Breast implant illness is starting to gain attention in the medical community. Breast implant illness (BII) is the term used to describe symptoms associated with breast implants and can range from joint pain, skin rashes, hair loss, and headaches to chronic fatigue, anxiety, neurological issues, and brain fog. Many women who identify as having BII experience symptoms after having breast augmentation or reconstruction with implants. As you’ll read in this article, BII symptoms can vary and may not resolve after the removal of implants.
Let me start by saying that I am not for or against breast implants. Instead, I am for a complete and thorough informed consent and supporting a patient in their medical decisions.
This article is here to provide you with information and education to have an informed discussion with your doctor about whether breast implants are right for you, or whether removing implants you already have might be of benefit if you've developed symptoms. These decisions are between you and your doctor, and it’s a good idea to be aware of the issues some women face.
Alright, let’s have some real talk about breast implant illness. Is it real? Is it bad? Is it treatable? Let’s dive in.
In this article:
- What Are the Symptoms of Breast Implant Illness?
- Is Breast Implant Illness Real?
- How Often Does Breast Implant Illness Occur?
- What Are Your Chances of Getting Breast Implant Illness?
- What Causes Breast Implant Illness?
- How is Breast Implant Illness Diagnosed?
- Can You Get Breast Implant Illness with Saline Implants?
- Can Breast Implants Cause Autoimmunity?
- What Is BIA-ALCL?
- Does Breast Implant Illness Go Away?
- How Is Breast Implant Illness Treated?
- What to Do If You Can't Get Your Breast Implants Out Right Now
- How Can You Prevent Breast Implant Illness?
What Are the Symptoms of Breast Implant Illness?
There is a long list of symptoms for breast implant illness. Most symptoms patients report can be related to other body systems, and you may not immediately think, could this be my breast implants?
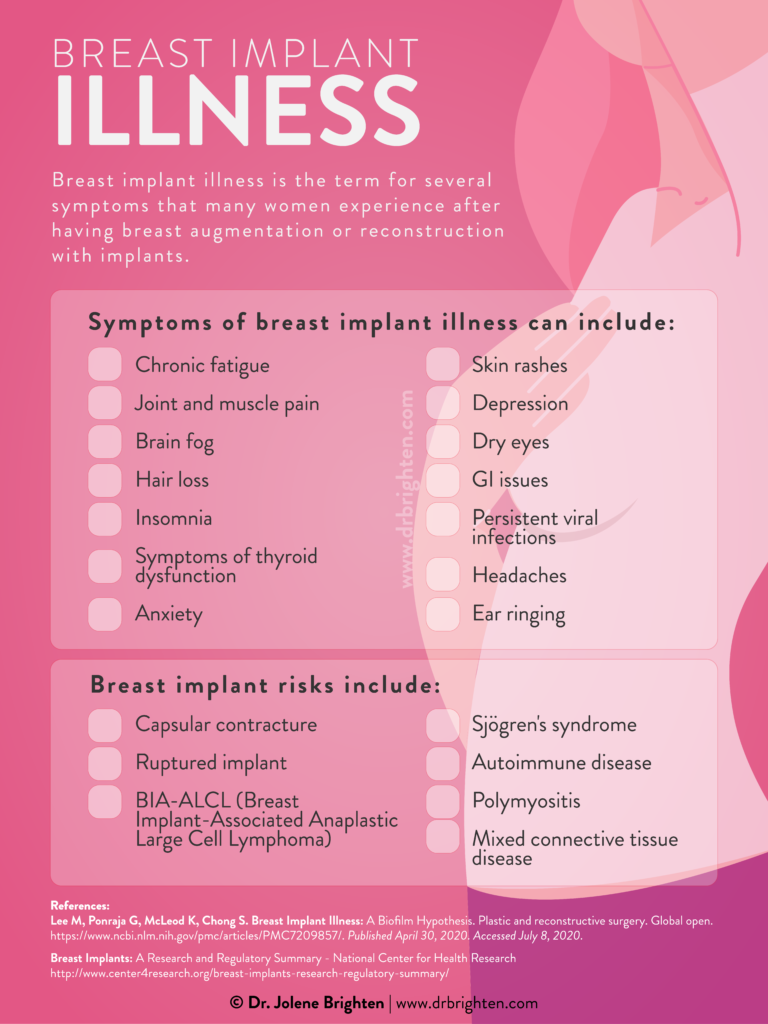
Some of the symptoms of breast implant illness include:
- Chronic fatigue
- Joint and muscle pain
- Brain fog
- Hair loss
- Insomnia
- Symptoms of thyroid dysfunction
- Anxiety
- Skin rashes
- Depression
- Dry eyes
- GI issues
- Persistent viral infections
- Headaches
- Ear ringing
On top of that, researchers have linked silicone implants with higher rates of:
- Sjögren's syndrome (dry eyes and dry mouth)
- Scleroderma
- Rheumatoid arthritis
- Stillbirth
- Melanoma
Real Life Breast Implant Illness Syndrome
Breast implant illness research is still in its infancy and while I highly value the science around this topic, I also believe that the patient experience is equally valuable as we seek to understand this emerging issue. I recently interviewed Krista Tagaras, personal trainer and self-love advocate, about her experience with breast implant illness, and her symptoms. Krista shared that within a year of getting breast implants, she developed:
- Amenorrhea (loss of period)
- Shortness of breath
- Nodules on her thyroid
- Swollen lymph nodes in her neck
