Perimenopause fatigue is a hormone-driven exhaustion caused by fluctuating estrogen and progesterone, disrupted cortisol patterns, and poor sleep quality.
During perimenopause, hormonal changes can turn your once-reliable energy levels into an unpredictable rollercoaster. And the cause isn't just getting older, nor is the solution simply needing more sleep.
To help cope with this type of exhaustion, you have to address changes taking place in your brain, hormones, and stress response, which can all collide during the perimenopause transition. Let’s dive into why perimenopause fatigue occurs, what it truly feels like, and how to begin restoring your energy.
In short, yes—perimenopause can cause extreme fatigue, including sudden ‘crashing’ exhaustion, because fluctuating hormones disrupt your stress response, sleep, blood sugar, and brain energy.
In this article:
- Perimenopause and Extreme Fatigue: What’s Really Going On
- Is Fatigue a Symptom of Perimenopause? (Yes—Here’s Why Extreme Fatigue Happens)
- What Does Perimenopause Fatigue Feel Like? Symptoms of Extreme Fatigue Explained
- Perimenopause Crashing Fatigue: Why It Hits Suddenly
- What Causes Extreme Fatigue During Perimenopause?
- How Long Does Perimenopause Fatigue Last? Duration and Timeline
- Fatigue Perimenopause Treatment at a Glance
- Natural Treatments for Fatigue During Perimenopause
- Best Vitamins for Perimenopause Fatigue (Magnesium, B12, Omega-3, Vitamin D, Iron)
- Final Thoughts on Perimenopause Fatigue: You’re Not Lazy—You’re in Hormone Transition
- FAQ: Perimenopause & Extreme Fatigue
Perimenopause and Extreme Fatigue: What’s Really Going On
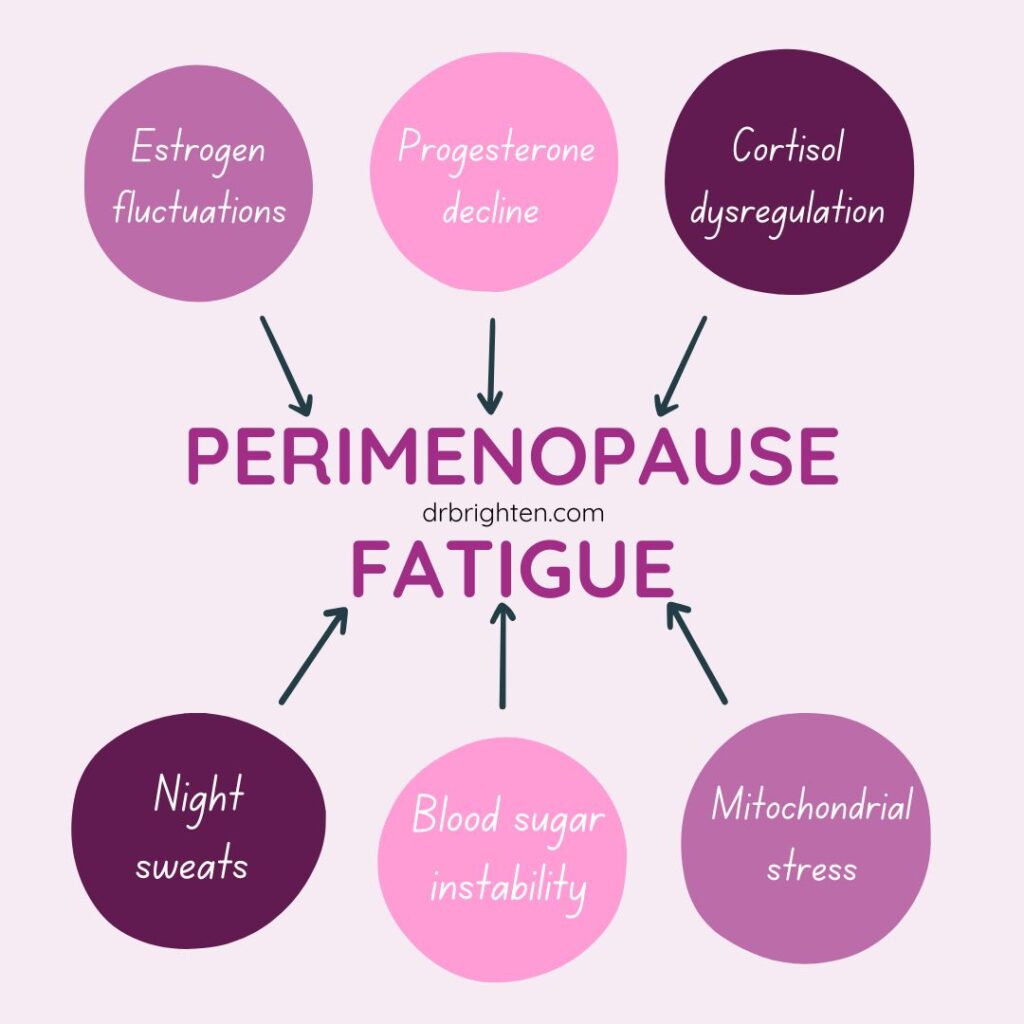
Perimenopause can cause sudden, severe “crashing fatigue” due to rapidly fluctuating estrogen and progesterone, disrupted cortisol rhythms, poor sleep quality, and unstable blood sugar. These hormonal shifts affect your brain, nervous system, and mitochondria—the engines that power every cell—leading to a deep, hard-to-shake exhaustion that rest alone doesn’t fix.
