like Saffron can help with that.
But we see other things like you can start the SSRI. Then you can start exercising and then you can start doing these other things. Now you're actually able [01:23:00] to rally and then you're able like to come off the ss. Right? Right. We see this sometimes the same thing with like endometriosis. Sometimes we put you on the pill, we stop your period, you don't menstruate, we take you off of it.
So's. Three months and you start the nutrition, you start the lifestyle because now you have the energy and capacity to do that. And then you come off. It's not always like you're a failure if you use a medication or if you use a medication, you have to be on it for life situation.
Right? Yeah. No, it's not all or nothing.
You know, and that's like, one of the things I, I really wanna highlight in, in the book is that not in the whole, I am not somebody who is an advocate for, um, antidepressants, especially as, uh, usually dosed, particularly in teenagers. Mm-hmm. And, um, and I think that they're given to mask a lot of problems. I, I remember, um, and my mom is gonna hate me for, I, I love my mom, but my mom's answer to like, everything in life is divorce or antidepressants.
Oh really?
Mine is drink water. Take a nap. Yeah. Oh my God, that's so funny. My
mom, so I remember with my, um, with my second child and, you know, I was like getting ready to [01:24:00] go back to work and, um, and thankfully, you know, we, um, have a nanny at home, which makes things better. But, um, it was like, you know, three months.
Four months after he was born. And even though I have a very supportive workplace and I was able to pump and I was able to work from home a lot and and still do the regular things, it's hard, right? Yeah. So I was like crying. I was like crying in my mom's life and I was crying every day because I was so sad about having to go back to work.
And my mom was like, you know, you might, I think you might need, I'm like, mom, I'm sad because this is sad. Like it is a sad event for a woman to leave her her very young baby. Like this is hard for women. Well, to
mention, you know, we've been talking about like this whole hormonal transition and how your brain has to adapt.
Oh yeah. What happens in pregnancy? So you have all this estriol, so e three, different time of estrogen. You have all this progesterone, but also your cortisol response is different. And then you shift to postpartum, you lose all those hormones and your cortisol response is changing. Then again, it is why whenever people are like, oh, six weeks is enough, and why should a woman have a vacation just 'cause [01:25:00] she had a baby.
And I'm like, her brain literally has to remodel over the next. Six months and change everything. That's just the brain. Not to mention, could we talk about what happens to our vaginas? Like, yeah. Yeah. No kidding. It's like they go through the ringer there. It's so
crazy. It's so crazy. Yeah. So I'm not a big, I'm not a big advocate of antidepressants.
I think that they're a sort of a last ditch. Um, you know, piece of medication that a person can use. But I, I want, like so many women when they're suffering with PMDD do get into a place where they can't do anything.
Mm-hmm.
And, um, and they are thinking about taking their own lives. And I'm so thankful that we have this medication that's out there for these women, even if they're only on it short term.
And I think that it's great if they're only on it short term, because the fact is, um, if you're able to get your body working back with, with itself instead of against itself. A lot of women are able to feel a lot better without medication. Mm-hmm. And so I think that, you know, just letting people know about what's available.
Um, and again, yeah. As I note in the book, it's like PMDD is not the result of a pro a Prozac deficiency. [01:26:00] Yeah. Right. It's like, it's, it, that's obviously not the problem. Right. But for some women, they can find it really helpful for, um, a month or two while they're able like to feel more light mm-hmm. And more stabilized.
And then they're able to do things like go out for the morning walk and then even maybe be able to begin to, um, exercise more vigorously, making sure that they're getting enough sleep, creating those types of social connections. Because all these things that support the cycle and that support mental health as we transition between different hormonal states do require, um, some ability to, um, you know, go out into the world.
Yeah. And some of these women really get into a really bad place before they're able to get the help that they need. Um, for a woman who's recognizing what's going on early on. Then I think that it makes sense to, you know, first try the, the behavioral techniques, right? Mm-hmm. So for example, cognitive behavioral therapy has been, as I noted, um, uh, neurofeedback therapy.
