Autoimmune Progesterone Dermatitis (APD)—also known as progestogen hypersensitivity—is a rare immune-mediated reaction in which the body mounts an allergic or autoimmune response to endogenous progesterone or synthetic progestins, leading to cyclical skin and systemic symptoms that worsen during the luteal phase of the menstrual cycle.
What's unique about APD compared to other types of dermatitis is that it's cyclical, with symptoms typically worsening during the luteal phase of the menstrual cycle (the second half of the cycle after ovulation occurs). Most often, symptoms are the worst just before menstruation begins. That's because APD is due to progesterone hypersensitivity—and progesterone is highest before a woman's period starts.
In this article, I'll answer the questions: what does autoimmune progesterone dermatitis look like, why does it occur, and what treatments are available? I'll also address whether it's safe to get pregnant with autoimmune progesterone dermatitis and if this condition is connected to fertility treatments like IVF.
In this article:
- Autoimmune Progesterone Dermatitis: Quick Overview
- Autoimmune Progesterone Dermatitis Symptoms
- How APD Differs From PMDD or Other Hormonal Skin Conditions
- How Is Autoimmune Progesterone Dermatitis Diagnosed?
- APD Causes and Risk Factors
- The Role of Histamine and Mast Cells in Autoimmune Progesterone Dermatitis
- Autoimmune Progesterone Dermatitis Treatments
- Autoimmune Progesterone Dermatitis and IVF
- Progesterone Hypersensitivity and Pregnancy
- Key Takeaways on Autoimmune Progesterone Dermatitis
- Frequently Asked Questions About Progestogen Hypersensitivity
Autoimmune Progesterone Dermatitis: Quick Overview
- Rare immune reaction to progesterone or synthetic progestins
- Symptoms flare during the luteal phase when progesterone peaks
- Common symptoms include hives, itching, angioedema, and asthma-like reactions
- Diagnosis is clinical and based on hormone timing and response to progesterone withdrawal
- Treatment may include antihistamines, diet changes, hormone suppression, or desensitization
- Pregnancy and IVF are possible with specialized care
Autoimmune Progesterone Dermatitis Symptoms
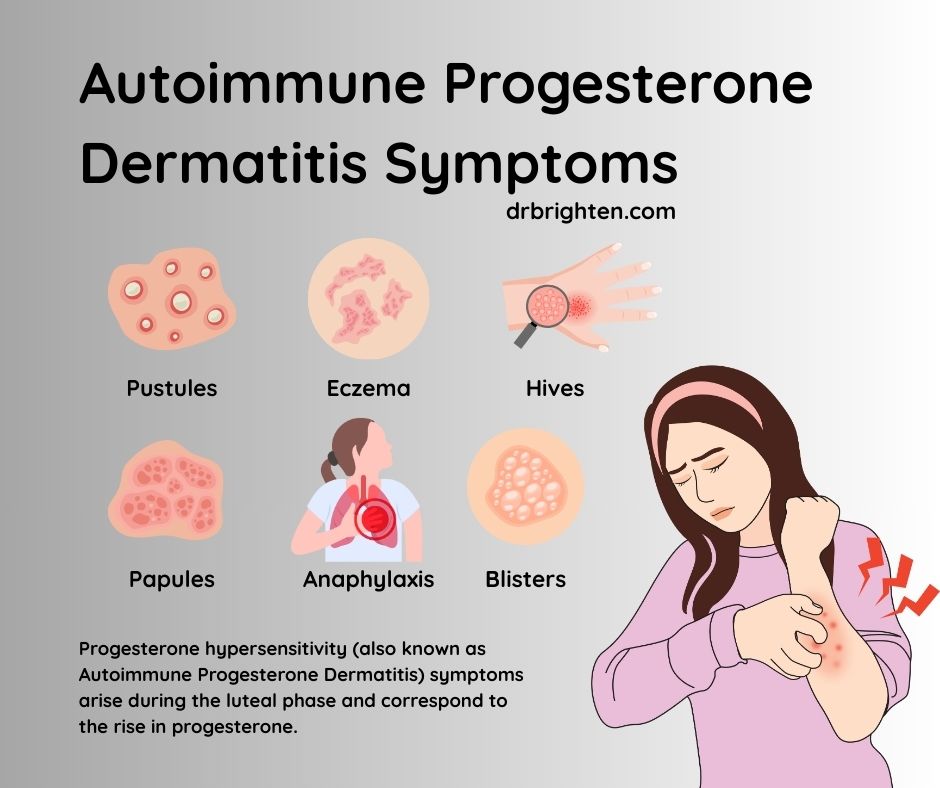
Rashes associated with APD vary significantly in appearance depending on exactly how sensitive someone is to progesterone. Some people develop small, itchy bumps, while others experience widespread hives or even eczema-like patches.
