If you’ve noticed your irritable bowel syndrome (IBS) symptoms get worse around your period, you aren’t alone. Even women without IBS1 can experience gastrointestinal discomfort during their menstrual cycle.
So if you suffer from IBS, things can get even worse during your period. Bloating, cramping, diarrhea (hello period poops) are all symptoms of IBS in women that can be exacerbated by fluctuations in hormones. No, period diarrhea isn’t an absolute sign of IBS, so don’t panic if that happens to you.
Why does this happen, and why do symptoms especially flare during your period? Can your period trigger IBS? I’ll explain below, plus give you some helpful tips to get things under control.
In this article:
- Understanding Female Hormones and IBS
- How to Distinguish Symptoms of IBS from Menstrual Cycle Symptoms
- IBS and Birth Control
- IBS and Small Intestinal Bacterial Overgrowth (SIBO)
- How to Support IBS Symptoms During Your Menstrual Cycle
- Can Supplements Help with IBS?
- IBS and Menstruation: You Don’t Have to Suffer
Understanding Female Hormones and IBS
Changes in hormones involved in your menstrual cycle are linked to worsening symptoms in your gastrointestinal (GI) tract. But why?
One reason is that there are hormone receptors throughout your body, including your GI tract2, which means hormones can stimulate your gut. There are several ways this can exacerbate IBS symptoms.
Menstrual Cycle Hormones
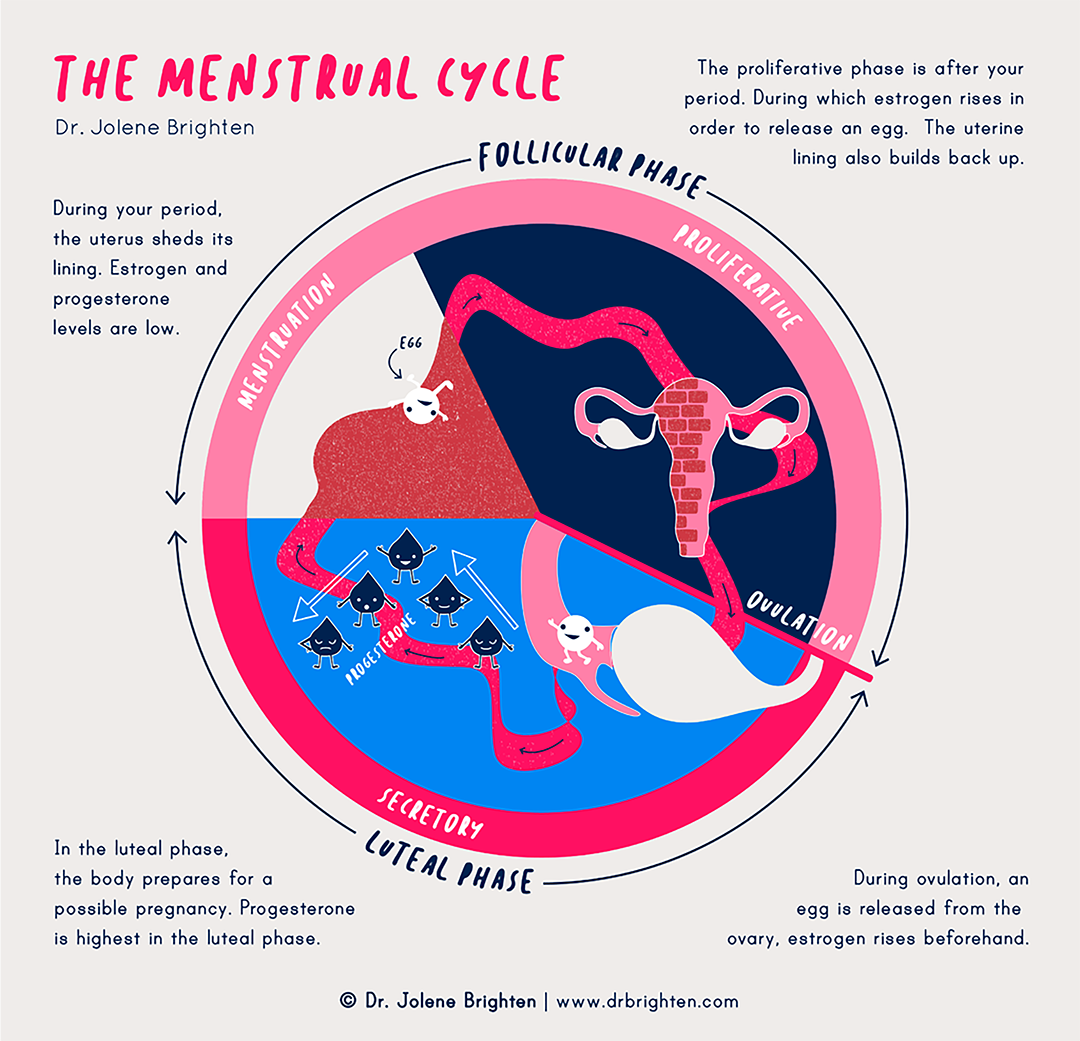
Let’s start with a quick overview of your menstrual cycle3 before we explore the various ways it can affect your IBS symptoms.