What’s actually happening inside your body:
- Estrogen fluctuations affect serotonin and dopamine, reducing motivation, energy, and mood stability.
- Progesterone decline disrupts sleep cycles and reduces the calming, GABA-supportive effects your brain relies on.
- Cortisol dysregulation creates the “wired but tired” pattern—daytime exhaustion with nighttime restlessness.
- Poor sleep from night sweats, anxiety, or hot flashes prevents restorative, energy-producing sleep stages.
- Blood sugar instability causes afternoon crashes, irritability, and brain fog.
- Mitochondrial stress reduces ATP production, the molecule your body uses for energy.
- Chronic stress makes hormonal shifts hit even harder, worsening fatigue.
This is the physiological “perfect storm” behind perimenopause extreme fatigue—and why you can’t willpower or sleep your way out of it.
Is Fatigue a Symptom of Perimenopause? (Yes—Here’s Why Extreme Fatigue Happens)
Yes, fatigue is one of the most common symptoms of perimenopause, often described as “crashing fatigue.”
In one study that included about 300 women, 46% of peri-menopausal women1 reported symptoms of physical and mental exhaustion compared to just 20% of the pre-menopausal women. Another study found that during menopause, about 68% of women2 regularly felt fatigued.
I'm not just talking about feeling a little tired after a long day. This is the kind of exhaustion that makes basic tasks feel monumental and can hit suddenly, even if you slept well.
Extreme fatigue in perimenopause goes beyond being lethargic because it’s rooted in deep hormonal imbalances, nervous system dysregulation, and mitochondrial exhaustion, not just lifestyle factors.
What causes perimenopausal fatigue? As explained more below, when estrogen and progesterone fluctuate, your ability to handle stress, regulate mood, and maintain stable blood sugar3 takes a hit. At the same time, your adrenal glands can become overworked trying to compensate for lots of daily demands4 and stressors, especially if you’re also dealing with poor sleep or emotional upheaval.
The result: bone-deep, can’t-function, hard-to-describe weariness that doesn’t lift with a nap or cup of coffee. This level of fatigue is a full-body signal that your internal systems need support, not just more rest.
Related: What Is Perimenopause? Perimenopause Symptoms and Solutions Explained
The Truth About Hormones for Sleep, Sleep Disturbances, Melatonin & Perimenopause Sleep Problems
What Does Perimenopause Fatigue Feel Like? Symptoms of Extreme Fatigue Explained
According to surveys5, among the most common perimenopausal symptoms are fatigue, headaches, anxiety, and brain fog.
Here are some clues6 that you might be dealing with extreme fatigue in perimenopause, rather than ordinary tiredness:
- Feeling physically and mentally drained even after getting enough rest
- Cognitive issues such as brain fog, trouble concentrating, and forgetfulness
- Needing caffeine or sugar just to function and get through the day
- Mood swings, low motivation, and feeling overwhelmed easily
- Afternoon crashes followed by difficulty falling or staying asleep
- Having trouble working and staying on top of daily responsibilities
Sound familiar? While every woman is different, this type of fatigue can also be cyclical and worsen during certain times of the month, especially when estrogen and progesterone drop sharply, such as just before menstruation starts.
