The postpartum time is a tumultuous period for women’s hormones, to say the least. You just grew a tiny human, which consumed a lot of your body’s resources. As you heal from delivery and begin nursing, the demands are even higher. Mix in the stress of adjusting to a new routine, having little time for yourself, and sleep deprivation, and you have a recipe for a postpartum hormone roller coaster.
This article will dive into all the details you need to know to support hormonal health during this exciting yet challenging time.
In this article
I will cover these most-asked questions:
- Does breastfeeding cause hormonal imbalance?
- How do hormones change postpartum?
- When do hormones return to normal?
- When do periods return postpartum?
- What are postpartum hormone imbalance symptoms?
- What nutrients do breastfeeding mothers need?
- How to balance hormones while breastfeeding
Does Breastfeeding Cause Hormonal Imbalance?
While your hormone profile during postpartum and while breastfeeding may be different from the rest of your childbearing years, the shift is normal. Breastfeeding is a natural state and requires certain hormones to adjust so that you can produce milk for your baby.
It’s not a defect that you need to correct — nutritional support is a good move, but most of the time breastfeeding hormones do not require medical intervention. Still, you may feel the effects. Symptoms like mood changes, night sweats, and breast tenderness may arise after you give birth until your body settles in. ,
Breast milk production is nutrient and energy intense. It requires a lot from your body, impacting the nutrients available for other things, like hormones. In addition, postpartum hormone changes are dramatic, impacting how you feel. Supporting your body with a high-quality prenatal vitamin can help.
How Hormones Change Postpartum
During pregnancy, many hormones are elevated to support the pregnancy but rapidly fall after the baby is born. Other hormones rise after birth to promote bonding and breastfeeding. These quick changes may lead to the baby blues, characterized by a low mood or mood swings in the weeks following delivery.
The baby blues, also called maternity blues or postnatal blues, affects between 13 and 76% of new moms1, depending on culture, geography, and other factors. These emotional changes are typically transient and resolve quickly.
If you find that these emotional changes are too much to handle or if you are thinking of harming yourself or your baby, call your doctor immediately.
During postpartum time and breastfeeding, women are also vulnerable to perinatal mood disorders, including perinatal depression (aka postpartum depression). Perinatal mood disorders affect about 10-20% of postpartum women2 and have many root causes, including lack of sleep3, hormone changes4, and more.
Let’s take a look at specific hormones while breastfeeding and how they contribute to symptoms or possible imbalances.

Sex Hormones
Sex hormones, especially estrogen and progesterone, play a critical role during pregnancy, supporting physical changes, growth and development, placental health, and more. These hormones are essential for healthy menstrual cycles and pregnancy but tend to stay low during breastfeeding.
During early breastfeeding and for some amount of time, you won’t be menstruating and ovulating, which means much less progesterone production. Ovulation is required prior to progesterone production at pre-pregnancy levels.
Estrogen and Progesterone
During pregnancy, estrogen and progesterone are at an all-time high, but immediately after the baby and placenta are delivered, levels rapidly drop to low levels like those in menopause.
Symptoms of low estrogen include:
- Vaginal dryness
- Depression
- Fatigue
- Brain fog
- Hot flashes
- Postpartum hair loss
Symptoms of low or no progesterone include:
- PMS
- Anxiety
- Sleep disruption
- Estrogen dominance
It’s natural and necessary to have low estrogen and progesterone while nursing. Some women may experience more symptomatic effects than others and benefit from supporting these hormones.
Oxytocin and Prolactin
While estrogen and progesterone plummet, the breastfeeding hormones (oxytocin and prolactin) rise.
During labor, oxytocin promotes uterine contractions, and contractions cause more release of oxytocin. After delivery, oxytocin levels remain high to promote bonding and caretaking.
Breastfeeding induces oxytocin release from the brain, which signals the breasts to release milk. Oxytocin levels remain high with baby suckling and then fall when not nursing. Higher oxytocin means higher prolactin and lower cortisol5.
Prolactin is the other essential hormone released during breastfeeding. It’s produced by the placenta6 and brain, remaining elevated after delivery. High prolactin suppresses the menstrual cycle by keeping estrogen and progesterone low and stimulates breast milk production.
Thyroid Hormones
Because of changes in the immune system that occur with pregnancy, along with the influence of estrogen and other hormones on thyroid health, women are more vulnerable to thyroid imbalances during postpartum and breastfeeding.
T3, T4, and TSH
Thyroid health tests7 (T3, T4, TSH, thyroid antibodies) are recommended around 6 to 12 weeks postpartum for those with Hashimoto’s thyroiditis, Graves’ disease, or another autoimmune disease, along with women using thyroid hormone replacement. Women with symptoms of thyroid imbalances should also be tested, even if outside of this early postpartum window.
Postpartum Thyroiditis
Postpartum thyroiditis is a specific thyroid disorder occurring in the postpartum period. It primarily resembles hyperthyroidism, or overactive thyroid, followed by symptoms of hypothyroidism or under-active thyroid. Some women will only experience hypothyroid symptoms.