APD is sometimes described as autoimmune and sometimes as allergic because it shares features of both. While it involves immune misrecognition of progesterone, many reactions are mediated through mast cells and histamine rather than classic autoantibodies.
These skin changes seen with APD are notably tied to the menstrual cycle, typically worsening in the five to seven days leading up to menstruation when progesterone levels are high.
Symptoms of autoimmune progesterone dermatitis1 can range from mild cyclical rashes to severe systemic allergic reactions.
Common Skin Symptoms
- Urticaria (hives)
- Eczematous rashes
- Papules or pustules
- Angioedema
Systemic or Severe Symptoms
- Asthma-like breathing difficulty
- Anaphylaxis2 (rare but documented)
- Worsening of pre-existing dermatologic conditions
How APD Differs From PMDD or Other Hormonal Skin Conditions
- APD involves immune activation, not neurotransmitter sensitivity
- Symptoms include hives, angioedema, or breathing symptoms (not typical of PMDD)
- APD resolves rapidly with progesterone withdrawal
- PMDD causes mood and cognitive symptoms, not immune-mediated skin reactions
- Histamine can be involved in both PMDD and APD
Related: Estrogen and Histamine

How Is Autoimmune Progesterone Dermatitis Diagnosed?
There is no single definitive test for autoimmune progesterone dermatitis (APD). Diagnosis is clinical and relies on recognizing a distinct hormonal pattern, supported by targeted testing and careful exclusion of other conditions. Key diagnostic elements include:
- Cyclical symptom pattern: Skin symptoms recur in a predictable, monthly pattern—most often flaring 5–7 days before menstruation and improving rapidly with the onset of menses, when progesterone levels fall.
- Clear correlation with the luteal phase: Symptoms consistently worsen during the luteal phase, when progesterone peaks, and are absent or significantly improved during the follicular phase when progesterone is low.
- Improvement with progesterone withdrawal or suppression: Resolution or marked improvement of symptoms after:
- Stopping progesterone containing medications
- Suppressing ovulation (and therefore progesterone production) This response strongly supports progesterone hypersensitivity.
- Intradermal progesterone testing (with important caveats): Some specialists use intradermal or skin-prick testing with progesterone to assess hypersensitivity. However:
- Results are not standardized
- False positives and false negatives can occur
- Testing carries a risk of severe allergic reaction, including anaphylaxis
For these reasons, it should only be performed by experienced allergy specialists and is not required for diagnosis.
- Exclusion of conditions that mimic APD: Several disorders can worsen premenstrually and must be ruled out, including:
- Chronic eczema or contact dermatitis
- Premenstrual flares of inflammatory skin conditions
- PMDD-related skin changes without immune involvement
- Mast cell activation disorders or systemic mastocytosis
- Drug reactions unrelated to hormonal timing
- Thorough medication and hormone exposure history: Identifying symptom onset after exposure to:
- Progestin-containing birth control
- Fertility medications
- Progesterone creams or suppositories can help distinguish exogenous from endogenous progesterone hypersensitivity.
Taken together, a reproducible hormone-linked pattern, improvement with progesterone withdrawal, and exclusion of other diagnoses form the cornerstone of APD diagnosis.
When to Suspect APD
APD should be suspected when:
- Skin symptoms recur monthly despite standard dermatologic treatment
- Symptoms reliably worsen before menstruation
- Reactions appear after starting progesterone or progestins
- Antihistamines provide partial but not complete relief
Related: Histamine Intolerance: What It Is & What to Do About It
APD Causes and Risk Factors
APD develops due to an autoimmune response to progesterone, though the exact mechanism of this hypersensitivity is not fully understood. Some describe it as a “progesterone allergy.”
There are two main types of APD3:
- Endogenous (from the inside): Symptoms occur during the luteal phase due to exposure to increased progesterone levels. Endogenous APD is considered an autoimmune condition because someone who has APD reacts to progesterone when their immune system mistakenly identifies progesterone—a hormone naturally produced by the body, with peak levels around day 21 of a 28-day menstrual cycle —as a harmful substance. Essentially, with APD, the body views its own hormone as a foreign invader, similar to how it might react to an allergen like pollen or certain foods. This immune response triggers a hypersensitivity or allergic reaction that then affects the skin.