Related: When Does Perimenopause Start and How Long Does It Last?
These are some of the most common fatigue perimenopause symptoms women report:
- Sudden “crashing” fatigue that hits even after adequate sleep
- Brain fog and difficulty concentrating
- Low motivation or feeling easily overwhelmed
- Irritability, anxiety, or mood swings
- Physical exhaustion that feels disproportionate to activity level
- Afternoon energy crashes
- Trouble waking up or feeling unrefreshed in the morning
- Wired-but-tired feeling at night
- Sleep disturbances, including night sweats or frequent waking
- Increased sensitivity to stress
- Reliance on caffeine or sugar to function
- Forgetfulness or difficulty staying organized
- Heavy limbs or feeling “weighed down”
- Difficulty keeping up with work or daily tasks
Perimenopause Crashing Fatigue: Why It Hits Suddenly
Perimenopause “crashing fatigue” is a sudden wave of overwhelming exhaustion that comes on quickly and feels disproportionate to what you’ve done that day. It’s driven by rapid hormonal fluctuations—especially sharp drops in estrogen and progesterone—that destabilize your stress response, blood sugar, sleep, and mood.
Here’s why crashing fatigue hits so suddenly:
- Sudden estrogen dips disrupt serotonin and dopamine, leading to an abrupt drop in energy, focus, and motivation.
- Progesterone withdrawal reduces your brain’s calming GABA activity, making you feel wired, overwhelmed, and then suddenly wiped out.
- Cortisol instability creates a crash after periods of stress or overstimulation, especially in the afternoon.
- Poor sleep depth from night sweats or anxiety leaves you operating from an energy deficit your body can’t compensate for.
- Blood sugar swings — a common perimenopause issue — trigger mid-day crashes and a foggy, heavy feeling.
- Increased mitochondrial stress limits ATP production, which causes a rapid decline in physical and mental stamina.
- Heightened nervous system sensitivity in perimenopause makes small stressors feel bigger, pushing your body into fast burnout mode.
Crashing fatigue is not normal tiredness. It’s a multidimensional exhaustion caused by hormone-related dysregulation that hits hard and often without warning.
What Causes Extreme Fatigue During Perimenopause?
The short answer: hormonal chaos, often accompanied by factors such as stress and poor sleep.
Results from one study7 found that the quality of sleep among perimenopausal women, and therefore their energy levels, were significantly affected by factors including long-term drug use, the use of hormone medications and/or nutritional supplements, perimenopausal status, and tendency toward anxiety and depression.
Another study8 revealed that out of 220 perimenopausal women who were surveyed, 64% did not have a habit of regular exercise, and 56% had chronic diseases. Fatigue syndrome was found in 64% of the women. The findings suggest that perimenopausal fatigue syndrome is more frequently found in women who have a co-morbidity (chronic illness) and do not stay active, which is an example of why a healthy lifestyle is so important.
Here’s more about what’s really happening when you're struggling with fatigue during perimenopause:
1. Fluctuating Estrogen and Progesterone
Estrogen affects serotonin and dopamine, two brain chemicals responsible for mood and motivation. As estrogen drops during perimenopause9, it's common to feel more tired, anxious, irritable, or depressed.
Progesterone, which has a calming, sleep-supportive effect, also declines, which can disrupt your circadian rhythm (your “internal clock”). This can lead to poorer quality sleep, resulting in more fatigue the next day.
2. Cortisol Dysregulation
Your stress response becomes more fragile in perimenopause. That means your adrenal glands (which produce cortisol) are working overtime. Over time, this can lead to dysregulated cortisol patterns, where you feel wired at night and wiped out during the day.
3. Poor Sleep Quality
Hot flashes, night sweats, and anxiety can make sleep fragmented and shallow. Lack of restorative sleep adds fuel to the fatigue fire. And when you don't get the deep, restful sleep you need, you're likely to be irritable and anxious the next day, creating a vicious cycle.
Related:
Why Can’t I Sleep? The Real Reasons for Perimenopause Sleep Issues (and What Actually Helps)
Perimenopause Anxiety Disorder: Can Unbalanced Hormones Like Progesterone Cause Anxiety?

How Long Does Perimenopause Fatigue Last? Duration and Timeline
Perimenopause can span 4 to 10 years, depending on your body and unique experience. Fatigue often fluctuates throughout this time, peaking in the late 30s to mid-40s and potentially easing after menopause (when hormone levels stabilize).