- Debilitating fatigue
- Neurological symptoms such as brain fog and memory problems
- Symptoms of hormonal imbalance
- Multiple food intolerances
- Severe IBS-D (Irritable Bowel Syndrome with Diarrhea) symptoms
- Relentless body pain after even small amounts of activity
Since breast implants illness can manifest in multiple body symptoms outside of the mammary tissue (breasts), doctors may not link symptoms like Krista’s to breast implants. Awareness is increasing, but the progression from noticing patterns to research to practice is a slow one.
Is Breast Implant Illness Real?
This is a big question. Like any surgery, breast implant surgeries carry risks. The most common risks patients are advised of breast implant surgery are implant leakage/rupture, incorrect implant position, changes in nipple sensation, infection, bleeding, and accumulation of fluid.
“When I had my implants put in, I was told about and given papers that discussed common possible issues such as capsular contracture, infection, pain, malposition of the implant, etc. I was never informed about breast implant illness or any significant side effects regarding autoimmune problems or other health issues associated with having breast implants. I was also given a pamphlet made by the breast implant manufacturer, which only highlighted the positives and safety of their breast implants.”
– Krista Tagaras
From Krista’s perspective, she was never informed about breast implant illness at all. This could be because, for many years, the adverse symptoms women complained of after getting implants were brushed off by their doctors, or attributed to other things. The compartmentalization of women’s bodies can often lead to missed diagnosis and leave women to struggle for years with symptoms.
Women's Health Conditions Can Be Dismissed
Unfortunately, medical gender bias could also play a role in delayed diagnosis and dismissal of symptoms. Women are often treated differently than men when seeking medical care, and women’s symptoms are more likely to be ignored by medical professionals.
Luckily, awareness around breast implant illness is growing, and women’s concerns are more likely to be addressed. While many more physicians now understand that breast implant illness is real, the vast majority may not acknowledge the potential connection between implants and symptoms.
If you’re still on the fence about whether or not breast implant illness is real, check out this video from BII survivor Karissa Pukas. She details her journey with debilitating symptoms that eventually led her to remove her breast implants.
How Often Does Breast Implant Illness Occur?
There isn’t enough research at present for us to know precisely how often breast implant illness occurs. As more women come forward to address symptoms, more data will become available to the medical community about the prevalence of breast implant illness.
What Are Your Chances of Getting Breast Implant Illness?
There is evidence to suggest that breast implant illness may seem to have an autoimmune component. Therefore, it is likely more common in people with either a personal or family history of autoimmune diseases.