These have been found to be effective, um, changing diet and exercise, um, exercise, [01:27:00] and I'll say this here and I'll say it a million times, and then people say, send the papers. So we can put some in the show notes. But exercise is at least as effective as antidepressants in treating depression, right? And this is depression of all, all sorts, whether it's it's stemming from hormones or whether it's.
Stem, it's stemming from other issues like that are not, not hormonally related. Mm-hmm. It's as effective as antidepressants, at least as effective as antidepressants. And it can feel really hard to get to the gym when you aren't accustomed to going to the gym and when you're in a hole. And so my, it makes some recommendations in the book for ways that women can have it stack to try to get themselves to a place where they're actually getting a therapeutic dose of exercise.
Mm-hmm. And even if it means for the first day, you know, you just go outside and you walk for five minutes, you, you go back home, you sit down the next day you're gonna walk at least five minutes and see if you can push yourself a little bit further. And then you just keep building from there. Yeah. But I mean, there's a starting place for everybody, you know, and [01:28:00] even if you are somebody who's never exercised and it seems like totally foreign, if you build it into existing routines, it's going to make it a lot easier.
Mm-hmm. You know, so like for me. Um, I just recently picked up the habit of, of getting more morning sunlight, um, right on my eyeballs to set my circadian rhythm. Yeah. So that way I'm able to sleep better, which was part of the reason I was so tired at dinner last night. I know these poor women got up at four o'clock in the morning.
Yeah. I was like, four o'clock Texas time. And I was like, oh my gosh. Um, but it's, it's because I am in the morning, I would sit outside and have my coffee in the morning anyway. Um, and so I was like, okay, I'll sit outside in the sun and make sure I'm getting sunlight. And then, um, and then it gradually changed into a morning walk with my coffee.
So it's like I started just sitting outside with my coffee. Then I moved sitting with my coffee outside in the sun, getting sunlight into my eyes. Next it was taking a little walk with my coffee outside, and now it's turned into every morning I walk at least an hour. Nice. Yeah. Without my coffee. Yeah. So during my coffee beforehand, but it's like I gradually built up to that by habits.
Stacking. So I started with an existing [01:29:00] habit, and then I made a minor modification for that until my brain felt safe and happy. Yeah. And then I made another change because the thing is when people try to make too many lifestyle changes at one time, it feels foreign. Mm-hmm. And their brain, your amygdala actually gets activated.
And people don't realize that your amygdala is like, shut it down. Yeah. It's like, it's like, oh my gosh, like what is this? It's different. Like, I don't know what this is and it's scary and I don't like it. And so like taking these little tiny steps where you can have it. Stack. Mm-hmm. And take existing routines and just make a minor modification with them.
Be patient with yourself. Make small changes, get used to the small change. And then once you're really comfortable with it, then make another small change. And you can do this over time and, and eventually, you know, and it doesn't need to take 10 years, you know, it can take a relatively short period of time before you develop new habits.
Um, that are going to help support your health and, and, and eating whole foods. So avoiding processed foods. 'cause that's another one where it's like the amount of inflammatory activity that goes on from lacking diversity in our microbiome. Mm-hmm. And having the rise and [01:30:00] fall of blood glucose constantly, um, is just really, really hard on the body.
And it erodes, um, our plasticity and our ability to be resilient to hormonal changes. So again, making small changes. And I, I talk about how I have a adopted, 'cause, you know, I'm like you, I, I work a lot and I know that you've worked a lot too. We were all talking about at
the table last night. I like, I was like, work balance.
Like what? Higher, like table full of people that are like workaholics, like, but we love what we do. Yeah. Yeah. That's, it's so hard when it's like, I, the work-life balance thing is just like when you're like, but. This is the thing I love. Like this is what brings me joy.
Yeah. No, and it's just like trying to, I talk about ways that I've, I've learned to, 'cause I always in my refrigerator keep storage, like glass storage containers full of chopped up vegetables Yes.
That I can grab hand handfuls of and you know, those little things like that and how to prioritize getting those things done so that way you have those things in your refrigerator and ready for you. Um, but just anything, you know, it's like the health of the body is so simple mm-hmm. In some ways that [01:31:00] people almost don't wanna listen to it.
