If you haven’t heard the term “adrenal fatigue,”it is a common way people describe the symptoms that are a result of something called HPA axis dysfunction. While it can feel like an accurate way to describe how you're feeling, “adrenal fatigue” isn’t a true medical diagnosis. Instead, what you’ll find in the research is the term HPA axis dysfunction, and there can be many patterns of adrenal dysregulation.
I’ve written about adrenal fatigue and HPA axis dysfunction before and typically discuss the impacts of dysregulated cortisol. In this article, I want to dive into another vital adrenal hormone, dehydroepiandrosterone (DHEA).
I’ll answer some important questions, including:
- What is HPA axis dysfunction?
- What causes HPA axis dysfunction?
- How to heal HPA axis dysfunction?
Plus, understanding DHEA explains why Hypothalamic Pituitary Adrenal HPA axis dysfunction affects sex hormones and causes symptoms throughout the body. Keep reading to learn how to support overall hormone balance with a foundation of adrenal support.
In this article
What is HPA Axis Dysfunction? (“Adrenal Fatigue”)
The hypothalamic-pituitary-adrenal axis, HPA axis, is part of the endocrine system composed of hormones and hormone-producing glands throughout the body.
The hypothalamus, the first part of the HPA axis, is a critical part of the brain that performs many functions. One key role is as the first responder to stress. When the hypothalamus senses a threat, it releases corticotropin-releasing hormone (CRH).
The pituitary gland, also in the brain, responds to CRH by releasing adrenocorticotropic hormone (ACTH) into the blood. The adrenal glands respond to ACTH by releasing cortisol (stress hormone), DHEA-S, and other adrenal hormones.
When someone refers to adrenal fatigue, they typically refer to the symptoms associated with low levels of adrenal hormones, which is different from adrenal insufficiency. While this pattern may occur in some people, it doesn’t represent the complexity of adrenal dysfunction.
While many people use the term “adrenal fatigue,” it is important to understand that the adrenal glands do not actually give out or become tired in HPA dysfunction. And your doctor may tell you that your symptoms, along with adrenal fatigue aren't real. Your systems are very real, as a 2016 review determined, adrenal fatigue does not exist as a medical condition1. For more on this story, please read Adrenal Fatigue Isn’t Real.
Despite the 2016 article, “adrenal fatigue” is still commonly used by patients and people experiencing HPA dysfunction to describe their symptoms. There is nothing wrong with using the term to describe how you feel and it is helpful to know that what you’re experiencing is referred to as HPA axis dysfunction (HPA-D) in the research.
The term adrenal fatigue implies it is an adrenal only problem, but as we know, the symptoms arise when the HPA axis is not working correctly. It could look like overproduction or underproduction of hormones, dysregulated daily cortisol rhythm, imbalances in cortisol metabolites, and other patterns.
What Causes HPA Axis Dysfunction?
Under normal circumstances, ACTH signals cortisol to rise in the morning with it gradually declining throughout the day. Cortisol is lowest in the evening when melatonin begins to rise. During times of stress or when someone is experiencing HPA axis dysfunction, the normal cortisol rhythm can be disrupted.
When a patient presents with HPA axis dysfunction, it’s critical to understand the root cause, what’s driving it, and their medical history.
The key determinants of HPA axis regulation2 include:
- Genetic background
- Early life environment
- Current life stress
- Post-traumatic stress disorder (PTSD)

Genetic background
Different genetic polymorphisms (gene variations) can play a significant role in how an individual's body responds to cortisol, which in turn will affect HPA axis regulation.
Early life environment
Prenatal stress has been shown3 to alter the HPA axis in the infant, which can affect them into adulthood. While cortisol is necessary for fetal development, excess levels of maternal cortisol can impact brain development and modify how the HPA axis responds to stress.
Early childhood trauma may permanently alter the stress response4, decrease resilience in adults and ultimately lead to disease.
In a small study5 examining the effects of extreme prenatal stress and early childhood stress in Holocaust survivors, it was found that the effects of stress on the brain persisted 70 years later.