- Exogenous (from the outside): Symptoms appear after exposure to synthetic progestins4, including those found in contraceptives like birth control pills or fertility medications.
APD is more likely to occur in women of reproductive age, especially those with a history of other autoimmune or allergic conditions. It can also emerge during times when progesterone levels are manipulated, such as during In Vitro Fertilization (IVF). This makes APD a concern for some women undergoing fertility treatments.
Related: Progesterone Side Effects & Intolerance: Why You Feel Worse on Progesterone| Dr. Jolene Brighten

The Role of Histamine and Mast Cells in Autoimmune Progesterone Dermatitis
A growing body of evidence suggests that mast cell activation and histamine release play a central role in the symptoms seen with autoimmune progesterone dermatitis (APD). In susceptible individuals, progesterone—whether produced by the body or introduced synthetically—can trigger mast cell degranulation, a process in which immune cells release inflammatory mediators, most notably histamine.
When mast cells are activated in response to progesterone, the resulting histamine surge helps explain many of the hallmark features of APD, including:
- Hives (urticaria) caused by histamine-induced blood vessel dilation
- Intense itching (pruritus) driven by histamine signaling in the skin
- Angioedema, or deeper swelling beneath the skin and mucous membranes
- Asthma-like symptoms or shortness of breath, due to histamine’s effects on airway smooth muscle
This mast cell–histamine connection also clarifies why treatments that target allergic pathways are often effective in APD, even though progesterone is a hormone rather than a classic allergen.
Specifically, it explains why:
- Antihistamines can significantly reduce skin and respiratory symptoms by blocking histamine receptors
- Low-histamine diets may lessen symptom severity by reducing overall histamine burden in the body
- Vitamin C and quercetin can be supportive, as both help stabilize mast cells and improve histamine breakdown, thereby dampening the inflammatory response associated with progesterone hypersensitivity
- N-Acetyl Cysteine (NAC) supports glutathione production and inflammatory regulation, which may further help reduce the downstream effects of mast cell activation when used alongside antihistamines and dietary strategies.
Understanding APD through the lens of mast cell activation and histamine intolerance bridges the gap between conventional allergy management and supportive nutritional strategies. This framework also reinforces why supplements aimed at histamine regulation are best viewed as adjunctive support, not alternative therapy, alongside appropriate medical care.
Related: Progesterone Intolerance: Symptoms, Causes & What To Do About It
Autoimmune Progesterone Dermatitis Treatments
When it comes to treating APD, several options are available depending on the severity of symptoms and whether it's caused by medications. Treatments range from natural remedies, including dietary changes, to pharmaceutical interventions and, in some cases, desensitization protocols that help “train” the body to react less to progesterone.
There are 7 key areas that need to be considered for autoimmune progesterone dermatitis treatment:
- Stopping or changing progesterone exposure
- Antihistamines
- Dietary strategies
- Steroids (short-term)
- Hormone suppressants
- Desensitization protocols
- Supportive supplements
Stopping or Changing Progesterone Medications
Synthetic progestogens, often found in contraceptives5 or fertility treatments, can trigger APD symptoms. If one of these medications is the cause of APD, it should no longer be taken to help manage symptoms. Some synthetic progestins that may cause symptoms6 include:
- Oral contraceptive pills
- Long-acting progestin injections
- Contraceptive vaginal rings
- Progestin-containing IUDs
- High-dose progesterone used in IVF treatments
- Certain corticosteroids, due to their similarity to progesterone
If you've recently started taking contraceptives and are noticing changes in your skin, discuss alternatives with your provider, such as combination birth control pills, that may be able to help manage your symptoms better.
In some cases, women undergoing IVF who have APD may experience heightened symptoms due to the surge in hormone levels. Treatment protocols during IVF may involve the use of antihistamines, corticosteroids, or progesterone desensitization methods to help manage reactions. It's important for women with APD to work closely with their healthcare provider during IVF to mitigate symptoms while ensuring a healthy pregnancy.
Antihistamines
A common first-line treatment includes antihistamines7, which block histamine—a chemical that triggers allergic reactions in the body. By inhibiting the effects of histamine, antihistamines help reduce discomfort and inflammation caused by APD.
During the luteal phase, particularly 5-7 days before menstruation, antihistamines like loratadine and famotidine can be effective in managing the histamine reaction that contributes to skin irritation and rashes.