Yeah. Because it just seems too airy fairy because it's not a sledgehammer approach, but it really is like, when you improve the health of your body, it is amazing what what it will do for you in return. And um, and just to give another example of this, and this has to do with hormones. Um, one thing that most people don't recognize that I think is so.
Cool. It's like one of the cooler things I learned about hormones last year, or I guess it was two years ago now when I was, um, starting to research the book, was about testosterone and anxiety. Mm-hmm. Yeah. And it's like when your testosterone is low, a lot of times you develop anxiety. And the reason that testosterone and anxiety are linked is because testosterone is, I mean, among other things that it measures is it measures your sort of formidability, right.
So it's like your ability to deal with threats. Mm-hmm. And when you're really weak and sick, your testosterone is lower because your body's essentially telling you if somebody comes after you retreat. Yeah. Right? Because you are not in good, you know, you are not in good condition. And part of that [01:32:00] submissive sort of, um, milieu or like part of that submissive.
Syndrome we can call it is, um, is anxiety. Mm-hmm. Because anxiety is nothing more than our brain lowering its threshold for what It's considering a threat. And when testosterone is low, which again is an internal cue that you're, that your body isn't in very good condition right now, whether it's that it's sick or you're not, you, you don't have enough strength.
Um, your, your smoke detector is gonna be super tuned to threats. Yeah. And that creates anxiety. Mm-hmm. And so one way that we can support ourselves and increase. Um, our ability to self manage anxiety and not experience it at all is by lifting weights and building muscle mass. Mm-hmm. Because building muscle mass is something that can increase testosterone levels.
And when we have higher levels of testosterone that supports our mental health by decreasing, um, by decreasing anxiety, and it's like nobody, you know, it's like you're not, your doctor's not gonna tell you that at the doctor's office. They're not gonna say, go and do a little resistance training to decrease your anxiety.
Um, instead they just give you medication and say, [01:33:00] take two of these and call me in the morning. Um, but there are so many ways that by supporting the health, um, of our physical body, that it really all works together to help, um, promote mental health and help to smooth the transitions, um, between different hormonal states.
Mm-hmm. You know, as you were talking about testosterone. When testosterone's low, we see women have a hard time with boundaries. They have a lot of people pleasing going on. And it's interesting when you put it in the context of like, because you are not strong enough to defend yourself, that even in the modern world that we've adopted to slightly, we've totally adopted, but it is that we're gonna people please.
Mm-hmm. Like we are, we can't set a boundary because we're not, we don't have the mental and physical fortitude to actually reinforce that. And as you're bringing up exercise, I've been nerding out on the research on lactate or actic acid. 'cause forever we were like, this is just a metabolic waste byproduct.
Yeah. And now we're like, oh, it's jump starting like neuroplasticity. Like it's giving your brain fuel. And so [01:34:00] when you say like, exercise is rivaling in SSRI and the mechanism of action of the SSRI may be neuroplasticity. Well exercise is doing that for you. Not to mention like your SSSI isn't gonna be pumping your blood flow the way like a cardio class or weightlifting is going to be doing.
So I think that's a really good thing to underscore of like how necessary and important exercise is. I wanna ask you perimenopause. Mm-hmm. And PMDD. Often women are told things like your PCOS, your endometriosis, your PMDD, they're all gonna get better when you go into perimenopause menopause. What is, I know, right?
I like, as someone with endometriosis, I'm just like, yeah, no, no. Uh, but this is what doctors say, right? It's just a, a myth. Someone probably said, uh, you know, at a grand rounds one time and it just got passed around the campfire, like, you know, a little game of telephone. So what does the research really say about PMDD and perimenopause?
Um, perimenopause is a time when most [01:35:00] women get worsening of everything. Mm-hmm. And the reason for this is, the first thing that happens when we're going through perimenopause is, um, as ovulation becomes sporadic and weak. Um, so meaning that your body is actually developing egg follicles and you're getting a dominant follicle, but then it's.
Not really going anywhere. Um, you don't release progesterone. And so you'll get, you know, estrogen being released as your body is starting to stimulate egg follicles. 'cause that's what's responsible for the production of the big estrogen bump that we get prior to ovulation. And so you get this going on.