That said, if you support your body properly—such as by eating well, managing stress, exercising, and prioritizing good sleep as much as possible—you can likely dramatically reduce fatigue even during the most intense hormonal shifts.
The goal is to end the cycle of anxiety and stress during the daytime, causing fatigue, which then disrupts sleep and causes even more exhaustion.
Fatigue Perimenopause Treatment at a Glance
- Adaptogens: Support cortisol balance and help reduce “wired-but-tired” crashes. (Examples: ashwagandha, rhodiola)
- B Vitamins: Boost neurotransmitters, energy metabolism, and mood—especially B12, B6, and methylated folate.
- Magnesium: Promotes deeper sleep, supports the nervous system, and helps regulate stress hormones.
- Sleep Hygiene: Consistent bedtime, reduced evening screens, nighttime wind-down routines, and morning light exposure to stabilize circadian rhythms.
- Stress Reduction: Mind-body practices, breathwork, gentle movement, and nervous-system regulation to prevent cortisol spikes.
- Blood Sugar Stabilization: Protein at each meal, balanced carbs, regular eating schedule, and reduced sugar to prevent energy crashes.
- Addressing Iron Deficiency: Testing ferritin and replenishing iron if low—critical for oxygen delivery, ATP production, and preventing “crashing fatigue.”
Natural Treatments for Fatigue During Perimenopause
Now for the good news: You don’t have to suffer through extreme perimenopause fatigue. Here are science-backed, natural strategies that help restore your energy and reduce burnout:
1. Adaptogens for Perimenopause Fatigue (Ashwagandha, Rhodiola, Eleuthero)
Adaptogens like ashwagandha and rhodiola help your body adapt to stress and remain in balance more easily. They do this by helping to lower cortisol spikes and potentially allowing you to sleep better, which can help improve energy without stimulants.
For example, studies show ashwagandha helps reduce stress and cortisol levels and improves sleep quality and fatigue scores in stressed adults.
Studies also show that rhodiola rosea can reduce fatigue and improve mental performance in adults experiencing stress-related burnout. Specifically, rhodiola was shown to decrease levels of stress hormones like cortisol while enhancing resilience and stamina, leading to reduced brain fog, better mood, and increased ability to handle daily tasks.
These adaptogens work synergistically to buffer the highs and lows of stress physiology, making them ideal for women in perimenopause experiencing energy crashes, sleep disturbances, and irritability.
2. B Vitamins for Perimenopause Fatigue and Low Energy
B vitamins—especially B12, B6, and methylated folate—are essential for cellular energy, mood regulation, and focus. Yet many women become deficient in B vitamins due to stress and hormonal shifts.
Work on increasing your intake of B vitamins with help from foods like eggs, leafy greens, beef liver, salmon, and legumes. You can also supplement with B vitamins to support your metabolism and energy, such as by taking B-Active Plus.
3. HPA Axis Support for Perimenopause Fatigue and Stress
The hypothalamic-pituitary-adrenal (HPA) axis controls your stress response, and, therefore, it's a major player in how much energy you have (or don't have). Nutrients that support this system can improve both daytime energy and nighttime relaxation.
These include adaptogens like ashwagandha and rhodiola, B vitamins (especially B6 and B12), vitamin C, magnesium, and phosphatidylserine. Together, they help regulate cortisol, support neurotransmitter production, and calm the nervous system.
One of the Best Kits for Perimenopause Fatigue:
My Optimal Adrenal Kit checks many of the boxes above, as it provides adaptogens, B vitamins, and other helpful nutrients, all combined into one convenient 3-in-1 kit. These three products are a powerhouse solution for supporting adrenal health, energy, focus, and calm, all with high-quality, science-backed ingredients.
Here's what’s Inside the Optimal Adrenal Kit:
- Adrenal Support: Contains standardized adaptogens (ashwagandha, rhodiola, and eleuthero) to support cortisol balance and the HPA axis. These help reduce burnout, improve stamina, and promote stable energy.
- Adrenal Calm: Formulated to help you wind down by reducing stress hormones like norepinephrine and epinephrine. Includes L-theanine and phosphatidylserine for mood regulation and better sleep.
- B-Active Plus: Provides bioavailable B vitamins—including methylated B12, B6, folate, and choline—for neurotransmitter support, methylation, and energy metabolism. Women with chronic fatigue often have lower levels of B12 and B6, which are crucial for ATP production and mental clarity.