Postpartum thyroiditis is challenging to distinguish from other thyroid conditions, hormone imbalances, and symptoms new mothers experience, like sleep deprivation and stress. It can occur up to one year after delivery8, which is a time when many women aren’t regularly seeing their healthcare provider like they were during pregnancy.
To learn more about postpartum thyroiditis and what to look for, read this article.
Adrenal Hormones
Adrenal health is another area greatly affected by the postpartum period. Low sleep, new routines, the nutrition demands of breastfeeding, going back to work, lack of a community to help with the baby, and other life factors increase stress for new moms. More stress means more cortisol.
Cortisol
Cortisol is one of the main adrenal hormones. It has a natural rhythm where it’s high in the morning and drops at night to promote sleep. Cortisol also spikes in response to acute stress, and chronic stress can lead to HPA-axis dysfunction. Clinically, I’ve seen this a lot in postpartum women.
A literature review9 looked at cortisol levels in postpartum women, finding that high cortisol is associated with transient depression, while low cortisol levels correlate with chronic postpartum depression. If you’re experiencing sadness or mood changes, let your doctor know so that depression, existing or emerging, can be addressed.

Insulin and Blood Sugar Balance
Insulin is another postpartum hormone to watch. Insulin plays a primary role in blood sugar regulation by helping move glucose from the blood into the cells for energy.
During breastfeeding, women become temporarily insulin resistant10, which supports producing high-calorie breastmilk. Low estrogen contributes to insulin resistance.
Insulin resistance may be an issue for some women during breastfeeding in terms of weight and metabolic health, especially in the context of a standard American processed food diet and those with diabetes or who had gestational diabetes.
When Do Hormones Return to Normal?
When is it normal for your period to return? Some women will get their period back in the first few months, and others won’t have a period for as long as they are breastfeeding. Most women will fall somewhere in between, which is completely normal.
Often the menstrual cycle returns when there is a reduction in nursing. Less suckling means prolactin reduces, which allows estrogen levels to rise and kickstart ovulation. Examples include night weaning or adjusting feedings to return to work.
What happens to your hormones when you stop breastfeeding? If your cycle doesn’t return while nursing, when you stop breastfeeding, you can expect sex hormones to rise and your period may return soon. It often takes a few cycles for hormones to regulate to pre-pregnancy levels.
Postpartum Hormone Imbalance Symptoms
Some symptoms like the baby blues are a normal response to the rapid and profound hormone changes you experience after having a baby. If symptoms are severe, persistent, and impact your daily life, please speak with your doctor. Even mild symptoms that are concerning are worth a conversation with your doctor.
Hormone imbalance symptoms to watch for postpartum include:
- Anxiety and depression
- Anger or irritability
- Insomnia
- Fatigue
- Loss of interest in favorite things
- Decreased ability to take care of your baby
- Rapid weight loss
- Weight gain
- PMS-type symptoms
- Vaginal dryness
Some doctors will recommend the birth control pill to manage postpartum symptoms, but there are also other options. Check out my article on Birth Control While Breastfeeding and my first book, Healing Your Body Naturally After Childbirth..
What Nutrients Do Breastfeeding Mothers Need?
A foundation for hormone balance while breastfeeding is solid nutrition. Eating a nutrient-dense diet and appropriate supplementation helps ensure you have the nutrition you need for balanced hormones and breast milk production.
Check out my free nutrition guide, with 7 days of hormone-balancing recipes, for added nutritional support on your breastfeeding journey!
Omega-3s
Getting omega-3 fats in the diet is essential for pregnancy and lactation. They promote neurodevelopment in the baby11 and help prevent postpartum depression12 for the mother.
Try getting three servings of low-mercury fish such as wild salmon, mackerel, and sardines each week. In addition, continue taking your omega-3 supplement while breastfeeding.
Iron
Iron is a critical nutrient during pregnancy13 to support blood volume expansion and fetal growth and development. Many women don’t get enough iron during pregnancy. Then, because of blood loss during delivery, breastfeeding mothers are at risk of iron-deficiency anemia too.
Continue to eat iron-rich foods, including grass-fed beef, shellfish, legumes, and leafy greens. Continue taking your prenatal vitamin to replenish iron levels during the postpartum period. Note that not much iron passes through breast milk, so this nutrient is all for you!
Vitamin D3
Vitamin D is another nutrient to have your eye on while breastfeeding. You need to be getting enough for your own needs and to pass through the breastmilk to your baby while exclusively breastfeeding, although you can supplement your infant directly14 as well. You’ll likely need 6000IU per day or more from a combination of your prenatal vitamin and additional vitamin D3 supplementation, depending on blood test results.
How to Balance Hormones While Breastfeeding
Let’s consider additional ways to promote postpartum hormone balance, including exercise, blood sugar balance, and supplements.
Exercise
Once you are cleared for exercise at your 6- or 8-week postnatal checkup, begin moderate exercise for its positive effects on your mood, hormones, metabolism, and more. Be careful not to push exercise too much, especially if sleep is poor, because it may add more stress, increase cortisol, and contribute to hormone imbalances instead of helping balance them.