Again, there isn’t enough research available to know a woman’s exact chances of getting breast implant illness. Because of this, it’s vital that women are informed of all the risks before moving forward with breast implants, especially women with a personal or family history of autoimmunity.
I recommend that my patients document all their symptoms or lack thereof for at least a month, if not 3, prior to undergoing surgery. I also order baseline lab testing so that we have a complete picture prior to breast implant surgery. This allows us to more objectively track if any adverse changes occur following surgery, especially if symptoms arise.
What Causes Breast Implant Illness?
At the moment, because most doctors do not recognize breast implant illness as a real condition and research is lacking, it is tough to say why it manifests. It is one of the many conditions impacting women that medicine has yet to invest in, let alone unanimously believe the women who are experiencing it.
Some experts have hypothesized about what could potentially cause breast implant illness.
Some of the Possible Causes of Breast Implant Illness Include:
According to the FDA, some possible causes of breast implant illness include:
- The body might be reacting to foreign objects (the implants) with an inflammatory response
- The body might be reacting to the materials making up the implant (e.g., silicone)
- The body may have an adverse reaction to how the breast implant was inserted
How is Breast Implant Illness Diagnosed?
There is no specific test for breast implant illness. However, a doctor may perform other tests and examinations to determine whether the patient has an autoimmune disease(s). While you may have experienced the onset of symptoms following implant surgery, it is important to have lab testing to rule out other medical conditions.
Can You Get Breast Implant Illness with Saline Implants?
Many women are told that saline implants are safe because they’re just filled with salt and water. They are usually not informed that saline implants can be just as dangerous as silicone implants.
Saline implants are usually not hermetically sealed (meaning they are not airtight), nor are their filling valves 100% secure. Because of this, bodily fluids, yeast, molds, and bacteria can all enter the implant, which leads to decay.
It goes both ways. If things can enter, decaying substances can exit the implant into your body. Over time, the implant contents may start leaking into the chest, and the toxic substances may spread throughout the body.
Many people don’t realize that breast implants (both silicone and saline) have a warranty of about ten years. After that, you should talk to your doctor about whether or not to leave them be, or remove and replace them. Be sure to mention any symptoms you've been experiencing.
And the longer they remain in the body, the greater the risk of complications developing.
Can Breast Implants Cause Autoimmunity?
Many of the symptoms of breast implant illness (such as joint and muscle pain, fatigue, etc.) are also hallmarks of autoimmunity.
Recently, a large multicentered, cohort study was conducted, involving 99,993 women with breast implants. This has been the most extensive study of breast implant outcomes to date. In this study, 56% of participants had silicone implants. What they found was that silicone implants were associated with higher rates of Sjögren's syndrome, stillbirth, melanoma, scleroderma, rheumatoid arthritis, and capsular contracture. Saline implants were more likely to rupture in the short term.
When Silicone Implants Leak
In a study of women with silicone breast implants, it was found that when the implants leaked, women were more likely to develop fibromyalgia, Hashimoto’s Disease, polymyositis, mixed connective tissue disease, and pulmonary fibrosis.
While the studies are pointing to an association between implants and the development of autoimmune disease, we do not have strong enough evidence at this time to definitely say that breast implants cause autoimmunity.
What Is BIA-ALCL?
BIA-ALCL (Breast Implant-Associated Anaplastic Large Cell Lymphoma) is a type of non-Hodgkin’s lymphoma (a cancer of the immune system). It is not breast cancer.
In 2011, it was discovered that there could be a link between breast implants (specifically textured implants, the type with a rough surface that minimizes migration and repositioning within the breast pocket) and the development of Anaplastic Large Cell Lymphoma. Typically, BIA-ALCL occurs only near the breast implant and surrounding scar tissue, but it has been known to spread throughout the body.
The chances of a person with breast implants developing BIA-ALCL are between 1 in 3,000 and 1 in 30,000. The disease most commonly occurs approximately a decade after the implant.
What Causes BIA-ALCL?