4. Sleep Hygiene for Perimenopause Fatigue and Nighttime “Tired but Wired” Symptoms
Poor sleep is one of the biggest drivers of extreme fatigue in perimenopause, and hormone changes make high-quality rest even harder to come by.
While you can't flip a switch to regulate your hormones, you can take steps to support a healthy sleep cycle. Creating a wind-down routine at night to relax, reducing blue light exposure before bed, and going to bed around the same time each evening can help regulate your circadian rhythm. Getting daytime light exposure and exercising can also help.
Nutrients like magnesium, L-theanine, and phosphatidylserine (found in Adrenal Calm) can assist in promoting a calmer nervous system and help you fall asleep more easily, too.
Related:
10 Best Sleep Supplements Besides Melatonin
5. Stress Reduction to Improve Perimenopause Fatigue
When your hormones are already in flux, unmanaged stress only makes things worse. Chronic stress over-activates the HPA axis, leading to excess cortisol, depleted neurotransmitters, and a general “wired but tired” feeling.
Mind-body practices like breathwork, gentle movement (like walking or yoga), prayer, or even just taking 10 minutes to unplug can restore nervous system balance.
Supplements in my Optimal Adrenal Kit can also help your body buffer that stress more efficiently, giving you a stronger foundation to recover from fatigue over time.
6. Blood Sugar Stabilization and Nutrition for Perimenopause Fatigue
A healthy perimenopause diet can make a big impact on your energy levels and mental health by stabilizing your blood sugar and providing essential nutrients. Here are some tips:
- Prioritize whole, nutrient-dense foods like leafy greens, colorful vegetables, berries, and healthy fats.
- Include high-quality protein (eggs, fish, chicken, beans) with every meal to support blood sugar balance.
- Limit refined carbs and added sugars, which can spike insulin and worsen energy crashes.
- Eat regularly (every 3–5 hours) to keep your metabolism stable and avoid dips in energy.
- Stay hydrated, aiming for at least half your body weight in ounces of water daily.
- Consider anti-inflammatory additions like omega-3-rich fish, turmeric, and green tea.
Related:
The Perimenopause Weight Loss Action Plan, which is designed to give you all the tools you need to reclaim your body and balance your hormones
How to Lose Weight During Perimenopause
Carbs, Cortisol, and Perimenopause: The Real Path to Feeling Forever Strong with| Liz Wolfe
Best Vitamins for Perimenopause Fatigue (Magnesium, B12, Omega-3, Vitamin D, Iron)
In addition to the Optimal Adrenal Kit, these nutrients can make a big difference in managing energy crashes, mood swings, and poor sleep during perimenopause:
Magnesium glycinate (such as Magnesium Plus): For muscle relaxation, sleep, and stress support.
Magnesium is involved in over 300 biochemical reactions in the body, including those related to energy production and nervous system regulation. The glycinate form is gentle on the stomach and particularly effective at calming the brain, reducing anxiety, and promoting deeper, more restorative sleep.
Omega-3 fatty acids (such as Omega Plus): For anti-inflammatory and brain-boosting effects.
Omega-3s from fish oil (EPA and DHA) help reduce systemic inflammation and support brain cell communication, which are critical during hormonal shifts that impact cognition and mood. Studies also suggest omega-3s may improve symptoms of depression and mental fatigue10, especially in midlife women.
Vitamin D3: For energy support, hormone health, and mood.
Vitamin D acts like a hormone and plays a central role in immune function, calcium metabolism, and hormone regulation. Deficiency has been linked to fatigue11, low mood, and even worsened PMS and perimenopause symptoms due to its influence on estrogen and serotonin.
Iron (if deficient): To prevent deficiency, since low ferritin can mimic or worsen fatigue.
Iron is essential for carrying oxygen to your cells and producing ATP (your body’s main energy molecule). Women in perimenopause may experience heavy periods, which can deplete iron stores, especially ferritin, leading to brain fog, weakness, and “crashing” fatigue that doesn’t improve with sleep.
Always talk to your provider about testing your nutrient levels before supplementing.
You can read more about my recommendations for supplements during perimenopause here: 15 Perimenopause Supplements for Happy Hormones
Final Thoughts on Perimenopause Fatigue: You’re Not Lazy—You’re in Hormone Transition
Fatigue during perimenopause is real, and it’s not in your head. The hormonal fluctuations you’re experiencing affect every system in your body, from your brain and adrenal glands to your sleep cycles and neurotransmitters.
