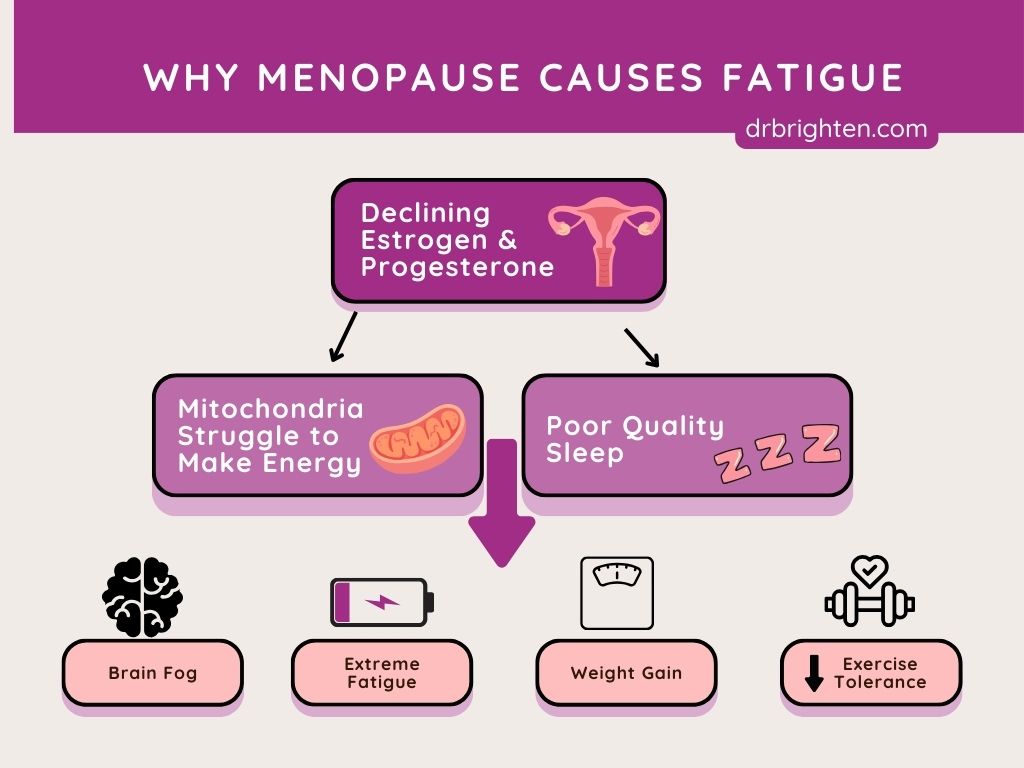
We often think of menopause as a hormone story, and it certainly is. But there’s another side of the equation that gets far less attention: your mitochondria, and more specifically, how they change as you enter perimenopause and get older.
Mitochondria, which are tiny “energy factories” inside your cells, are intricately connected to hormone production, brain function, metabolic health, and how energized or exhausted you feel each day.
When hormone levels fluctuate during perimenopause and menopause, mitochondrial health is often impacted too. This can set off a chain reaction of symptoms like fatigue, brain fog, weight gain, and more.
In this article, we’ll explore why so many women feel tired during menopause, how mitochondria play a role, and what you can do to support your cellular energy from the inside out.
Quick Summary:
- 85% of women report fatigue in menopause.
- Estrogen decline = weaker mitochondria = less energy.
- Common symptoms: brain fog, mood swings, weight gain, sleep issues.
- Solutions: nutrient support (saffron, bacopa, citicoline, zinc), strength training, sleep, blood sugar balance, toxin reduction.
In this article:
- Why Menopause Causes Fatigue (And Why It Feels So Extreme)
- When Does Menopause Fatigue Start? Early Signs in Your 40s
- The Hidden Role of Mitochondria in Menopause Fatigue
- How Estrogen Fuels Your Energy and What Happens When It Drops
- Brain Fog, Low Mood, and Menopause Fatigue: The Mitochondria Connection
- The Best Nutrients and Supplements to Beat Menopause Fatigue
- Lifestyle Strategies to Restore Energy in Menopause
- HRT and Mitochondrial Support
- Comparing Treatments for Menopause Fatigue and Mitochondrial Support
- How long does menopause fatigue last?