The primary sex hormones involved are estrogen and progesterone. Your cycle begins on the first day of your period. During the first half, the follicular phase, estrogen rises to help thicken your uterine lining in preparation for egg release and to help with the ovulation process.
Towards the end of the follicular phase, estrogen peaks and activates the release of luteinizing hormone (LH) and follicle-stimulating hormone (FSH). This triggers ovulation, and estrogen levels drop soon after.
Estrogen persists during the second half of your cycle, the luteal phase, and then drops off towards the end, initiating your period. At the same time, progesterone (the predominant hormone of the luteal phase) begins to rise and peaks during your luteal phase in preparation for pregnancy.
But if the egg is not fertilized, progesterone also drops off to trigger the beginning of your period. Both hormones are low right as you start your period.
If you’re looking for a more detailed breakdown of the menstrual cycle, I’ve got a full guide for you!
How Can Hormones Make IBS Symptoms Worse?
Understanding the patterns of these hormones can help explain why symptoms of IBS can get worse throughout the month.
For example, progesterone can impact your gut motility, slowing the movement of food through your GI tract. So increased progesterone4 during your luteal phase5 can contribute to constipation and bloating for all women, not just those with IBS.
But as both hormones (estrogen and progesterone) drop before your period, you’re more likely to notice opposite symptoms like diarrhea. One study6 on women with mixed-IBS (alternating constipation and diarrhea) found that one-third noticed constipation mainly during the luteal phase. But amazingly, as the women got closer to their period when progesterone and estrogen were low, not one person had constipation as a primary GI symptom.
Estrogen also influences how you experience pain by regulating your nervous system7. Inflammation chemical messengers, and HPA-axis (how your brain and adrenal glands communicate). It does this in various ways, including synthesizing proteins known as neurotrophins8 that regulate pain and boosting opioid receptors9 (also involved in pain regulation) in the brain. Estrogen also can influence the release of inflammatory signaling chemicals that lead to the body’s pain activation.
As a result, when estrogen levels are higher, your GI-related pain may be more tolerable (yay!). But unfortunately, as it drops, as when you get your period, pain sensations can increase.
Studies also suggest that the drop in estrogen and progesterone at the end of your luteal phase can create signals10 in your GI tract that increase stool frequency, urgency, and abdominal discomfort.
Finally, hormonal shifts can also affect the diversity of bacteria11 in your gut and the health and function of your intestinal barrier12—both red flags for IBS.
Essentially, there are quite a few ways that hormonal changes during your cycle can affect IBS symptoms, and they’ll vary depending on a lot of factors—everyone is different. And a lot of this research is very new, meaning that even scientists aren’t yet aware of all the ways that hormones may affect IBS.
While this can be challenging and frustrating, it’s definitely worth paying close attention to how your cycle affects your IBS symptoms. To do this requires that you learn to notice and name subtle shifts in your symptoms throughout the month, which I'll describe in the following section.
How to Distinguish Symptoms of IBS from Menstrual Cycle Symptoms
The connection between your menstrual cycle and IBS can be tricky to figure out because the symptoms look so similar. Symptoms can also change throughout your cycle, as noted above.
Interestingly, IBS is also more common in women13 than men.