Current life stress
In many cases, the root cause is chronic, long-term stress. When the autonomic nervous system is stuck in sympathetic (stress) mode, the brain constantly interprets stress and sends hormonal signals to the adrenal glands. Your autonomic nervous system is responsible for involuntary actions like heart rate, blood pressure, sexual arousal, breathing, and digestion.
An acute stress response is essential for survival, but chronic stress leads to health issues and impacts how your HPA axis functions, including your hormone levels. Chronic stress disrupts sex hormones, the circadian rhythm, neurotransmitter production, metabolism, can lead to psychiatric disorders, and decreases your resilience to stress.
Research published in Stress Health6 found greater cumulative stress over a lifetime leads to less production of cortisol in an acute stress event or less resilience to stress. In addition, the study predicts greater DHEA production under acute stress for those with more lifetime stress.
Addressing environmental stress you encounter daily is an important step in healing, which we'll discuss shortly.
Post-traumatic stress disorder (PTSD)
According to the American Psychiatric Association7, post-traumatic stress disorder (PTSD) is a psychiatric disorder that may occur in people who have experienced or witnessed a traumatic event, series of events or set of circumstances.
It has been found8 that the type of trauma can impact cortisol levels in an individual, with those who have experienced sexual or physical trauma exhibiting the lowest cortisol levels. People with PTSD may also have lower afternoon cortisol levels.
In another study9, women with PTSD were found to have elevated evening cortisol and cortisol awakening response.
Medications
Besides chronic stress, HPA axis dysfunction may have other root causes, including medication use (or abuse). Long-term use of corticosteroids10 to manage inflammation or opioids11 for pain management has the unintended consequence of affecting the HPA axis.
Additionally, oral contraceptive pills, commonly referred to as the pill, may have an effect on users' stress response. ACTH, the pituitary hormone that signals the release of stress hormones in the adrenal gland lowers during times of socialization. However, some studies12 have found that in women who are taking the pill, ACTH levels do not decline as they do in non-pill users following periods of socialization.
Another study13 found there to be a dysregulated stress response, along with a blunted cortisol response in those using hormonal contraceptives. A blunted cortisol response is when there is a lower cortisol response to stress, which is correlated with depression in some cases.
How Does HPA-D Impact Your Cortisol and DHEA Levels?
HPA axis dysregulation affects adrenal hormone production, including cortisol and DHEA-S. DHEA and cortisol follow a daily rhythm, where the adrenals produce more hormones in the morning, and levels come down in the evening as part of the circadian rhythm.
To learn more about DHEA and the form produced by the adrenals, DHEA-S, please read What Does DHEA Do and When Should You Take It?
Elevated DHEA Levels and PCOS
You may experience elevated DHEA levels during times of greater adrenal hormone production, such as during acute stress response, as well as with certain medical conditions like PCOS.
Polycystic ovary syndrome (PCOS) presents differently in each woman but is often associated with elevated androgen hormones, including testosterone and its precursor DHEA. Interestingly, some symptoms of PCOS overlap with HPA-D14.
For a deep dive into DHEA and PCOS, please read PCOS and How to Lower DHEA Levels Naturally. (add link)
Lower DHEA Levels
Prolonged stress affects cortisol and DHEA production by the adrenals15. Low DHEA levels are one manifestation of HPA-D.
Because DHEA levels determine estrogen and testosterone levels, lower DHEA levels could mean low estrogen, low testosterone, and associated symptoms.
(Note that the ovaries make DHEA, and the adrenals make DHEA-S. The two versions convert back and forth, with DHEA-S making up most of the circulating levels.)