- FAQs: How to Fix Menopause Fatigue Naturally
Why Menopause Causes Fatigue (And Why It Feels So Extreme)
If you feel like you can’t keep up with your “old self” during perimenopause and menopause, you're on to something…
“Fatigue with menopause,” “low energy in menopause,” and even “extreme fatigue with menopause” are among the most common complaints about menopause symptoms that I hear from women in their 40s and 50s.
According to the Study of Women’s Health Across the Nation1 (SWAN), about 85% of women report fatigue as a symptom during perimenopause and menopause.
Another survey found that about 70% of women aged 40–65 experience daytime fatigue2, which was strongly correlated with both sleep disturbances and hormonal shifts. Many also report dealing with depression3, which is linked to low energy.
Why is exhaustion such an issue during menopause? Hormonal changes, especially declining estrogen levels, directly affect how your body produces and uses energy.
Why Your Cells Struggle to Make Energy:
- Poor mitochondrial function
- Increased oxidative stress
- Reduced glucose utilization
- Slower metabolism
- Sleep disturbances
- Mood and cognitive changes
Combined with the daily demands of life, these changes can make you feel like you’re basically running on empty and struggling to keep up with all that life is likely throwing your way.
Related:
Connection Between Gut Health, Menopause, and Perimenopause
When Does Menopause Fatigue Start? Early Signs in Your 40s
The average age of menopause is 51, but symptoms of perimenopause often begin in the late 30s to early 40s.
Research from SWAN shows that hormonal fluctuations usually begin several years before your final menstrual period, and those changes can affect your energy long before you realize you’re in perimenopause.
This transition isn’t linear, and some women experience “crashes” of fatigue as their hormones swing up and down. While there’s no universal timeline, it’s common to notice symptoms such as low energy, sleepiness, or exhaustion even in your early 40s.
Related:
When Does Perimenopause Start and How Long Does It Last?
7 Causes of Early Menopause + 5 Ways to Eliminate Symptoms
The Hidden Role of Mitochondria in Menopause Fatigue
Mitochondria are often called the “powerhouses” of your cells. That’s because they’re responsible for producing adenosine triphosphate (or ATP), which is the energy currency your body uses for everything from thinking and moving to hormone production and immune response.
In fact, mitochondrial health affects nearly every system in your body. The top five functions of mitochondria include:
- Generating cellular energy (ATP)
- Regulating cell survival and death
- Supporting hormone biosynthesis
- Managing cellular signaling and immune function
- Controlling oxidative stress and detoxification
As you age, mitochondria naturally decline in number and efficiency, a process known as mitochondrial aging.
Estrogen helps to protect and maintain healthy mitochondria, which helps explain why fatigue and metabolism shift so dramatically in menopause, when estrogen drops.
How Estrogen Fuels Your Energy and What Happens When It Drops
Estrogen is more than a reproductive hormone. It directly influences mitochondrial function, as well as cognitive function and more, in several important ways.
Estrogen normally helps:
- Increase the number of mitochondria in cells (mitochondrial biogenesis)
- Enhance energy production by upregulating genes involved in ATP generation
- Reduce oxidative stress by improving mitochondrial antioxidant defenses
- Promote mitochondrial repair and resilience
This means that when estrogen begins to decline, your mitochondria may struggle to keep up, especially in energy-demanding tissues like the brain, muscles, and ovaries.
Signs of Low Estrogen Fatigue in Menopause:
- Menopause tiredness symptoms, like struggling through work, feeling overwhelmed easily, and not being as productive as you once were
- Exercise intolerance
- Sleep disturbances
- Brain fog and memory issues
- Hormone production imbalances, which can lead to other symptoms like mood swings, low sex drive, irritability, and more
Unfortunately, if you're in menopause and feeling wiped, you're essentially experiencing a vicious cycle: less estrogen weakens mitochondria, and weaker mitochondria make it harder to produce the hormones and neurotransmitters your body needs.