BIA-ALCL occurs only in women with breast implants. It also seems to be more likely to occur in women who have textured implants (as opposed to smooth implants). Currently, there are no confirmed cases of smooth only implant BIA-ALCL.
The causes of BIA-ALCL are still unknown, and more research is needed to determine what causes it. Some experts suggest that since textured implants have a greater surface area, there is a higher likelihood that the surgery will introduce bacteria, resulting in inflammation and disease. Others think the scar tissue that forms around an implant might be to blame, while some believe there is also a genetic component.
According to board certified plastic surgeon Dr. Anthony Youn, BIA-ALCL could have an infectious component to it, possibly chronic lymphocyte (white blood cell) proliferation and activation due to the development of biofilm.
Is There a Treatment for BIA-ALCL?
Doctors have successfully treated BIA-AL-CL by removing the implant and surrounding scar tissue, along with chemotherapy and radiation. Chemo and radiation may not be needed in the early stages of disease.
Does Breast Implant Illness Go Away?
Dr. Youn has seen mixed results in his medical practice when women have decided to have their breast implants removed due to symptoms associated with breast implant illness.
“Of those patients who’ve had them removed due to concerns that they were causing symptoms or autoimmune disease, unfortunately most of those with autoimmune disease don’t appear to have improved. I would love to say that they get better, but it hasn’t been my experience. They may say they feel somewhat improved, but I have rarely seen a complete resolution of their autoimmune disease. However, most of them with symptoms, but not true diagnoses of autoimmune disease, appear to resolve significantly. I have recently had two patients with these types of symptoms resolve completely after their implants were removed.”
Dr. Anthony Youn
I asked Krista whether her symptoms have resolved since explant surgery, and she told me that she has experienced almost complete symptom resolution following removal. Her IBS-D completely resolved, she got her period back (it disappeared for three years), her gut health and metabolism are back to normal, no more brain fog, and her lymph node swelling went down.
Will Having Implants Removed Make Symptoms Go Away?
While Dr. Youn has seen mixed results regarding the resolution of symptoms with the removal of implants, he does feel that any patient requesting their implants be removed should have their wishes honored.
“Whenever a patient asks me to remove her implants, whether she has symptoms of BII or not, the answer is always yes. I fully believe that the decision to have implants should be made by the woman with the implants, and no one else.”
Dr. Anthony Youn
How Is Breast Implant Illness Treated?
Explant surgery is currently the primary treatment for breast implant illness. For Krista, deciding to remove her implants was a difficult decision, because she had always dreamed of having large breasts. However, after learning that other women felt so much better after removing their implants, she hoped that it would make her feel better.
I also recommend women work with a naturopathic physician or licensed functional medicine provider to address their individualized health needs. We understand there is a strong connection between hormones and autoimmune disease, which is why it is important to address both as part of a holistic treatment plan. While we know that explant surgery may not be enough to resolve symptoms, there are additional steps you can take to reclaim your health.
What Is Explant Surgery?
Explant surgery involves the removal of breast implants. During explant surgery, the surgeon might also remove silicone from implant leaks, and the breast capsule – the scar tissue that forms after implants are inserted into the body.
Implant leaks do not always occur, nor does scar tissue always need to be removed. However, both can occur, and are also possible reasons for women to have their implants removed.
Explant Surgery Cost
According to the American Society of Plastic Surgeons, the average cost of explant surgery in 2019 was $2,641. Keep in mind that this fee does not cover anesthesia, medication prescriptions, hospital fees, tests, or X-rays. These can add up quickly, and turn into quite a substantial sum.
If you are considering explant surgery to remove your breast implants, it is essential to discuss all fees with your surgeon.
Another vital factor to consider is insurance. Unfortunately, many insurance companies will not cover implant removal surgery, unless it is medically necessary (e.g., ruptured implants or severe capsular contracture). Be sure to check with your provider to avoid any surprise expenses.