So estrogen is being produced, but if we have, um, a, a non robust egg or the egg, it doesn't develop correctly. It'll just get reabsorbed in. The body never gets released. There's no corpus lutetium, there's no progesterone. And when we're going through this. State of constant estrogen, which is again, very stimulatory.
Mm-hmm. And no progesterone, which really counterbalances, uh, that rise in estrogen. Um, it makes women feel on edge. They're not getting that GABAergic activity in the brain that's really calming and [01:36:00] kind of kumbaya. Mm-hmm. Um, they're also getting over proliferation of the uterine lining, which is why you get the worsening of endometriosis.
I mean, it can just really be a terrible time for women. And, you know, the idea, you know, when, when many doctors, um, are reluctant to give women, uh, biologically identical hormones, and if they do, they just give them estrogen. For a lot of these women for a couple of years at least, they would do just fine just taking progesterone.
Mm-hmm. Because a lot, that's where a lot of the issues are, are, um, popping up. And this is, um, in part what's responsible for the worsening of, uh, premenstrual symptoms that happen postmenopausally. Um, and so while those things may resolve and feel better once you're in full menopause, during that 10 to 15 year period, um, when you're in this state of hormonal transition, things can get a whole lot worse.
Yeah. And for a lot of women, they really are.
Mm-hmm. Yeah. And not to mention as we weren't talking about the HPA dysregulation, that takes effect in that time as well. And [01:37:00] I completely agree with you. It's very, so I've been prescribing hormone replacement therapy, treating menopause, perimenopausal women for over a dozen years.
And the number of doctors, so. I generally start with progesterone. 'cause I'm, if I'm seeing you early enough, it's progesterone that we're starting with. 'cause why should you have to suffer? Right. Then I would start women on estrogen before they were officially in menopause. So everybody, like you don't have a period 12 months to the day, that's your birthday, your menopause next day, your post menopause.
But doctors were very much, um, the majority consensus was like, no, not until she's there. That's but most of the symptoms and feeling like hell is happening before then. But it's so interesting because. It even. It's only now. I would say only now in 2025 starting to turn the corner. So whether you had a uterus or not, I didn't care.
I was also going to give you progesterone if I was giving you estrogen, because I knew you would sleep better, you would feel better. Like progesterone is doing so much [01:38:00] more than just protecting the uterine lining. That's so frustrating. And still today, there are doctors like, who will tell me like, there's no reason that you're giving her progesterone and that's not the guidelines and you shouldn't do it.
And I'm like, but sometimes we gotta go off script because the guidelines were not updated fast enough. We're not like this woman. Sometimes I'm with a patient and she's looking at 20, 25 years left of her life. Mm-hmm. Why am I gonna say, you know what? I know you feel bad, but the guidelines tell me that it doesn't matter.
Like I, you don't have a uterus, therefore, I'm just gonna give you estrogen. I also have gotten pushback because women with endometriosis, they have a hysterectomy. I still give progesterone. Why? Because I don't know where those other lesions are. Are we certain there's not a lesion somewhere else in your body?
And if I give you just estrogen, we're gonna stimulate that. I mean, you telling me this,
so let me, let me just say that I'm late to the party of understanding that doctors were only giving micronized progesterone to women if they had a uterus. Crazy. I just, right. They're still doing it. No, I just learned this like a month ago and I was like, and I'm like, wait a minute.
Hold [01:39:00] on. Can you repeat that? And then, and then I heard the, the sort of status quo, um, in hormone treatment and that they're only giving it when there's a uterus. And that, again, and I loved your, what happens in Vegas stays in Vegas thing. Um, but that's like, that's based on this idea of uterus island.
Yeah. Right. And, and as you said, you know, what happens there doesn't stay there. It doesn't just stay there. There are progesterone receptors throughout the body. Mm-hmm. That is absolute insanity. And honestly, it represents a complete misunderstanding of the way that hormones work. And so anybody who says, I'm not gonna give you progesterone because you don't have a uterus, and that's the only thing that it influences, doesn't know anything.
They need to retake human physiology because that's, I mean, it's madness. Yeah. And even just to give a, a simple exam, I mean, it modulates the immune system. And in fact, one of the, um, reasons that it's been hypothesized that, um, autoimmune disease is so high in women now is because, um, progesterone is potently anti-inflammatory.