Related:
The Medical System Is Misleading Women About Symptoms of Menopause with Dr. Tara Scott
How Hormones and Menopause Affect ADHD: What No One’s Telling You with Dr. Jolene Brighten

Brain Fog, Low Mood, and Menopause Fatigue: The Mitochondria Connection
Your brain consumes about 20% of your body’s total energy4, making it especially sensitive to mitochondrial decline.
For example, the hypothalamus, a region of the brain that regulates hormones, temperature, sleep, and metabolism, is highly vulnerable during the menopausal transition.
Studies show that low estrogen levels may alter mitochondrial dynamics in the brain, contributing to classic menopause symptoms like:
- Brain fog: Difficulty focusing, forgetfulness, and mental sluggishness that make everyday tasks and conversations feel harder to manage. Mitochondrial energy deficits in the brain may reduce clarity and processing speed.
- Anxiety or low mood: Increased worry, sadness, or emotional reactivity that can seem out of proportion or difficult to control. Estrogen normally supports neurotransmitter balance and mitochondrial function in mood-regulating areas of the brain, which explains why anxiety is more common during perimenopause.
- Hot flashes: Sudden, intense waves of heat often accompanied by sweating and flushing, caused in part by dysregulation in the hypothalamus.
- Sleep disturbances: Trouble falling asleep, staying asleep, or waking up too early, due to changes in the brain’s sleep-wake centers. For help getting better sleep during perimenopause, refer to: Why Can’t I Sleep? The Real Reasons for Perimenopause Sleep Issues (and What Actually Helps)
- Cognitive decline: A noticeable drop in memory, verbal fluency, or problem-solving skills. These symptoms are often subtle, but they can become more pronounced over time if mitochondrial resilience isn’t supported.
Recent studies, such as those published in Frontiers in Aging Neuroscience5 and Biology of Sex Differences6, have found that mitochondrial dysfunction in the hypothalamus may be one reason why women experience more neurodegenerative risk after menopause. For instance, an estimated 67% of adults with Alzheimer's disease are women7.
Fortunately, there are a number of ways you can help protect your mental clarity, mood, and focus while in menopause and afterwards.

The Best Nutrients and Supplements to Beat Menopause Fatigue
So how can you support your mitochondria and restore your energy in menopause?
Research shows that several nutrients and botanicals can help increase mitochondrial function, support resilience, and help combat the fatigue that so many women in midlife experience.
1.Saffron: Mood and Energy Support
Saffron is a traditional spice with potent antioxidant and neuroprotective properties. Clinical studies show saffron can:
- Improve mood8 and energy
- Reduce symptoms of depression9 and anxiety
- Enhance mitochondrial function in brain cells
- Combat oxidative stress and inflammation
- Support metabolic health
A 12-week clinical trial10 found that a standardized saffron extract (called affron®), taken twice daily, significantly reduced feelings of anxiety and depression in perimenopausal women.
Participants who took saffron reported a 33% drop in anxiety and a 32% drop in depression scores compared to those who took a placebo. Saffron was found to be well-tolerated and showed strong benefits for mood and emotional well-being.
2. Bacopa: Brain and Memory Boost
Bacopa is an adaptogenic herb that contributes to overall balance and is known to support memory and brain health, including by supporting key brain structures and synaptic function. It's especially helpful if you’re experiencing brain fog, forgetfulness, or low motivation during menopause. It's been shown to help:
- Protect mitochondrial membranes
- Improve learning and memory11
- Reduce cortisol and stress-related fatigue
- Increase ATP production in brain tissue
In a small 12-week study12 of adults over age 55, researchers found that Bacopa monnieri combined with weekly cognitive training led to higher accuracy on memory tasks. Brain scans also showed changes that were potentially thought to reflect increased brain network complexity and efficiency.