Nutrient-Dense Diet
I’ve talked about the importance of a nutrient-dense diet to meet the high demands of breastfeeding. In addition, be sure to eat enough overall food in a way that balances blood sugar. Balancing blood sugar will help to support healthy hormone levels.
Balance hormones by including protein, healthy fats, and fiber-rich carbs at each meal. Snack as needed (and you’ll need to!) with nutrient-dense options. Grab my free hormone-balancing meal plan for added support
Prenatal and Postnatal Supplements
Just because pregnancy is over doesn’t mean it’s time to stop your prenatal supplements. In fact, your prenatal vitamin and other supplements are just as crucial after pregnancy as they were before.
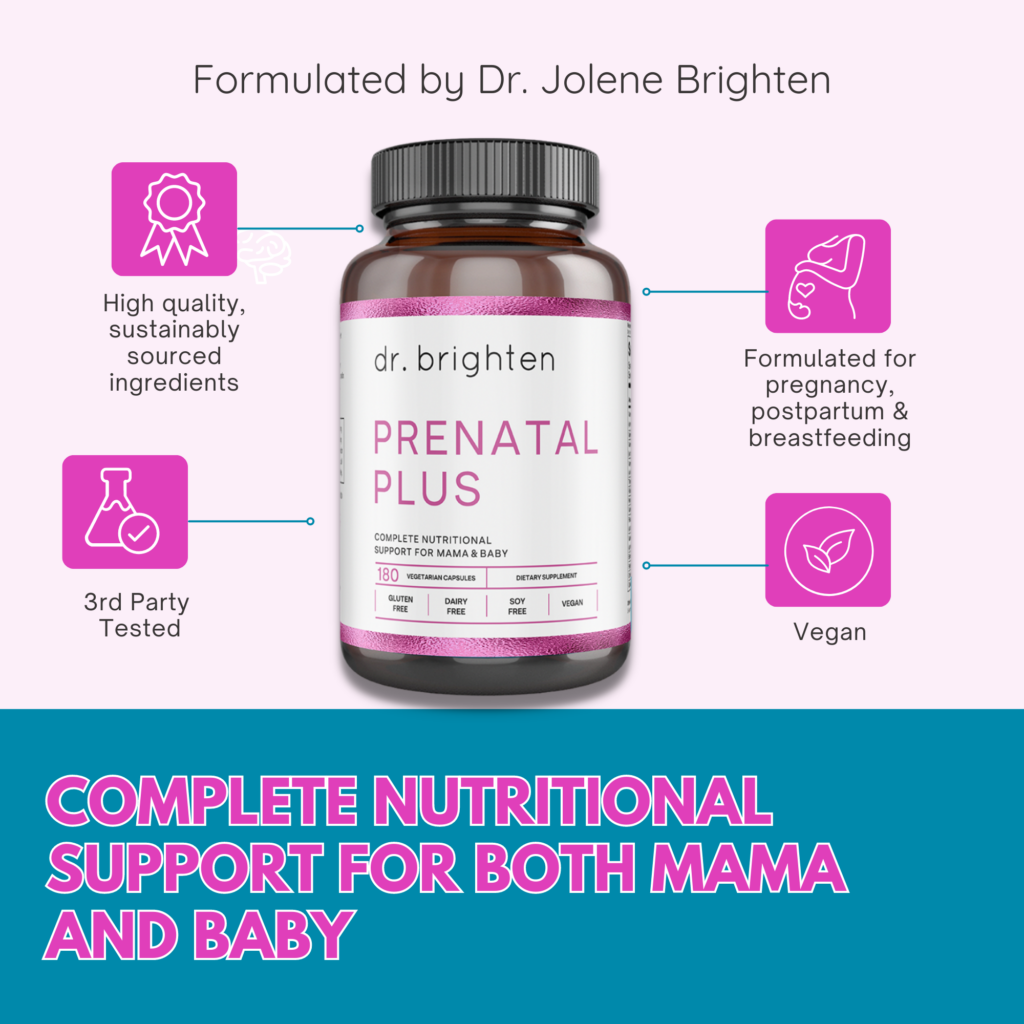
My Pregnancy Support Kit is designed to carry you from pregnancy and through your postpartum and breastfeeding journey. It includes Prenatal Plus, Omega Plus, and Women’s Probiotic to fill in dietary gaps and support healing from labor and breast milk production.
If you are looking for how to balance your hormones while breastfeeding, get back to the basics. Prioritize nourishing food, gentle movement, sleep (as you are able), and foundational supplements to support your own health and the health of your newborn. And most of all, be gentle with yourself while you enjoy the journey of motherhood.
References
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9863514/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/32357982/ ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1160560/ ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7794990/ ↩︎
- https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0235806 ↩︎
- https://pubmed.ncbi.nlm.nih.gov/35545690/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/35181848/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/34983968/ ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4886446/ ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7372076/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/34383914/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/32898343/ ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7492370/ ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8910000/ ↩︎