Loratadine is preferred over Benadryl (an over-the-counter) antihistamine due to less risk of side effects. For example, it can help provide relief without causing lots of drowsiness or other common antihistamine side effects.
Dietary Changes and Foods to Avoid
Diet changes can play a role in managing APD symptoms by limiting histamine reactions8 and inflammation. Foods that are known to trigger histamine release or are high in histamines should be avoided. Autoimmune progesterone dermatitis foods to avoid include:
- Alcohol
- Processed meats
- Certain aged cheeses
- Foods with artificial colors and flavoring
- Night-shade vegetables (like eggplant, tomatoes, and potatoes, depending on the person)
- For some people, eggs, some canned fish, shellfish, and certain fruits and nuts (what may cause allergies)
When managing APD, focus on consuming nutrient-rich foods that support the immune system and skin health, such as fresh fruits, vegetables, nuts, seeds, lean meats, legumes, and other non-processed foods. If you're having trouble determining which foods cause you allergic reactions, it's best to work with an allergist or dietician.
Desensitization Protocols
Desensitization protocols involve gradually exposing the body to increasing amounts of progesterone to build up tolerance and decrease sensitivity9. This method has shown promise in reducing the severity of APD symptoms10 over time. It's often considered for those who experience significant disruption to their quality of life due to APD.
In one study11, up to 90% of patients experienced improvements in their skin reactions and other symptoms after undergoing desensitization.
Desensitization protocols typically take weeks or even months, depending on the patient’s response and the severity of their condition. Successful desensitization can lead to a significant reduction or complete resolution of symptoms, including skin rashes, itching, and other allergic responses to progesterone.
In some cases, long-term maintenance doses of progesterone might be required to prevent the return of hypersensitivity. It's important to note that this treatment must be administered and monitored by a healthcare professional experienced in allergy and hormone disorders to ensure safety and effectiveness, especially if performed during pregnancy.
Steroids
In more severe cases of APD, steroids (or corticosteroids) can be prescribed to manage acute APD flare-ups. These work by reducing inflammation, but they're typically only used when symptoms are very bothersome.
Corticosteroids, such as oral or injectable forms, can alleviate skin swelling and itching, but they won't address the underlying cause of progesterone hypersensitivity or offer a long-term solution.
Hormone Suppressants
Hormone-suppressing medications may be considered to reduce how much progesterone the body makes. One option is to prevent ovulation entirely, which halts the production of progesterone.
Leuprolide acetate12 (sold under the brand name Lurpon and Eligard, among others) is a commonly used medication for this purpose, although it's typically only used in extreme cases where other treatments fail. It works by stopping ovulation and reducing the surge of progesterone that occurs after an egg is released, which then decreases symptoms of APD.
It's important to note that Leuprolide acetate can have significant side effects, such as bone density loss, mood changes, and menopause-like symptoms, which must be carefully weighed against its benefits.
Overall, hormone management may be necessary in some cases for long-term relief, but it's best to discuss this option carefully with a knowledgeable practitioner since it also has drawbacks.
Natural Options, Including Supplements
Several supplements, such as vitamin C and quercetin, can help support the body’s ability to process histamine more effectively. Supplements do not treat progesterone hypersensitivity itself, but may help reduce histamine burden and symptom severity when used alongside medical management.
NAC for Histamine Intolerance, Mast Cell Activation, and Hormone-Related Inflammation
N-acetylcysteine (NAC) is a precursor to glutathione, one of the body’s most important antioxidants involved in immune regulation and detoxification. While NAC does not treat progesterone hypersensitivity itself, it may help reduce inflammatory burden and oxidative stress associated with immune activation in autoimmune progesterone dermatitis (APD).
NAC may be supportive in APD by:
- Helping replenish glutathione, which plays a role in regulating immune responses
- Reducing oxidative stress that can worsen mast cell activation and inflammation
- Supporting overall inflammatory balance, particularly during hormonally driven immune flares
Some research also suggests NAC may influence mast cell–mediated pathways indirectly13, which may be relevant in conditions where histamine release contributes to symptoms.
Recommended dosage: 600–1,200 mg daily, often divided into two doses. NAC is typically best tolerated when taken away from food, unless gastrointestinal sensitivity occurs.
Clinicians may recommend NAC as part of a broader histamine- and inflammation-support protocol; for example, Dr. Brighten Essentials NAC is formulated to support glutathione production without unnecessary additives.
As with other supplements, NAC should be used as a supportive strategy alongside medical care, particularly for individuals managing complex immune or hormone-related conditions.