But there is a path to better energy, clarity, and calm. With the right support, such as from adaptogens and activated B vitamins, you can stop running on fumes and start feeling like yourself again.
Want Even More Support?
If you're struggling with ADHD-like brain fog or motivation slumps in perimenopause, join the free 5-day ADHD Women's Hormone & Brain Sync Mini Course to learn how your hormones are impacting your focus, mood, and energy—and what to do about it. Check it out here for plenty of useful tools and tips.
FAQ: Perimenopause & Extreme Fatigue
Yes. Perimenopause can cause extreme fatigue due to fluctuating estrogen and progesterone, disrupted cortisol patterns, poor sleep quality, and blood-sugar instability that all combine to drain energy.
Perimenopause fatigue often feels like “crashing fatigue”—a sudden, overwhelming exhaustion that hits even when you’ve slept. Women describe it as brain fog, low motivation, physical heaviness, and trouble concentrating or getting through basic tasks.
Yes. Fatigue is one of the most common symptoms of perimenopause, affecting more than half of women. It’s driven by hormonal fluctuations, sleep disruption, and increased stress reactivity.
Extreme fatigue during perimenopause is caused by fluctuating estrogen and progesterone, cortisol dysregulation, sleep disturbances (like night sweats or anxiety), unstable blood sugar, chronic stress, and sometimes nutrient deficiencies such as low B vitamins, magnesium, or iron.
Perimenopause fatigue can last anywhere from several months to several years, depending on your hormone patterns. For many women it fluctuates throughout the 4–10 years of the transition, often peaking in the late 30s to mid-40s. Fatigue typically improves after menopause when hormones stabilize.
Normal tiredness improves with rest. Perimenopause crashing fatigue feels sudden, intense, and disproportionate to your activity level, and often doesn’t resolve with sleep. It’s tied to sharp hormonal drops, adrenal strain, and disrupted sleep cycles.
Helpful strategies include stabilizing blood sugar with regular meals, improving sleep hygiene, managing stress, exercising regularly, and using nutrients that support the stress response—such as adaptogens (ashwagandha, rhodiola), B vitamins, magnesium, omega-3s, vitamin D, and iron when needed.
Key vitamins and nutrients include:
– B vitamins (B12, B6, methylated folate) for neurotransmitter and energy support
– Magnesium glycinate for sleep and nervous system regulation
– Vitamin D3 for mood, immunity, and energy
– Omega-3s (EPA/DHA) for inflammation and brain health
– Iron if ferritin is low or periods are heavy
Lack of energy in perimenopause comes from hormone fluctuations affecting mitochondrial energy production, cortisol rhythms, sleep depth, and blood-sugar control. Many women also experience more stress, heavier periods, and micronutrient deficiencies that further drain energy.
Yes. Women with chronic illness, ADHD, hypothyroidism, autoimmune disease, insulin resistance, or high stress loads often experience more severe perimenopause fatigue because their stress-response systems, metabolism, and sleep quality are already taxed.
A combination approach works best:
– balancing cortisol (adaptogens, stress management)
– improving sleep (magnesium, phosphatidylserine, nervous system support)
– stabilizing blood sugar with protein-rich meals
– supplementing with B vitamins and vitamin D
– addressing iron deficiency
– optimizing movement and morning light
Many women experiencing perimenopause fatigue leverage my Optimal Adrenal Kit, with B vitamins, adaptogens, and nervous system soothing herbs to help ensure daytime energy and quality sleep at night.
Yes, for most women it improves after menopause when hormones stop fluctuating. With targeted lifestyle changes, nutrient support, and stress balancing, you can significantly reduce or even eliminate extreme fatigue during perimenopause.
References
- https://pmc.ncbi.nlm.nih.gov/articles/PMC5866170/ ↩︎
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8002518/ ↩︎
- https://pmc.ncbi.nlm.nih.gov/articles/PMC11465791/ ↩︎
- https://pmc.ncbi.nlm.nih.gov/articles/PMC4834516/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/39753725/ ↩︎
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8002518/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/21139447/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/34247816/ ↩︎
- https://pmc.ncbi.nlm.nih.gov/articles/PMC10842974/ ↩︎
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9641984/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/38257114/ ↩︎