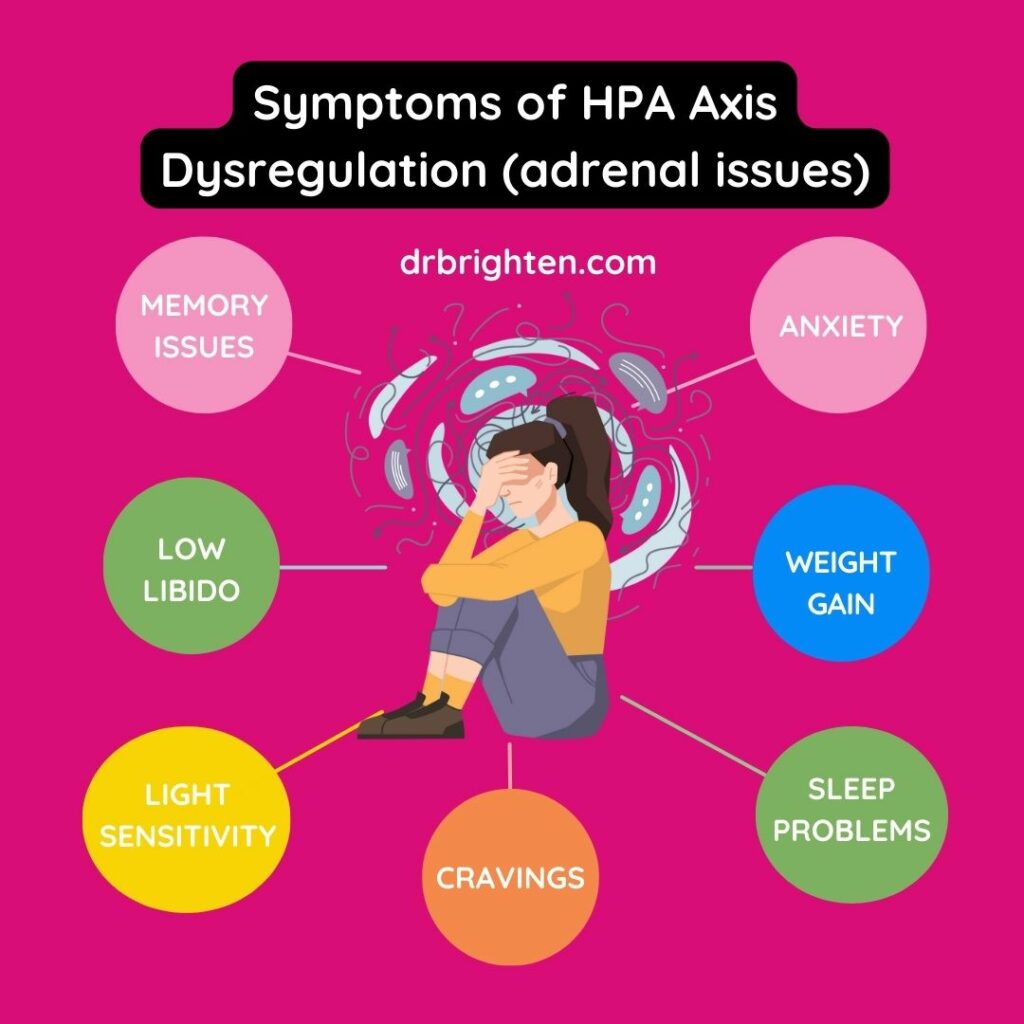
Symptoms of Hypothalamic Pituitary Axis Dysfunction (HPA-D)
Adrenal health affects total body health, so symptoms of HPA-D are widespread.
Hypothalamic Pituitary Axis Dysfunction Symptoms include:
- Changes in blood pressure, dizziness with standing
- Altered immune function, such as poor immune response, inflammatory response, or autoimmunity
- Poor cognitive function, cognitive deficits or memory issues
- Brain fog
- Sleep disturbance or not feeling rested from a whole night’s sleep
- Mood changes, including anxiety
- Low libido
- Weight gain
- Cravings for sugar or salt
- Changes in thyroid health
- Poor stress tolerance
- Changes in sex hormones and menstrual cycle
- Depressive disorder
- Light sensitivity
Let’s look at a few of these symptoms in more detail.
Low Libido
It’s no surprise that when you are stressed out, sex may be the last thing on your mind, but there is biochemistry behind this connection too. Women with low libido, termed Hypoactive Sexual Desire Disorder (HSDD), affects 10 to 14% of women and is associated with HPA-D.