Vitamin C
Vitamin C is a powerful antioxidant that can help lower histamine levels in the body14. It has been shown to support immune function and reduce inflammation, which is helpful in managing allergic reactions. By breaking down histamine, vitamin C can ease the symptoms of progesterone hypersensitivity, such as rashes, itching, and swelling.
Recommended dosage: 500-1,000 mg daily. Split doses can be helpful, as large amounts of vitamin C can sometimes cause gastrointestinal discomfort.
Quercetin
Quercetin is a natural plant pigment found in foods like apples and onions. It is a potent antioxidant with anti-inflammatory properties and has been shown to inhibit the release of histamine15 from immune cells, making it a natural antihistamine. Quercetin can help reduce allergic reactions and soothe symptoms like itching, hives, and skin irritation. It also works synergistically with vitamin C to further bolster histamine control and inflammation reduction.
Recommended dosage: 500 mg two times per day, ideally 30 minutes before meals. Quercetin is best taken with a meal that contains some fat for improved absorption.
Bromelain
An enzyme found in pineapple, bromelain works well with quercetin to reduce inflammation and allergic responses16. It can help decrease swelling, redness, and other inflammatory symptoms.
Recommended dosage: 500 mg two to three times daily between meals.
Probiotics
A healthy gut can improve your body’s immune response and histamine regulation. Probiotics help balance gut bacteria, which in turn may support a healthier immune system17 and reduce allergic symptoms.
Recommended dosage: Follow label instructions for a high-quality probiotic supplement, usually containing at least 10-20 billion CFUs daily (such as my Women's Probiotic).
While supplements do not treat the underlying immune mechanism of APD, they may support histamine regulation and inflammatory balance when used alongside medical care.
Autoimmune Progesterone Dermatitis and IVF
In Vitro Fertilization (IVF) can increase the risk of symptom flares in people with autoimmune progesterone dermatitis because fertility protocols often involve high-dose exogenous progesterone to support implantation and early pregnancy. For individuals with progesterone hypersensitivity, this sudden and sustained exposure can provoke significant immune reactions.
Why IVF increases APD risk
- IVF protocols commonly require progesterone injections, suppositories, or oral formulations at doses much higher than those produced during a natural cycle
- Exogenous progesterone bypasses the body’s normal regulatory mechanisms, increasing the likelihood of mast cell activation and histamine release
- Repeated exposure during fertility treatment may unmask previously undiagnosed APD or worsen existing symptoms
When progesterone desensitization is used
- Desensitization protocols may be recommended before or during IVF for individuals with known or suspected APD
- These protocols involve carefully supervised, incremental exposure to progesterone to reduce immune reactivity
- Desensitization is most often used when progesterone cannot be avoided, such as during luteal support or early pregnancy
Role of antihistamines and corticosteroids during IVF
- Antihistamines (such as H1 and H2 blockers) are commonly used to blunt histamine-mediated symptoms during progesterone exposure
- Short-term corticosteroids may be prescribed to control severe inflammatory or allergic reactions during treatment cycles
- These medications do not treat the underlying hypersensitivity but can help protect patient safety and treatment continuity
- In some cases, clinicians may also consider antioxidant support such as NAC to help manage inflammatory stress during fertility treatment or pregnancy, though this should always be individualized.
The importance of coordinated care
Managing APD during IVF requires collaboration between:
- A reproductive endocrinologist (REI) overseeing fertility treatment
- An allergist or immunologist experienced in hormone hypersensitivity
- In some cases, a dermatologist familiar with hormonally mediated skin disorders
This team-based approach allows fertility treatment to proceed while minimizing the risk of severe allergic reactions and improving overall outcomes.
Progesterone Hypersensitivity and Pregnancy
Yes—many women with autoimmune progesterone dermatitis can safely become pregnant with appropriate monitoring and treatment.
Pregnancy presents a unique challenge in APD because progesterone levels rise steadily and remain elevated throughout gestation. For some individuals, this prolonged exposure can trigger symptoms, while for others, pregnancy may actually lead to symptom improvement due to immune system modulation.