3.Citicoline: Cellular Energy Recharge
Citicoline (CDP-choline) is a naturally occurring compound that supports brain energy metabolism. If you feel mentally drained or unfocused, citicoline may help recharge your brain from the cellular level up. Studies suggest it:
- Enhances mitochondrial efficiency in neurons
- Increases phospholipid production for healthy brain cell membranes
- Improves focus, mental clarity, and memory13
- May delay cognitive aging
According to one review14, citicoline helps make phosphatidylcholine, a key building block of brain cell membranes. Research shows it may protect brain cells and reduce inflammation, especially in cases of stroke, brain injury, glaucoma, and memory loss.
Citicoline has been shown to work by strengthening cell membranes, reducing damaging glutamate levels, limiting oxidative stress, and calming overactive immune responses in the brain. Clinical studies suggest it may help improve recovery and protect against cognitive decline.
4. Zinc: Hormone and Mitochondria Protection
Iron and zinc are vital minerals for brain and emotional health, especially in premenopausal women. Zinc is involved in mitochondrial enzyme activity and protects against oxidative damage. Low zinc levels are common in women with fatigue15, hormonal imbalances, or chronic stress.
Zinc can also help:
- Support healthy thyroid and adrenal function, which is important for energy balance and mood support
- Help regulate estrogen and progesterone balance
- Strengthen immune response
- Assist in detoxification and DNA repair, which contributes to overall brain health
One review16 looked at 11 clinical studies and found that iron supplementation improved memory and thinking skills, even in women without full-blown anemia.
Seven studies showed better mood, focus, and cognitive performance after increasing iron levels. Zinc also showed promise in reducing symptoms of depression, both on its own and when added to antidepressant therapy. Overall, improving iron and zinc levels may support emotional and mental clarity.
Nutrients That Support Energy and Mood in Menopause
| Supplement / Nutrient | How It Helps |
| Saffron | Supports mood, reduces oxidative stress17 |
| Bacopa | Improves memory18 & supports ATP production through lowering oxidative stress19 |
| Citicoline | Enhances brain energy metabolism |
| Zinc | Regulates hormones & mitochondrial enzymes, supports healthy energy20 |
| Rhodiola | Improves stress resilience21, alleviate fatigue22, may improve memory23 |

Lifestyle Strategies to Restore Energy in Menopause
Alongside targeted supplements, these evidence-based strategies can support mitochondrial health and help restore your energy:
1.Eat More Polyphenols to Boost Energy
Colorful plant foods are rich in polyphenols, compounds that protect mitochondria from oxidative damage and inflammation.
Dr. Kara Fitzgerald’s study24 found that a polyphenol-rich diet could reverse biological age by over 3 years in just 8 weeks, in part by optimizing cellular health. This style of eating also helps manage blood sugar and can help reduce menopause belly fat, two key challenges during the perimenopause transition.
Top polyphenol foods include:
- Berries
- Pomegranate
- Dark leafy greens
- Herbs and spices (like turmeric and oregano)
- Cocoa/dark chocolate
- Nuts and seeds
- Green tea
- Dark chocolate
- Olive oil
2. Balance Blood Sugar for Steady Energy
Stable blood sugar supports mitochondrial function and reduces energy crashes. Aim to:
- Eat protein and fiber with every meal, including 30 grams with breakfast and ideally about 100 grams per day
- Limit ultra-processed carbs and added sugars
- Include healthy fats to stay full and energized
3. Strength Training Builds More Mitochondria
Muscle tissue is metabolically active and contains a high number of mitochondria. Strength training can help improve mitochondrial density, support estrogen metabolism, and boost fat-burning, all of which benefit women over 40.
Depending on what you enjoy, try:
- Resistance band workouts, which are joint-friendly
- Pilates, which focuses on core strength, muscle control, and flexibility
- Kettlebell training, which combines strength and cardio
- High-intensity interval training (HIIT) involving short bursts of resistance-based cardio
- Functional strength movements like squats, lunges, and step-ups
4. Sleep Is When Your Mitochondria Repair
Sleep is when your body repairs and regenerates mitochondria. Poor sleep disrupts hormonal balance, increases oxidative stress, and worsens fatigue. Try:
- Getting to bed by 10 PM
- Sticking to a consistent sleep-wake schedule, even on weekends, to regulate your circadian rhythm
- Limiting screens before bed
- Taking magnesium, such as Magnesium Plus, or adaptogens (like ashwagandha, lemon balm, and valerian, which are found in my Adrenal Calm formula) to calm your nervous system
Related: The Best Herbs for Menopause and Understanding Magnesium for Menopause: Your Comprehensive Guide
5. Reduce Toxins to Protect Energy
Environmental toxins can impair mitochondrial function and contribute to estrogen imbalance. Support detoxification and lower your exposure by:
- Using clean personal care and home products, specifically those that do not include parabens, phthalates, synthetic fragrances, formaldehyde-releasing preservatives, or harsh cleaning agents. These endocrine-disrupting chemicals can interfere with estrogen receptors and place extra stress on your mitochondria.