Mm-hmm. And the [01:40:00] female immune system is way more powerful than the male immune system. So left unbridled without, um, progesterone, uh, to help modulate the immune system. So just under the, um, influence of estrogen, the female immune system will go absolutely bonkers over anything that it encounters. Mm-hmm.
And um, and the reason for this is that we evolved for most of our history, spending a long span of our adulthood, either in the luteal phase or pregnant.
Yeah.
And so our bodies are adapted to progesterone. And so taking that away is one of the hypothesized reasons. That women have such high rates of autoimmunity mm-hmm.
Is because we are no longer exposed regularly to high doses of progesterone because we spend much less time pregnant. And that this leads our very overactive, um, immune system to, to auto react. And so the, the idea that progesterone only matters for that when it, it also helps remodel bone tissue, it remodels breast tissue leading, um, cells from a proliferation state into a differentiation [01:41:00] state, which reduces the risk of breast cancer.
It causes all kinds of changes. You know, throughout the body, outside of the uterus. And so the idea of not giving this mm-hmm. Because you don't have a uterus. Like when I first heard it, I like literally thought I misheard what the person was saying because it was so nuts. Yeah. And it's like, I just couldn't, I couldn't get over it.
I'm like, you do understand that that's not the only place where there's receptors for this hormone, but this
goes back to bikini medicine. Right. Well, no, totally. That this, the only reason to ever treat you is because it's got a, something to do with your uterus. Or something to do with your breast. I know.
It's, it
is based on like a fundamental misunderstanding and mis. Representation of what sex differentiation means. You know, like men and women are biologically different from one another because our bodies have to be biologically different from one another because of the different demands of each sex for the act of reproduction.
Mm-hmm. And that has led to the evolution of sex differences in systems ranging from our cardiovascular system and immune system to our brain [01:42:00] and our reproductive systems. I mean, it's all over the place in the body. Mm-hmm. And we need to move away from bikini science and bikini medicine if we wanna actually promote the health of women.
'cause women's health is not just about the health of the breasts and, and the uterus. Women's health is about the health of women, which means women from head to toe.
Yeah. And you know, as you brought up before, men have testosterone, which they have estrogen too. They have these other hormones, right? Yeah.
Yeah. But that's their primary hormone. Women have two primary hormones, so. Why, if we know that if a man didn't have testosterone enough testosterone, we would, we replace it. We do that. Why if a woman doesn't have enough progesterone, do we just act like, uh, game over doesn't, yeah. It's, it's,
it's like estrogen is seen as like the female hormone.
Yeah. And I think that part of it is just birth order. Right. Uh, estrogen was discovered first and then progesterone was discovered later. And so I think that it was like, oh look, it's estrogen. Like men have one hormone women, women have one hormone. And then they're like, oh no, look, there's two. And then it was just kind of ignored.
And, um, and I think that it's [01:43:00] 'cause it was inconvenient. Yeah. You know, because it is inconvenient. Like our cycles as a scientist and I'm, I still work in the research lab and run studies. Um, it's hard, you know, studying women and having to make sure that you get them at the right point in the cycle and then making sure that you get them in one phase and then you get them in the other phase.
It is harder. It doesn't fit in the male model of research mm-hmm. That we've created. And science was created with the idea of men in mind who have a one size fits all primary sex hormone that. Pretty much the same day in and day out. Um, and we require something different. And I think that the inconvenience just led researchers to say, ah, you know, it only matters for the breasts and the uterus anyway.
We'll just, you know, ignore it and just study women in this other phase. But yeah, it's, it's completely nuts. That we are only giving women estrogen when we have two primary sex hormones. And calling it hormone therapy is ludicrous. Mm-hmm. In fact, I, so I read an article, um, in The Atlantic, which I love, so Atlantic, don't get mad at Me.
I love you. Um, I love, I love The Atlantic. Um, and the, and the, and the writers actually somebody I also really like, she's somebody whose [01:44:00] articles that really enjoy, but the, there was a, a headline where it said, um, something to the effect of hormone therapy is finally starting to change to actually account for the hormones that women have.