How pregnancy affects APD symptoms
- Some women experience worsening skin or allergic symptoms, particularly early in pregnancy
- Others report symptom improvement or complete remission, possibly due to gradual progesterone increases and immune tolerance
- In some cases, APD may first appear during pregnancy or after childbirth, potentially due to immune sensitization during gestation
Management during pregnancy
- Antihistamines are often used to control histamine-mediated symptoms and are commonly part of pregnancy-safe treatment plans
- Progesterone desensitization may be considered before conception or early in pregnancy for those with severe reactions
- Close monitoring allows clinicians to balance symptom control with fetal safety
Postpartum considerations
- Symptoms may recur or worsen after delivery, when progesterone levels drop rapidly
- Ongoing follow-up is important to manage postpartum flares and guide future family planning
With individualized care and proactive planning, many people with autoimmune progesterone dermatitis are able to conceive, maintain pregnancy, and deliver safely.
Key Takeaways on Autoimmune Progesterone Dermatitis
- APD is a condition caused by hormonal sensitivity to progesterone that causes an immune response. It leads to skin reactions, including rashes, hives, and other symptoms.
- A progesterone allergy can be caused by a reaction to the body's hormone, or to synthetic progesterone found in birth control pills or fertility treatments.
- Both medical and natural approaches, including the use of antihistamines, steroids, medications, and desensitization protocols, can help to manage this condition and allow people with APD to lead more comfortable and less disruptive lives.
Frequently Asked Questions About Progestogen Hypersensitivity
Yes. Autoimmune progesterone dermatitis (APD), also called progestogen hypersensitivity, is considered a rare condition, though experts believe it is underdiagnosed because symptoms often resemble eczema, chronic hives, PMDD-related flares, or unexplained allergic reactions.
APD shares features of both autoimmune and allergic conditions. While the immune system reacts abnormally to progesterone, many symptoms are driven by mast cell activation and histamine release rather than classic autoantibodies, which is why antihistamines are often effective.
NAC does not treat progesterone hypersensitivity itself, but it may help reduce inflammatory and oxidative stress that can worsen histamine-driven symptoms. Some clinicians include NAC—such as Dr. Brighten Essentials NAC—as part of a broader supportive protocol
Yes. Progestin-containing birth control methods—including pills, injections, hormonal IUDs, and vaginal rings—can trigger or worsen APD symptoms, particularly in people with exogenous progesterone hypersensitivity. Symptoms may improve after stopping these medications.
In many cases, yes. Because progesterone production declines after menopause, APD symptoms often improve or resolve completely. However, symptoms can persist if progesterone-containing hormone therapy is used.
APD is usually manageable, but severe cases can be serious, especially if symptoms include angioedema, breathing difficulty, or anaphylaxis. Anyone with systemic or respiratory symptoms should be evaluated promptly and managed by experienced clinicians.
APD does not directly cause infertility, but it can complicate fertility treatment. IVF protocols that require high-dose progesterone may trigger symptoms, which is why coordinated care and, in some cases, progesterone desensitization are used.
Although both conditions worsen before menstruation, PMDD is driven by brain sensitivity to hormonal shifts, while APD involves an immune reaction to progesterone. APD commonly causes hives, swelling, or allergic-type symptoms, which are not typical of PMDD.
There is no single cure, but symptoms can often be well controlled. Management may include antihistamines, dietary strategies, hormone suppression, or progesterone desensitization, depending on severity and reproductive goals.
References
- https://rarediseases.org/rare-diseases/progestogen-hypersensitivity/ ↩︎
- https://www.jpagonline.org/article/S1083-3188(18)30093-7/abstract ↩︎
- https://rarediseases.org/rare-diseases/progestogen-hypersensitivity/ ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10481886/ ↩︎
- https://onlinelibrary.wiley.com/doi/10.1111/ajd.12529 ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10481886/ ↩︎
- https://www.spandidos-publications.com/10.3892/etm.2018.7055 ↩︎
- https://www.hopkinsmedicine.org/-/media/johns-hopkins-childrens-center/documents/specialties/adolescent-medicine/cfs-low-histamine-diet.pdf ↩︎
- https://www.annallergy.org/article/S1081-1206(18)31360-7/fulltext ↩︎
- https://pubmed.ncbi.nlm.nih.gov/27090357/ ↩︎
- https://www.jaci-inpractice.org/article/S2213-2198(16)30012-5/fulltext ↩︎
- https://medlineplus.gov/druginfo/meds/a685040.html ↩︎
- https://onlinelibrary.wiley.com/doi/10.1046/j.1365-2567.2000.00045.x ↩︎
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9970132/ ↩︎
- https://www.mountsinai.org/health-library/supplement/quercetin ↩︎
- https://pubmed.ncbi.nlm.nih.gov/38676413/ ↩︎
- https://www.jaci-inpractice.org/article/S2213-2198(22)00686-9/abstract ↩︎