- Filtering your water to remove heavy metals, pesticides, and pharmaceuticals that may affect hormonal and mitochondrial health.
- Eating organic produce when possible, especially from the Environmental Working Group’s “Dirty Dozen” list25, to reduce pesticide intake that can tax your detox systems.
- Sweating regularly through exercise or sauna therapy, which helps eliminate fat-soluble toxins and supports mitochondrial biogenesis.
- Supporting your liver and gut with cruciferous vegetables (like broccoli and arugula), fiber-rich foods, and targeted nutrients like calcium-D-glucarate and milk thistle, which aid in hormone detox and mitochondrial resilience.

HRT and Mitochondrial Support
When it comes to tackling menopause fatigue, hormone replacement therapy (HRT) can play an important role. Estrogen directly supports mitochondrial biogenesis, energy production, and antioxidant defenses. Restoring estrogen through HRT may help improve fatigue, cognitive clarity, and metabolic function in women who are good candidates. Research suggests that timely use of HRT, ideally within 10 years of menopause onset, can better protect mitochondria and reduce long-term risks such as neurodegeneration.
That said, not every woman can or wants to use HRT. This is where mitochondrial and adrenal support strategies make a powerful difference. Nutrients like saffron, bacopa, citicoline, zinc, and magnesium directly enhance mitochondrial efficiency, while adaptogens such as rhodiola, ashwagandha, and eleuthero strengthen adrenal resilience and reduce the “wired but tired” feeling so common in midlife.
For many women, the best results come from a combined approach:
- HRT (when appropriate and supervised by a provider) to restore estrogen’s mitochondrial protection.
- Targeted supplementation (e.g., Dr. Brighten Essentials Radiant Mind, Adrenal Support, and Magnesium Plus) to fortify cellular energy, mood, and sleep.
- Lifestyle strategies like strength training, blood sugar balance, and stress reduction to give mitochondria the best environment to thrive.
Together, these approaches create a synergistic effect, helping women move from chronic exhaustion to renewed vitality in menopause.
Comparing Treatments for Menopause Fatigue and Mitochondrial Support
| Approach | How It Works | Benefits | Considerations | Support Options |
| Hormone Replacement Therapy (HRT) | Restores estrogen, which directly supports mitochondrial biogenesis, energy production, and antioxidant defenses. | Improves fatigue, brain fog, mood, and metabolic function. May protect long-term brain and cardiovascular health if started within 10 years of menopause. | Not suitable for all women. Requires medical supervision and personalized dosing. | Bioidentical estrogen, progesterone, testosterone as prescribed by a provider. |
| Targeted Supplements | Provide nutrients and adaptogens that enhance mitochondrial efficiency, reduce oxidative stress, and support adrenal resilience. | Steadier energy, better mood, improved sleep, and stress tolerance. | Results build over time. Works best when paired with a healthy lifestyle. | Radiant Mind (saffron, bacopa, citicoline, zinc), Adrenal Support (rhodiola, eleuthero, B5, ashwagandha), Magnesium Plus (for sleep and mitochondrial repair). |
| Lifestyle Strategies | Improve mitochondrial density and lower stress burden through daily habits. | Long-term foundation for energy, hormone balance, and healthy aging. | Requires consistency. May take time to notice full benefits. | Strength training, blood sugar balance, polyphenol-rich diet, sleep hygiene, toxin reduction. |
How long does menopause fatigue last?