A word of caution in the world of plastic surgery, if the price of surgery seems to be too good to be true, it probably is. If you’re exploring explant surgery, it is advised that you work with a board certified plastic surgeon. Don’t be afraid to ask in depth questions about their experience, training, and how the surgery will be performed.
What to Do If You Can't Get Your Breast Implants Out Right Now
If your insurance provider will not cover your breast explant surgery cost, and it is not something you can afford out-of-pocket at the moment, you might start to feel stuck in a hopeless situation.
While there is no way to eliminate the symptoms of breast implant illness without implant removal, reducing your overall inflammation might help with symptom management.
One effective way to reduce inflammation is through nutrition, lifestyle, and supplementation under your healthcare provider’s supervision. This is to help mitigate symptoms and is not a treatment or cure for BII.
Nutrition to Help Breast Implant Illness Syndrome
Adopting a whole-foods eating plan to nourish your body and optimize hormones may help support you through this time and can be beneficial when undergoing surgery.
To the best of your ability, fill your plate with fresh, colorful vegetables, grass-fed or pasture-raised meat, wild-caught fatty fish, and healthy carbs. Aim to include anti-inflammatory omega-3 rich foods like walnuts, chia seeds, flax seeds, and cold water fish. Cooking with herbs or drinking teas that include ginger or turmeric can also provide anti-inflammatory benefits. Healthy fats, nutrient dense foods, and fiber rich plants can support your hormones and overall health. If you’re looking on how to get started, grab our free recipe guide and meal plan to learn how to build a hormone-loving diet.
Supplements Support for Breast Implant Illness Syndrome
It is always best to check with your provider about supplements specific to your needs. This is a good list to speak with them about.
Some of the best anti-inflammatory supplements supported by science are:
- NAC (N-Acetylcysteine). NAC has been known to reduce oxidative stress and inflammation, enhance immune function, and also support those with autoimmune diseases. Check out Dr. Brighten N-Acetyl-Cysteine (NAC) HERE.
- Turmeric (Curcumin). Curcumin (a compound found in turmeric) may help calm inflammation without the side effects of conventional anti-inflammatory drugs. Keep in mind that dietary turmeric should be combined with a little bit of fat (e.g., coconut oil) and black pepper to increase its absorption. View Dr. Brighten Turmeric Boost HERE.
- Omega-3 fatty acids. The proper omega-3 to omega-6 ratio may help quiet inflammation, and omega-3 fatty acids are necessary for many body processes anyway. We have to get our omega-3s through diet or supplementation. Unfortunately, the standard western diet is lacking in omega-3s and is much higher in omega-6 fatty acids. Try Dr. Brighten Omega Plus HERE.
- Adaptogenic Herbs. The adrenal glands produce cortisol in response to inflammation. This is a crucial hormone in controlling inflammation and is important in overall hormone balance. Adaptogenic herbs can help support optimal adrenal function. Learn more about our Adrenal Support HERE.
- Vitamin D. This vitamin has been shown to be essential in proper immune system function. Because of this, it may also influence inflammation. Check out our Vitamin D HERE.
Will diet and supplementation get rid of breast implant illness? No. But these tools can help you manage your symptoms if you are unable to have explant surgery right now.
How Can You Prevent Breast Implant Illness?
This is one of those times when the saying “prevention is better than cure” is pretty apt. The best way to avoid breast implant illness is not to get breast implants.
If you already have implants, there is no surefire way to avoid breast implant illness. Now, this does not mean that you will definitely feel sick someday as a result of your implants. Many women have no issues with their breast implants.
And it is your body. You know I am not about telling women what they should or should not do with their bodies, so if you want to get implants, then I encourage you to make an educated decision so you can feel confident in what is best for you.
If you are considering breast implants, ask questions. Do your research. Make sure you know all the possible side effects and future implications breast implants could have. Give your plastic surgeon a thorough health history. Try to find a surgeon who has dealt with or believes in breast implant illness, so that if you discover, down the road, that you are suffering from symptoms that may be linked to your implants, you already have a doctor in mind who can assist you.