And I'm like, oh my gosh, this is great. It's finally talking about progesterone and I'm reading it. And it was about estrogen and testosterone and it never meant, it is mentioned progesterone, a couple of places in there, but not as something that needs to be added into hormone therapy. Mm-hmm. And I was like, this is madness.
I mean, it's complete madness that we're not, it's, it's, it's been an absolute and it's an unsung hero in terms of, um. Promoting brain health, promoting mental health, promoting anti-inflammatory activities in the body from head to toe. Mm-hmm. I mean, it's, it's like a really beautiful hormone. And, um, and it's just been absolutely, you know, cast aside, you know, and, and nobody pays any attention to it.
And so I, I wrote the period brain because like, we need to pay attention to this. Yeah. It's like this is, this is a hormone, you know, in which a cycling woman spends at least half of [01:45:00] her adult life, you know, under the primary control of it plays such an important role in creating the experiences of who we are.
It can play such an important role in creating hormone therapy that actually makes women feel better. It plays, I mean, it. It's part of who we are and the idea that we've just totally left it outta the conversation until now. Totally inappropriate when we are a female body. That cycles.
Mm-hmm. I wanna ask you one last thing.
I get pushed content all the time. Uh, people are like tele on gynecologists. I see. So I get all this content all the time. Gynecologists saying ovulation is optional. It's not necessary. There's no research to show that we actually need to ovulate or there's any problem with that. And gynecologists who say, I'm a fan of menstrual suppression, therefore I recommend it to all my patients, I take issue with bias of like, just 'cause you like something.
Doesn't mean you push it on everybody. Why do you think it is that modern gynecology sees. Ovulation is optional and progesterone's not necessary.
[01:46:00] You know, I think that this all goes back to bikini medicine, bikini science. Mm-hmm. And I think that it's like the only thing that our reproductive hormones and reproductive organs are seen as doing is, um, making babies and our reproductive organs by cycling and by ovulating.
That's the primary way by which the female body produces sex hormones right in our body. We spent our long evolutionary history as a species in, um, being bathed. Regularly in these sex hormones, whether it's estrogen, whether it's progesterone, both estrogen and progesterone. Um, both of those things during pregnancy, during cycling, I mean, it would be like taking away oxygen and then saying, we don't really need this.
Right? Mm-hmm. 'cause if you're able to survive then and not die, which we can't do with oxygen obviously, so it's a terrible metaphor, but, um, but like taking something like gravity, right? And then being surprised when the body falls apart when you don't have gravity on it. Mm-hmm. It's like gravity was a constant throughout our evolutionary history.
And when you put people in space, their bo their bones fall apart if [01:47:00] they don't have them doing different types of exercise, because that was an ev that was a constant. We needed that in order to be healthy, the female body produces sex hormones and it's part of what our body needs to be functioning optimally.
And so the idea that we can just shut that down and that we don't need that is absolutely insane to me. I mean, it just doesn't make any sense at all. And so, you know, and I also hear this with, um. When women are talking about like low dose birth control pills, we're like, oh, it's more na it's more natural because these are the, the levels of synthetics are really low.
And it's like, yeah, there's nothing natural about being in a low hormonal state as of reproductively aged women. I mean, it's like our, what our bodies accustomed to is high and fluctuating levels of hormones. That's like what our bodies are, are designed to operate optimally under and, and suppressing that generally makes people feel terrible.
And we're only starting to understand what the consequences of that are. Yeah. Both in mental health and in physical health.
Well thank you so much for taking the time to chat with [01:48:00] us today. I could seriously, well, you know, we talked forever last night. I could talk to you forever. Uh, but I think if people enjoyed this conversation and they do wanna hear more, they definitely need to grab a copy of your new book, the Period Brain.
Thank you so much. No, I'm really, this was so much fun and I'm so excited to you and I have gotten to have a lot of digital interactions and it's been so nice. Happy face to face.
Thank you so much for joining the conversation. If you could like, subscribe or leave a review, it helps me so much in getting this information out to everyone who needs it.
If you enjoyed this conversation, then I definitely want you to check out this.