Menopause fatigue doesn’t have a one-size-fits-all timeline. For many women, fatigue begins in perimenopause (often in the early 40s) as estrogen and progesterone fluctuate. Symptoms may come and go in waves during this transition, lasting several years before and after the final menstrual period.
Once hormones stabilize in postmenopause, some women notice their energy gradually improves. However, fatigue can persist if underlying issues—like mitochondrial decline, blood sugar imbalance, poor sleep, thyroid changes, or adrenal stress—aren’t addressed.
The good news is that menopause fatigue is not permanent. By supporting your mitochondria, balancing hormones, strengthening adrenal function, and addressing lifestyle triggers, you can restore steady energy at any age. Many women find that with the right plan—including targeted nutrients, adaptogens, and sleep support—they feel more energized in midlife than they did in their 30s.
FAQs: How to Fix Menopause Fatigue Naturally
Menopause can absolutely cause extreme tiredness due to factors like hormonal fluctuations, poor mitochondrial function, disrupted sleep, and increased stress response.
Studies show that fatigue, poor energy, and increased sleepiness are some of the most reported symptoms during the menopausal transition. Menopause is unique for every woman, but there's a good chance you'll notice changes in your energy.
Extreme fatigue in menopause is most often caused by a combination of declining estrogen levels, disrupted sleep, slower mitochondrial function, and increased oxidative stress. As estrogen drops, your mitochondria—the energy powerhouses of your cells—don’t produce energy as efficiently, leading to exhaustion, brain fog, and low mood. Blood sugar swings, thyroid changes, and stress can make menopause fatigue feel even worse.
Natural strategies can go a long way in restoring energy during menopause. These include:
– Balancing blood sugar with high-protein meals (at least 30 grams per meal).
– Strength training to build muscle and boost mitochondrial density.
– Prioritizing sleep and supporting circadian rhythm with magnesium or calming adaptogens.
– Reducing toxin exposure to lessen the burden on your mitochondria.
– Targeted supplementation such as saffron, bacopa, citicoline, and zinc—nutrients shown to support mood, cognition, and mitochondrial energy.
Many of these evidence-based nutrients are available in my formulas like Radiant Mind (with saffron, bacopa, citicoline, and zinc) and Adrenal Calm (with magnesium and adaptogens that improve sleep and stress resilience).
For many women, menopause fatigue improves once hormones stabilize after the transition. However, it doesn’t always disappear on its own. Supporting mitochondrial function, addressing nutrient deficiencies, and optimizing lifestyle factors can make fatigue much less disruptive—and in many cases, women feel more energized than they have in years once their systems are supported.
Several nutrients and botanicals have been studied for their role in combating menopause fatigue:
– Saffron: supports mood, resilience, and mitochondrial function.
– Bacopa: improves memory, stress adaptation, and energy production in the brain.
– Citicoline: recharges brain cell membranes and boosts focus.
– Zinc: supports hormone balance and mitochondrial enzymes.
– Magnesium: calms the nervous system and improves sleep quality.
– Rhodiola & Eleuthero: adaptogens that enhance stress tolerance, reduce burnout, and improve stamina.
– Ashwagandha: helps regulate cortisol, calm anxiety, and support restorative sleep.
– Vitamin B5 (Pantothenic Acid): essential for adrenal hormone production and energy metabolism.
These are key ingredients in Radiant Mind and Magnesium Plus, designed to target the root causes of fatigue, brain fog, and mood swings in menopause. Together, these nutrients not only help your cells produce more energy but also strengthen your adrenal glands, which are under extra demand during menopause. Supporting adrenal health can reduce that “wired but tired” feeling, improve resilience to stress, and restore steady energy.
Many of these adaptogens and nutrients are found in Adrenal Support and Adrenal Calm from Dr. Brighten Essentials—formulas designed to nourish the stress response, balance cortisol, and reduce fatigue in midlife women.
Yes. Hormone replacement therapy (HRT) can help reduce fatigue in menopause by restoring estrogen, which protects mitochondrial function, supports neurotransmitters, and improves sleep. Not every woman is a candidate for HRT, but when used appropriately and monitored by a healthcare provider, it can be an effective tool for energy, mood, and cognitive support. For women who cannot or choose not to use HRT, nutrient and lifestyle support (like supplements, strength training, and blood sugar balance) are powerful alternatives.