Women with low libido tend to have lower serum levels of DHEA-S16 and other alterations with DHEA-S and cortisol production.
If you are struggling with low libido, supporting your adrenal glands and tending to stress is an important key in recovering from it. We'll discuss steps on how to do this shortly.
As I discuss in Is This Normal, it is also important to note that some people feel an increase in their sexual desire when stressed, which is normal. Sex and orgasms can increase oxytocin, reduce the HPA axis production of cortisol, and can serve as an act of mindfulness. So it is one tool people will use when they are stressed.
Thyroid Dysfunction
HPA-D and thyroid dysfunction share some common symptoms, such as weight gain, fatigue, and sleep problems. Sometimes, HPA-D is the root cause of thyroid dysfunction, so it’s important to work with a medical provider for the proper testing and to help you understand, and effectively treat, the imbalances.
To learn more about the similarities and differences between HPA-D and low thyroid, please read Adrenal Fatigue Vs. Low Thyroid: How to Tell the Difference.
Insomnia
The HPA axis plays a role in the sleep-wake cycle, so adrenal issues could manifest as dysregulated sleep. In addition, stress levels influence sleep and propensity toward insomnia17. Interestingly, women are more likely to have insomnia than men.
A disrupted circadian rhythm can contribute to HPA dysregulation and allostatic load, the effect of accumulated stress on the body. Poor sleep is at the crux of many chronic health conditions and hormone imbalance, with HPA axis dysfunction being no exception.
While many people approach HPA-D by trying to focus solely on increasing cortisol, they are missing the key component of healing, which is restful and restorative sleep. The adrenal glands should “get the night off” as cortisol production declines and melatonin rises to help you get the rest you need. This is why I designed our Optimal Adrenal Kit to include an evening formula, Adrenal Calm, that encourages the evening cortisol decline. The full picture of restoring HPA regulation is to address daytime needs, stress exposure, and support healthy hormone levels to restore adrenal health at night.
Weight Gain
HPA-D may impact weight. Elevated cortisol promotes elevated blood sugar and weight gain, particularly around the midsection. In addition, HPA-D impacts DHEA, estrogen, thyroid hormone, insulin, leptin, and other hormones that play a role in metabolism, eating behaviors18, and weight.
Sugar Cravings
HPA-D is associated with cravings for sugar and salt. Cortisol is involved in blood sugar regulation and with HPA-D, cravings may go up. The adrenals also influence blood pressure and electrolytes, via a hormone known as aldosterone, which accounts for salt cravings.
How to Heal Hypothalamic Pituitary Adrenal Axis Dysfunction (HPA-D)
While being evaluated by a doctor may be necessary given your symptoms, there are nutrition and lifestyle interventions you can employ right now to reverse HPA dysfunction.
7 Ways to Reverse HPA-D include:
- Improve micronutrient status
- Optimize blood sugar
- Practice stress reduction techniques
- Take nervines and adaptogens
- Stay hydrated
- Address underlying infections
- Get mental/ emotional support
Your doctor can assess HPA-D by measuring cortisol and DHEA-S levels via the blood, urine, or saliva. However, saliva or urine tests are often easier and allow for multiple data points over a single day. If your doctor chooses to test ACTH, they will also test serum cortisol levels at that time in order to understand your adrenal's response to the pituitary gland hormone.
If you are experiencing true adrenal insufficiency, you will need to work with a licensed medical provider.
Once you understand your pattern of imbalance, you can target treatment approaches.
Improve Micronutrient Status
Your adrenal glands require specific nutrients in order to produce the hormones you need to feel your best. In addition, brain health is a crucial piece to support as that is where the hypothalamus and pituitary gland reside. Supporting both these areas are key when addressing HPA axis dysregulation.
Magnesium
Stress is well known to deplete nutrients19, including magnesium, zinc, calcium, and certain B vitamins. Unfortunately, as magnesium levels drop, HPA axis dysregulation can become more pronounced, as can anxiety20. This may be especially true in cases of long term stress.