There are three primary types of IBS14:
- IBS-D or diarrhea-predominant
- IBS-C or constipation-predominant
- IBS-M or mixed having both constipation and diarrhea
General symptoms of IBS15 in women include:
- Constipation or incomplete bowel movements (feeling like you still need to go)
- Diarrhea with frequency and urgency
- Bloating
- Stomach pain and cramping
- Gas
- Nausea
But IBS can have other symptoms16 that also mimic what you might experience with PMS and your period, like:
- Body pain
- Increased urinary frequency
- Impaired sexual function
- Insomnia
As you probably noticed, most of these symptoms can result from normal hormonal fluctuations on your period. But if you have GI distress all month long, that would indicate your period isn’t the primary culprit.
If you don’t have a definitive diagnosis of IBS, it’s worth seeing a trustworthy health care practitioner to see if the diagnosis fits. Although IBS is common (affecting up to 20%17 of US adults), there are also other causes of similar symptoms, so it’s a good idea to rule out other causes instead of assuming.
IBS and Birth Control
Since IBS symptoms can be exacerbated due to changing hormones, some doctors may advise using birth control pills to help control symptoms. But there’s no evidence supporting using the pill to manage symptoms.
In fact, certain birth control pills may make symptoms worse. A study on drospirenone18, an active ingredient in some birth control pills, concluded that women taking these were more likely to be diagnosed with IBS.
The pill can also lead to inflammatory changes in your gut by disrupting the balance of your normal gut flora19. It’s even associated with an increased risk of inflammatory bowel disease20. You’re likely better off finding other natural ways to support your IBS symptoms.
IBS and Small Intestinal Bacterial Overgrowth (SIBO)
For a long time IBS was thought to be a psychological condition. As it turns out, there may be an infectious component that triggers a temporary autoimmune response that impacts gut motility. You can learn more about SIBO here.

How to Support IBS Symptoms During Your Menstrual Cycle
The same interventions that help with IBS at all times of your cycle can help support your gut health during your period.
There are several ways you can adjust your diet and lifestyle habits to help you feel better.
Eat More Fruits and Vegetables
A diet rich in vibrant fruits and veggies filled with fiber and phytonutrients to support healthy levels of inflammation is oh-so-important when it comes to IBS and your period.
Phytonutrients are natural compounds found in plants that help protect against oxidative damage and inflammation. They can help calm down those prostaglandins21 that contribute to pain. To include more phytonutrients, think bright colors like berries, green veggies, squash, and sweet potato.
If you need more help getting started with a hormone supporting diet, we’ve simplified things for you with our free hormone starter kit that includes a free 7-day meal plan.
Try Eating More Fiber
Fiber is necessary for healthy hormone balance, especially healthy estrogen detoxification22 and regulation.
If you tend towards constipation, make sure you are getting enough fiber to get things moving.
However, keep in mind that fiber can be tricky with IBS as it can worsen symptoms for some people.
Start slow and consider starting with soluble fiber like oats or bran instead of insoluble options like leafy greens if you aren’t used to eating fiber.
Support Your Microbiome
Microbiome-supporting foods like fermented vegetables, kefir, and yogurt (if you tolerate dairy) can all support healthy diversity of bacteria in your gut.
Different probiotic foods work for different people, so it’s worth experimenting. Probiotic supplements are another research-backed option to support gut health.
Stay Hydrated
Hydration is also so important to keep things moving. Dehydration can cause constipation.
Plus, it’s always a good idea to increase your water intake as you add more fiber to your diet.
Whether or not you're feeling dehydrated, try setting hydration goals. One easy way is to carry around a liter water bottle and be sure to fill and drink the entire thing (with purified or spring water, preferably) twice per day, or more if you're very active or perspire a lot.
Move More
Movement is beneficial for healthy bowel function. It can stimulate the muscles in the intestines and help you pass stool more easily.
Studies also suggest that regular exercise23 can help reduce symptoms related to your period.
For best results, aim for about 30 minutes of movement five times a week. Try moving in different ways like stretching, yoga, swimming, dancing.
Manage Stress
Stress24 can worsen your IBS, so it’s essential to find healthy ways to cope with stress (like exercise or meditation).
You may also want to consider a yoga practice with a focus on gentle breathing and stretching.