Focus on mitochondrial support:
– Eat a hormone-supportive diet (high in protein, healthy fats, fiber, and lower in added sugar and refined carbs)
– Get regular movement, especially resistance training
– Support your sleep and circadian rhythm
– Remove processed foods and toxic chemicals from your diet and lifestyle
– Consider taking supplements like saffron, bacopa, citicoline, zinc, magnesium, omega-3s, and ashwagandha
– Work with a provider to assess your hormone levels and deficiencies
Related: HRT for Menopause & Perimenopause: Benefits, Side Effects & Menopause Solutions with Dr. Amy Killen
If you're struggling with stubborn weight during perimenopause, it's likely because metabolic and hormonal shifts can slow your metabolism, drain your energy, and make it harder to lose fat, especially around the belly.
That’s I created the free Perimenopause Weight Loss Action Plan—a doctor-designed strategy that supports your metabolism, hormones, and mitochondria (your body’s energy engines).
Inside the plan, you’ll get:
– A 7-day anti-inflammatory meal plan to stabilize blood sugar and reduce bloat
– High-protein, fiber-rich recipes to curb cravings and nourish your hormones
– Daily strength & movement guides to boost mitochondrial density and fat-burning
– A supplement guide to support energy, mood, and restful sleep
– And stress and sleep strategies to lower cortisol and rev up your metabolism
You can download your free action plan here.
Key Takeaways: You Can Overcome Menopause Fatigue
- Mitochondrial dysfunction is a key driver of menopause lack of energy, but it’s not the end of the story.
- While there is a deep connection between estrogen and your cellular powerhouses, you can take action to support your energy, brain, and metabolism at any age.
- If you’re feeling tired from menopause or wondering how to improve mitochondrial function, this is your invitation to dig deeper, not just into your hormones, but into the health of every single cell in your body.
References
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3185243/ ↩︎
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9381266/ ↩︎
- https://pmc.ncbi.nlm.nih.gov/articles/PMC9178181/ ↩︎
- https://pmc.ncbi.nlm.nih.gov/articles/PMC2816633/ ↩︎
- https://pmc.ncbi.nlm.nih.gov/articles/PMC5934418/ ↩︎
- https://pmc.ncbi.nlm.nih.gov/articles/PMC11587679/ ↩︎
- https://pmc.ncbi.nlm.nih.gov/articles/PMC3970844/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/29332222/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/37264347/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/34463070/ ↩︎
- https://www.ncbi.nlm.nih.gov/books/NBK589635/ ↩︎
- https://pmc.ncbi.nlm.nih.gov/articles/PMC7937913/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/33978188/ ↩︎
- https://faseb.onlinelibrary.wiley.com/doi/10.1096/fj.202400823R ↩︎
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8133867/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/25405366/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/29332222/ ↩︎
- https://www.gavinpublishers.com/article/view/effect-of-bacopa-monnieri-extract-on-memory-and--cognitive-skills-in-adult-humans-a-randomized-double-blind-placebo-controlled-study ↩︎
- https://www.jsirjournal.com/Vol2Issue402.pdf ↩︎
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8133867 ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5370380/ ↩︎
- https://karger.com/cmr/article/24/1/46/67709/Rhodiola-rosea-in-Subjects-with-Prolonged-or ↩︎
- https://pmc.ncbi.nlm.nih.gov/articles/PMC6288277/ ↩︎
- https://pubmed.ncbi.nlm.nih.gov/36947707/ ↩︎
- https://www.ewg.org/foodnews/?gad_source=1&gad_campaignid=43684673&gbraid=0AAAAAD_iHo67Ppr2-auxfiHO_LZIceAhj&gclid=Cj0KCQjw5JXFBhCrARIsAL1ckPtHkO-vnhuTInrk3sLI46-hWgUfaJhp6gshliCrpnFQa4QB-CWRMZwaAsLkEALw_wcB ↩︎