Magnesium can act by way of ACTH to down regulate cortisol production21 and may therefore, reduce elevated cortisol levels.
In cases of extreme stress and depression, HPA-D has been shown to be correlated with a decrease in brain derived neurotrophic factor22 (BDNF). Magnesium has been shown to increase BDNF23 and suppress free radical production in the brain. In this way, magnesium offers substantial brain protection.
Magnesium also plays a crucial role in the metabolism of catecholamines or stress hormones, which is why magnesium supplementation may aid in the recovery of HPA axis dysregulation.
Magnesium is found in:
- Pumpkin seeds
- Broccoli
- Chocolate
- Bananas
For more food sources and benefits of magnesium, read this article.
Vitamin C
Vitamin C is absolutely essential to adrenal health and a key antioxidant24 in protecting these glands. In addition to diet, supplementation may be necessary.
Vitamin C is found in:
- Acerola cherries
- Guava
- Bell peppers
- Strawberries
For a list of additional vitamin C rich foods and the benefits of vitamin C, see this article.
Omega-3 Fatty Acids
HPA-dysfunction and accumulated biological stress have been associated with lower levels of omega-3 fatty acids25. Additionally, researchers have hypothesized that low omega-3 status could in fact be a cause of HPA-D and recommend supplementing in those cases to support HPA axis function.
Additionally, inflammation is understood to be a stressor and a result of HPA-D, as cortisol provides anti-inflammatory protection when in the right levels. Omega-3 fatty acids offer anti-inflammatory support and are brain protective.
Omega-3 fatty acids are found in:
- Sardines
- Mackerel
- Salmon
- Anchovies
For additional omega-3 containing foods and benefits, see this article.
Optimize Blood Sugar
Blood dysregulation can drive HPA-D issues. Glucocorticoids, including cortisol play a significant role in blood sugar regulation, which is why poorly managed blood sugar can significantly affect the HPA axis.
While intermittent fasting has benefits, it's important to recognize that maintaining stable blood sugar both morning and night is essential in healing hypothalamic pituitary adrenal axis dysfunction. In cases where patients are experiencing blood sugar dysregulation while sleeping, which can manifest as waking hungry with anxiety, panic, or feeling hot, it may be best to have a snack that contains protein, carbs, and fat before bed.
How to begin to optimize blood sugar:
- Limit or remove refined carbs and sugar
- Eat protein and fat with meals
- Strength train regularly
- Go for daily walks
- Start the day with 25-30 grams of protein
- Incorporate fiber rich foods into your meals
- Avoid caffeine until after breakfast
Practice stress reduction techniques
Stress plays a role in HPA-D and it’s critical to address and reduce daily stressors. It's important to note that a stressful event that is real or perceived can elicit a hormonal response as both lead to HPA axis activation.
Mindfulness practices, like meditation, breathing exercises, yoga, and others positively impact stress and encourage HPA axis regulation.
In a randomized trial26 of people with self-reported stress, one group received a Mindfulness-Based Stress Reduction (MBSR) program, one group received a local stress reduction program, and the third group was the control. After 12 weeks the MBSR group had statistically higher DHEA-S levels over baseline compared to the other groups, suggesting that MBSR supports adrenal health. DHEA-S is a marker of healthy adrenal gland function.
Take Nervines and Adaptogens
Nervines and adaptogenic herbs support the nervous system to promote a state of calm by encouraging a healthy hormonal response, especially to stimuli that cause HPA axis activation. In addition, adaptogens can have a positive effect in helping regulate the HPA axis.
Adaptogenic herbs like Schizandra, Eleuthero root, Rhodiola, Ashwagandha, holy basil, and Shatavari (asparagus racemosus) may have all long term benefits for the HPA axis27. Taking these herbs in a formula that includes B vitamins can have a synergistic effect, which is why you'll find this combination in our Adrenal Support supplement.
Nervines like passion flower contain GABA, which has an inhibitory effect on stress hormones, meaning it can help you feel more calm and get better sleep. Look for a combination formula of nervines and nutrients that can help reduce stress and tension. You'll find relaxing nervines, soothing adaptogens, and nutrients that encourage a healthy decline in cortisol in the evening all within our Adrenal Calm formula.