Focus on Sleep
Sleep is so vital for all aspects of health, including the wellness of your gut. Plus, lack of sleep just makes everything worse, including period25 and IBS symptoms. Try working on avoiding screen time before bed, sticking to a sleep schedule, and attempting bedtime yoga (or gentle stretches) to help you unwind.
Keep a Symptom Journal for a Month or Two
As you work on solving your IBS and period symptoms, you may also want to consider tracking food, lifestyle, and symptoms with a journal to note any patterns. It’s not difficult and can provide an excellent way to measure the impact of what you’re doing.
A good journaling practice can also help identify food sensitivities or other factors that may make your symptoms worse.
Can Supplements Help with IBS?
Yes. In many cases, depending on your IBS symptoms, some supplements can add support on top of diet and lifestyle.
Hormone balancing supplements can support a healthy foundation, while some other options can provide additional support.
Magnesium
Magnesium26 can be especially helpful for those who struggle with body pain. It can also help with relaxation and PMS27.
But if you tend to have diarrhea, choose magnesium glycinate or malate because they are less likely to cause loose stools.
Probiotics
Probiotics can support your gut health, which may be helpful for hormone related fluctuations in gut symptoms or gut symptoms in general.
Your gut is a primary part of hormone detoxification and balance. Certain strains like Bacillus subtilis28 support your gut barrier, microbial diversity, and a healthy inflammatory and immune response.
Multiple studies point to the benefit of probiotics for IBS29.
You can view our Women’s Probiotic that contains probiotics that support a healthy gut, hormones, and menstrual cycle.
Curcumin
Curcumin is an anti-inflammatory, antispasmodic compound found in turmeric.
It can help with reducing PMS30 and IBS symptoms31 through its impact on neurotransmitter and anti-inflammatory activity.
Ginger
Ginger contains phenolic components that are high in antioxidants. It may help to reduce inflammation and help improve digestion for people with IBS.
One study32 suggested that ginger’s anti-inflammatory activity could benefit those with IBS-D (the type with predominantly diarrhea) by lowering the inflammatory response33.
Digestive Enzymes
Digestive enzymes can support healthy digestion and may help with symptoms of IBS around your period and throughout your cycle.
They are especially helpful for feelings of gas, bloating, or discomfort associated with food intake.
Taken with a meal, enzymes can make it easier to break down food so you can absorb the nutrients more effectively.
IBS and Menstruation: You Don’t Have to Suffer
There is a clear relationship between our digestive system and our period. If you have IBS, this connection can make things worse.
But you shouldn’t have to suffer. If you feel miserable around your period or anytime, try some of the lifestyle changes listed above. I encourage you to really focus on food, movement, sleep, and stress management as they are all powerful tools—especially when combined.
Supplements like probiotics can also help support your healing process. If you feel like you’ve tried it all and still don’t feel well, consider reaching out to a women’s health care practitioner for extra support.
Questions or stories to share? Leave a comment below, I love hearing from you!
References
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3901893/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/7227774/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/20869180/ ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4527267/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/14619388/ ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7883586/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/11844293/ ↩︎
- https://link.springer.com/referenceworkentry/10.1007%2F978-1-4614-5836-4_30 ↩︎
- https://pubmed.ncbi.nlm.nih.gov/16723535/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/16368009/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/28778332/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/31364524/ ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6175559/ ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4051916/ ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4051916/ ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4527267/ ↩︎
- https://www.womenshealth.gov/a-z-topics/irritable-bowel-syndrome ↩︎
- https://pubmed.ncbi.nlm.nih.gov/22663950/ ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4752384/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/28542115/ ↩︎
- https://www.tandfonline.com/doi/abs/10.1080/10408398.2016.1251390 ↩︎
- https://pubmed.ncbi.nlm.nih.gov/28778332/ ↩︎
- https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD004142.pub4/full ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4202343/ ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5323065/ ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6786451/ ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3208934/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/32664604/ ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4356930/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/26051565/ ↩︎
- https://www.liebertpub.com/doi/abs/10.1089/acm.2004.10.1015 ↩︎
- https://bmccomplementmedtherapies.biomedcentral.com/articles/10.1186/s12906-020-03059-3 ↩︎
- https://bmccomplementmedtherapies.biomedcentral.com/articles/10.1186/s12906-020-03059-3 ↩︎