Stay Hydrated
One of the roles of the adrenal glands is regulated blood pressure by way of the hormone aldosterone. This is why high blood pressure can be seen in some cases of HPA-D and why others report low blood pressure symptoms, like becoming dizzy when standing.
Replenishing water loss through food and beverages during the day is an important step in healing. In some cases, people benefit from electrolyte-rich water in addition to regular water intake. If you're consuming electrolyte water, avoid sugar heavy drinks, which will contribute to blood sugar swings. This is one electrolyte option I recommend to patients.
Address Underlying Infections
If you are experiencing chronic inflammation due to autoimmune disease or underlying infections, it is important to address these. Working with a licensed health care provider can enable you to get the right testing and treatment.
Get Mental and Emotional Support
Psychological stressors, as previously discussed, can result in HPA-D or be the result of it. While working on environmental stress is important, it is important to recognize that factors like prenatal stress, early childhood stress, and allostatic load need to be addressed as part of healing.
Allostatic load refers to the cumulative effect of life stressors. In some cases, the allostatic load28 can exceed what the neuroendocrine response (aka the HPA axis response) is capable of managing, which is referred to as allostatic overload. Essentially, the “wear and tear” of environmental stress and other stressors can force the body into a state where it is no longer able to adapt or respond to stress.
Examples of factors that contribute to allostatic load include:
- Poor sleep and circadian disruption
- Smoking
- Alcohol consumption
- Lack of exercise
- Low nutrient or unhealthy diet
- Subtle and chronic stressors that elicit an HPA axis response
- Major life events (death, divorce, etc)
- Inability to reduce or turn off stress response when stress is no longer present
- Discrimination29, including racism and weight
While some factors that contribute to chronic stress and allostatic load are within your control, others are not. This is why I recommend all patients work with a licensed mental health professional to develop tools to process, reduce, and recover from stress. Work with a mental health professional to ensure you're taking the most holistic approach to your healing.
Takeaway
The picture of HPA axis dysfunction is often more complicated than “adrenal fatigue” and impacts DHEA levels, affecting estrogen and testosterone and having body-wide effects. HPA-D may explain many cases of low DHEA-S and associated symptoms, like low libido. There are many evidence based steps you can take to build resilience to stress and recover from hypothalamic pituitary adrenal axis dysfunction.
References
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4997656/ ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3860380/#:~:text=Three%20main%20determinants%20of%20HPA,contribute%20to%20HPA%20axis%20disturbances ↩︎
- https://pubmed.ncbi.nlm.nih.gov/20550950/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/19750552/ ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10449780/ ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6377358/ ↩︎
- https://www.psychiatry.org/patients-families/ptsd/what-is-ptsd ↩︎
- https://pubmed.ncbi.nlm.nih.gov/17978317 ↩︎
- https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-021-03170-w ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8360169/ ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10003084/ ↩︎
- https://dent.au.dk/en/display/artikel/ny-forskning-understreger-p-piller-paavirker-kroppens-evne-til-at-regulere-stress ↩︎
- https://link.springer.com/article/10.1007/s11920-019-1095-z ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9498167/ ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8604255/ ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7343293/ ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7045300/ ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7026436/ ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7442351/#:~:text=The%20largest%20body%20of%20evidence,on%20calcium%20and%20iron%20concentrations. ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3198864/ ↩︎
- https://www.mdpi.com/2072-6643/12/12/3672 ↩︎
- https://www.tandfonline.com/doi/abs/10.1080/08039488.2016.1184310 ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7352515/ ↩︎
- https://ccforum.biomedcentral.com/articles/10.1186/s13054-019-2332-x ↩︎
- https://www.sciencedirect.com/science/article/pii/S0306453018302117 ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8604255/ ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3991026/ ↩︎
- https://karger.com/pps/article/90/1/11/294736/Allostatic-Load-and-Its-Impact-on-Health-A ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8172431/ ↩︎

